Chapter 155 Leukemias and Lymphomas
Introduction
Leukemias and lymphomas are myeloproliferative disorders that may affect the eye. The ophthalmic symptoms and findings can be the initial manifestation of the systemic illness. Indeed, before the use of bone marrow biopsy, the ophthalmologist was often called upon to assist with the diagnosis of the leukemias.1
Estimates of the frequency of intraocular involvement with leukemia range as high as 90% of cases.1 Although melanoma is the most common primary intraocular tumor in adults and retinoblastoma is the most common primary intraocular tumor in children, when secondary or metastatic neoplastic intraocular disease is considered, intraocular manifestations of hematological malignancies are found to be overwhelmingly more common since the prevalence of myeloproliferative disorders is higher in the general population.
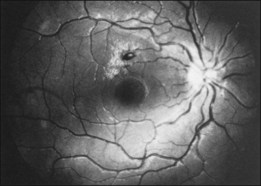
Liebreich first described leukemic retinopathy in the 1860s. Since that time, reports have documented that virtually all intraocular structures may be involved. Patients have been reported with leukemic infiltrates of the optic nerve, choroid, retina, iris, ciliary body, and anterior chamber. A child with a leukemic hypopyon is illustrated in Figure 155.1. Central serous chorioretinopathy overlying areas of choroidal infiltration has been reported, as has retinal vascular sheathing, subconjunctival hemorrhage, anterior chamber hemorrhage, intraretinal hemorrhage, and intravitreal hemorrhage.2 Retinal changes may be related to direct invasion of tissue by neoplastic cells, to manifestations of associated hematological abnormalities such as anemia, thrombocytopenia, or hyperviscosity states, to opportunistic infections, or to unrelated chance findings.
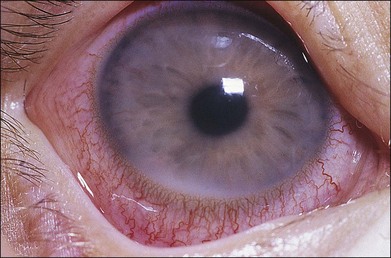
Fig. 155.1 Leukemic iris infiltration in a child with acute lymphocytic leukemia. Note hypopyon inferiorly.
Intraocular infiltrates appear to correlate with associated central nervous system (CNS) involvement and decreased survival. The intraocular manifestations of leukemia are protean, and clinically, it usually is not possible to differentiate the various leukemias and lymphomas on the sole basis of their ophthalmoscopic findings.3
Systemic classification of leukemia and lymphoma
At presentation, the acute leukemias most often have systemic manifestations of anemia, hemorrhage, infection or signs and symptoms related to infiltration of organs. Acute lymphocytic leukemia is the predominant leukemia type in children, and more than 50% of these patients can be cured. In adults, acute myelogenous leukemia is the predominant myeloproliferative disorder and survival rates are lower in adults than children.1
The chronic leukemias often first appear in an indolent manner. Symptoms may be vague. These diseases generally are found in older individuals. Although associated infections or other complications are often treated aggressively, many patients receive no treatment for their underlying disease because treatment has not definitely been shown to prolong survival. Some chronic leukemias degenerate into a “blast” (acute) phase, in which case the signs and symptoms resemble those of the acute leukemias.1
Leukemia
Prevalence and incidence
Scant data are available from prospective series of patients concerning ocular findings at the time of diagnosis.4,5 Even less information can be found about the frequency with which various intraocular manifestations are seen during the course of the illness. Most clinical series contain cross-sections of patients seen both early and late during the course of the illness. Autopsy series, which presumably show the highest prevalence rates, often overstate the frequency with which clinical disease is detected.
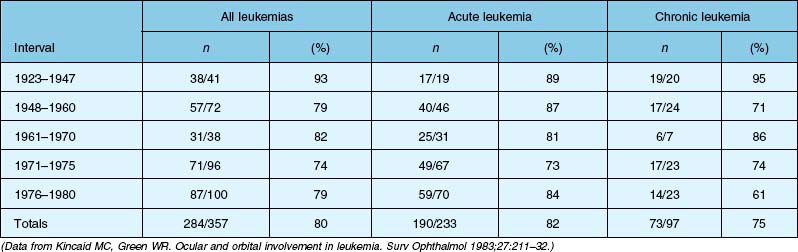
Four autopsy series have shown variable prevalence data. Allen and Straatsma3 found that 38 of 76 patients (50%) had ocular involvement by neoplastic disease or pathologic changes that could be directly ascribed to the neoplastic disease. Nelson et al.6 found that 33 of 117 patients (28%) with various types of leukemia had ocular metastases at the time of death. Leonardy et al.7 found leukemic infiltrates in the eyes of 42 of 135 patients (31.1%), with the choroid being the most frequently involved site. Data from Kincaid and Green1 are summarized in Table 155.1, which shows that 75% of patients with chronic leukemias, 82% of patients with acute leukemias, and 80% of affected patients in this study had intraocular involvement at the time of death.
Clinical series show highly variable prevalence rates. A small prospective series was reported by Karesh et al.,4 who examined the fundus findings in 56 newly diagnosed, untreated patients with acute myelogenous leukemia. They found retinopathy at the time of initial examination in 28 of 56 patients (50%) and no cases of leukemic infiltration. Schachat et al.5 reported on the largest series of patients with newly diagnosed leukemia examined within a few days of diagnosis. Among the 120 patients examined (65 with acute myelogenous leukemia, 51 with acute lymphocytic leukemia, and four with other leukemias), 62% had ocular abnormalities due to their underlying myeloproliferative disorder.
Clinical manifestations
Reddy et al. reported on 82 children examined after diagnosis of acute leukemia and before initiation of chemotherapy. Although only 4% of patients complained of visual symptoms, abnormal retinal findings were noted in 16% of all patients examined.8 Reddy and colleagues also reported on the ocular findings in 288 newly diagnosed cases of leukemia in adults and children. Clinical symptoms were present in 10%, but ocular findings were noted in 35.4%. Ocular findings were more common in adults (49%) than in children (16%), and were more frequent in myeloid leukemia (41%) compared with lymphoid leukemia (29.2%).9
Russo et al. evaluated 180 pediatric patients with acute leukemia and found ocular manifestations in 66% of children with acute myeloid leukemia and 11.5% of children with acute lymphocytic leukemia.10 Data from multiple reports suggest the need for routine ocular examination of all patients with newly diagnosed acute leukemia regardless of whether they are symptomatic or not. Other investigators have also noted that chronic lymphocytic leukemia appears to have a very low prevalence of ocular involvement and routine screening of these patients at the time of diagnosis does not appear to be necessary.11
In our series of 120 cases examined at the time of diagnosis, four patients (3%) had leukemic infiltrates. In addition, intraretinal hemorrhages were present in 29 cases (24%), white-centered retinal hemorrhages in 13 cases (11%), vitreous hemorrhage in three cases (2%), and cotton-wool spots in 19 cases (16%). Miscellaneous findings, presumably unrelated to leukemia, were present in 20% of cases.5 The low prevalence of leukemic infiltrates in our series differs from those reported in autopsy series. One potential reason for the lower prevalence is the ability to detect leukemic choroidal infiltrates, which are a frequent finding in autopsy series but are difficult to diagnose clinically.
Leukemic infiltrates
Retinal or preretinal infiltrates
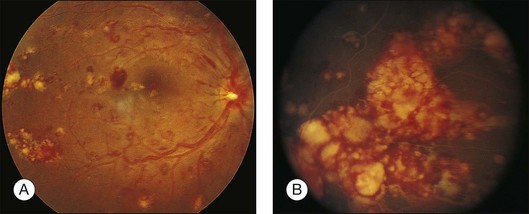
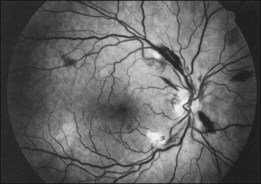
Leukemic infiltrates have been described by several investigators. Kuwabara and Aiello12 reported on a patient with chronic myelogenous leukemia with large gray-white nodules of varying sizes in the retina.12 They suggested that this finding was an ominous prognostic sign and, in general, associated with high blood counts, fulminant disease, and early demise.13 Merle and colleagues have described a subretinal infiltrate with venous vasculitis in a patient with adult T-cell leukemia.14 As the ocular lesions progressed, the general health of the patient declined despite treatment with chemotherapy. Another patient with leukemic infiltrates is illustrated in Figure 155.2. This type of pathologic change in the fundus was seen in 2–3% of patients in our prospective series.5 Optic nerve infiltration may be the initial ocular manifestation of acute leukemia and can result in severe vision loss if not treated.15
Gray-white streaks along vessels may be caused by local perivascular leukemic infiltrates. A case of diffuse unilateral retinal angiopathy that resembled frosted-branch angiitis that responded to local radiation and intrathecal chemotherapy was reported by Kim et al.16 This case represented the sole manifestation of relapsing acute lymphoblastic leukemia in an 18-year-old man and also involved optic nerve infiltration in the same eye.
Choroidal infiltrates
Leukemia may also infiltrate the choroid; however, clinical signs of choroidal involvement are often subtle unless overlying retinal or retinal pigment epithelial (RPE) changes bring them to attention. Serous retinal detachment overlying choroidal infiltrates17 or overlying frank choroidal masses18 is an important clue. Histopathologic confirmation of choroidal infiltration has been reported in a patient with adult T-cell leukemia.19
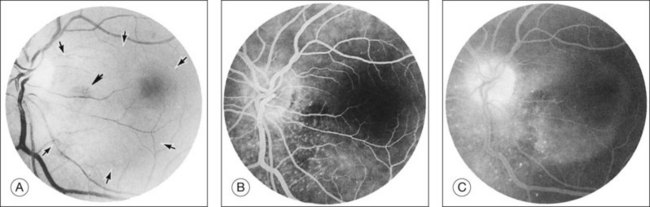
Kincaid et al.20 reported on a 71-year-old woman with an exudative retinal detachment, shifting subretinal fluid, and areas of diffuse pinpoint fluorescein hyperfluorescence with dye leakage into the subretinal space. The patient had a poorly characterized and unusual leukemia. Histopathologic study showed that the choroid was moderately distended by a diffuse cellular infiltrate with an overlying serous retinal detachment. The RPE showed areas of depigmentation and proliferation. There were a few small areas of associated pigment epithelial detachment.20 Gass21 described a patient with myelomonocytic leukemia who had a discrete choroidal mass with an overlying serous retinal detachment. Pinpoint hyperfluorescence was seen on the angiogram in areas overlying the mass (Fig. 155.3).
Burns et al.22 reported on a 37-year-old patient with acute lymphocytic leukemia who appeared to have “bilateral macular edema.” The patient was treated with ocular radiation on the assumption that underlying leukemic infiltration of the choroid was present, and this was confirmed at autopsy. Serous retinal detachment overlying areas of choroidal infiltration has been reported in patients with chronic lymphocytic leukemia, acute lymphocytic leukemia, chronic myelogenous leukemia, and acute myelogenous leukemia.1,23 Serous RPE detachment has also been reported in a patient with acute lymphoblastic leukemia.24 The serous retinal and RPE detachments can be the presenting manifestation of the leukemia.25 Eventually, as the fluid and detachment resolve, coarse clumping of the RPE is seen.17,24
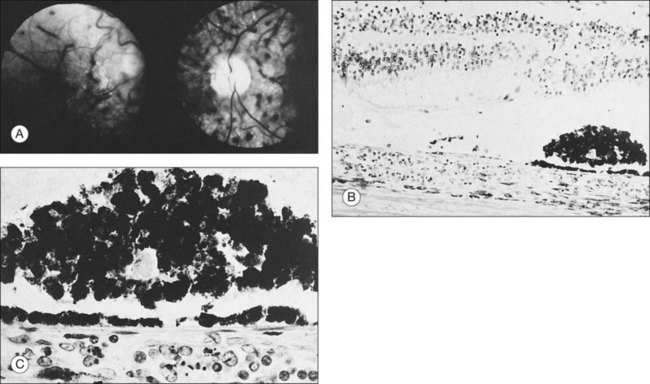
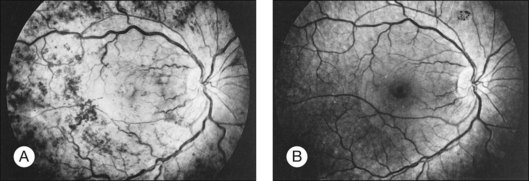
Prominent pigment epithelial changes also may be seen after resolution of what may be retinal infiltrates. Jakobiec and Behrens26 reported on a 3-year-old patient with acute leukemia who was found to have preretinal hemorrhages, some with white centers. A multitude of jet-black spots were seen, most prominently in the posterior pole. Soft white patches were described in the retinal periphery. The authors believed that these patches were the precursor lesions of the black spots. They postulated that the spots represented proliferation of pigment epithelial cells or small pigment epithelial detachments.26 Clayman et al.17 reported on a child with acute lymphocytic leukemia who had massive pigmentary changes simulating leopard spots, most marked in the posterior pole (Fig. 155.4). At autopsy, the retina and the choroid were infiltrated with atypical immature lymphocytes. Areas of RPE hyperplasia were present, including heaped-up masses of pigment epithelium surrounding leukemic cells.
Vitreous infiltrates
Vitreous opacities may be manifestations of an intraocular malignancy. Moribund patients may show massive collections of tumor cells in the vitreous, but most patients with intravitreal hemorrhage have neoplastic cells in the vitreous only because their peripheral blood contains tumor cells (Fig. 155.5). The cells do not appear to be preferentially replicating in the vitreous cavity. Swartz and Schumann2 described a patient with acute lymphocytic leukemia who had a dense vitreous cellular infiltration. Diagnostic vitreous aspiration confirmed the neoplastic nature of the process. Examination of the cerebrospinal fluid was also positive for blast cells. At the time, the peripheral blood was negative for tumor. The patient was treated with systemic and intrathecal chemotherapy and 1200 cGy of cranial radiation therapy. The vitreous cleared after the treatment.2
Belmont et al.27 reported on a 72-year-old patient with chronic unilateral uveitis. Leukemic cells were found in the iris and throughout the vitreous at the time of a pars plana vitrectomy performed to rule out reticulum cell sarcoma. Isolated ocular blast crisis with leukemic hypopyon has been reported to occur in chronic myelogenous leukemia.28 Vitreous cells and leukemic retinopathy have been reported in a single case of hairy cell leukemia (which constitutes less than 2% of adult leukemias).29 A masquerade syndrome with primarily ocular findings of panuveitis in a patient with T-cell prolymphocytic leukemia was reported by Dhar-Munshi et al.30 Additional cases of vitreous involvement in leukemia have been cited by Kincaid and Green1 as well as by Rothova et al.31 Leukemic cells have been found in the vitreous of patients with neovascularization of the disc. Delaney and Kinsella32 reported on a patient with chronic myelogenous leukemia and disc neovascularization who had good peripheral perfusion, although the macula did show areas of nonperfusion. de Juan et al.33 described a 3-year-old patient with acute lymphocytic leukemia who had disc neovascularization, vitreous hemorrhage, and vitreous infiltration. This case was unusual because neither the cell count nor the platelet count were remarkably elevated.
Hattenhauer and Pach34 reported a single case of ocular B-cell lymphoma occurring in a patient with chronic lymphocytic leukemia. The occurrence of diffuse large cell lymphoma in patients with chronic lymphocytic leukemia is known as Richter syndrome. Richter syndrome is estimated to occur in 3–10% of patients with chronic lymphocytic leukemia. It portends an abrupt deterioration in health and carries a poor prognosis for survival.
Possible leukemic infiltrates
Duane et al.35 reviewed the causes of white-centered retinal hemorrhages (Fig. 155.6) and also described possible pathophysiologic mechanisms. The authors suggested that these lesions should be classified as suspicious for direct intraocular manifestations of leukemia, since aggregates of leukocytes have been reported in the center of white-centered hemorrhages.36,37 However, it should be noted that white-centered retinal hemorrhages can be composed of fibrin-platelet aggregates and are not necessarily a definite sign of neoplasia.
Manifestations of anemia and thrombocytopenia
Leukemic retinopathy is the term most often used to denote the fundus manifestations of anemia, thrombocytopenia, and increased blood viscosity seen in patients with leukemia. In general, the term does not necessarily refer to frank leukemic proliferation. The changes of “leukemic retinopathy” may be more commonly seen with the acute leukemias, but the frequency with which they occur has not been adequately studied to be certain. Although perivascular sheathing may be due to actual perivascular infiltrates, tortuous dilation of the retinal veins probably is not. The veins and arteries may assume a yellowish tinge because of both anemia and leukocytosis.1 Retinal hemorrhages may occur, often at the posterior pole, and may be subretinal, deep retinal, superficial retinal, or preretinal, with potential breakthrough bleeding into the vitreous cavity. Hemorrhages may have a blot or blotch shape, flame shape, or they may have white centers (Figs 155.7, 155.8).35
Cotton-wool spots may be the presenting abnormality that precipitates the systemic evaluation leading to the diagnosis of leukemia.38 Cotton-wool spots may be caused by local factors, such as an abnormally large cell or a cluster of cells occluding retinal arterioles, and may not be related to the overall peripheral blood composition. In general, hematologic parameters are not associated with the presence of cotton-wool spots.39 Cotton-wool spots and hemorrhages can spontaneously resolve in patients with chronic leukemic disease.2
Manifestations of hyperviscosity
Whole-blood hyperviscosity may lead to veno-occlusive disease, microaneurysm formation, retinal hemorrhages, and retinal neovascularization. The most common manifestation is probably a mild, or “hyperpermeable,” central retinal vein occlusion (Fig. 155.9). A systemic hyperviscosity state should be suspected in patients with simultaneous, bilateral retinal vein occlusion. Also, the very high white cell count may lead to a hyperviscosity state that results in poor absorption of cerebrospinal fluid, creating a clinical picture similar to that of benign intracranial hypertension with bilateral disc swelling.40
Peripheral retinal microaneurysms in leukemic patients were originally described by Duke et al.41 and subsequently by Jampol et al.42 Duke et al.41 found that 50% of patients dying with chronic leukemia had peripheral microaneurysms. None were seen in patients with the acute leukemias. Seven of nine patients with chronic myelogenous leukemia and three of 10 patients with chronic lymphocytic leukemia had this finding, but it was not present in any of the 21 patients with acute leukemia.41 Kincaid and Green1 saw only one case in their large series. They noted that trypsin digest of the retina was essential or else the change would be overlooked on histopathologic examination.
Peripheral retinal neovascularization has been reported in patients with chronic myelogenous leukemia in association with peripheral capillary nonperfusion. Most cases have associated extreme leukocytosis or thrombocytosis.43–46 Presumably, the hyperviscosity state leads to peripheral nonperfusion and subsequent development of retinal neovascularization, as in patients with proliferative sickle retinopathy.
Morse and McCready46 reported on a 32-year-old patient with chronic myelogenous leukemia and retinal neovascularization. The peripheral white blood cell count was 340 500 and subsequently rose to 524 000/mm3. The fasting blood sugar value was normal, as was the hemoglobin electrophoresis study. No paraproteins were present. A fluorescein study highlighted multiple sea fans, and obliteration of the terminal arterioles was apparent. Frank and Ryan43 described a 30-year-old patient with a subhyaloid and vitreous hemorrhage who had a white blood cell count of 250 000/mm3 related to chronic myelogenous leukemia. Numerous sea fans were apparent and a glucose tolerance test and hemoglobin and serum protein electrophoresis studies were negative.46 Like Morse and McCready,46 Frank and Ryan43 believed that the pathogenic mechanism was related to increased blood viscosity, as in patients with complications of Waldenström macroglobulinemia or polycythemia. Kincaid and Green,1 however, did not see any cases of peripheral retinal neovascularization in their series.
Levielle and Morse44 described a patient with chronic myelogenous leukemia who had a relatively low (33 700/mm3) white blood cell count. In general, the blood viscosity begins to increase remarkably only with white blood cell counts of >50 000.47 In Levielle’s case report, the patient had an elevated platelet count of 988 000/mm3, and the peripheral neovascularization was attributed to this elevation. However, the authors did not emphasize that their patient also had an 11-year history of diabetes mellitus; therefore diabetic retinopathy also may have contributed to retinal capillary non-perfusion and formation of peripheral neovascularization.47 Melberg et al.48 described the effect of acute lymphocytic leukemia on the progression of mild diabetic retinopathy in a 16-year-old girl. The patient developed bilateral rubeosis, and after aggressive laser and vitrectomy, her vision declined to 20/200 bilaterally as a result of macular ischemia. The accelerated course of diabetic retinopathy correlated most closely with the anemia accompanying her leukemia and its treatment.
Wiznia et al.49 reported on concurrent optic disc and retinal neovascularization in an 18-year-old woman with acute lymphocytic leukemia who underwent therapy. They described progression of the neovascularization caused by the additive effects of radiation retinopathy and chemotherapy, resulting in macular traction detachment. The authors postulated that toxic effects of chemotherapy when combined with radiation therapy could lead to a more severe form of ischemic retinal vasculopathy than would be encountered with acute lymphocytic leukemia alone.49
The mechanism of the retinal hemorrhage seen in patients with leukemia is not yet known. The hemorrhages may be caused by an associated anemia or thrombocytopenia. Although commonly associated with severe leukocytosis, white-centered hemorrhages may be present regardless of the degree of leukocytosis.50
Some authors believe that the platelet count is more predictive than the hematocrit for the presence or absence of retinal hemorrhages.51 Kincaid and Green1 summarized the issue in 1983 and wrote that there is no close correlation between the degree of retinal involvement and red blood cell, white blood cell, or platelet levels. We have prospectively correlated the ocular findings with hematologic values on presentation in our series of 120 cases examined within a few days of diagnosis.52 We found a strong association between low platelet counts and intraretinal hemorrhages. Acute lymphoblastic leukemia patients with hemorrhages had a mean platelet count of 26 857/mm3, whereas patients without hemorrhage had mean counts of 116 159 (P≤0.0001); acute myelogenous leukemia patients with platelet counts of <15 000 were more likely than those without such low counts to have intraretinal hemorrhages (55% versus 29%). In addition, there was also a statistical difference between hematocrits (a mean of 20.3 mL/dL for patients with hemorrhage and a mean of 26.2 for patients without hemorrhage). However, a two or three point difference in the hematocrit is not of clinical importance. We believe that the platelet count plays a much stronger role in determining the presence or absence of intraretinal hemorrhage.52 Furthermore, on presentation, hematologic values were not found to be correlated with the presence of cotton-wool spots.
The presence of specific retinal manifestations of leukemic retinopathy and the subsequent risk of developing an intracranial hemorrhage was reported by Jackson et al.53 They reported a fivefold relative risk of an intracranial hemorrhage developing in those patients with macular hemorrhages compared with those patients without such hemorrhage. No increased risk of intracranial hemorrhage existed with the presence of non-macular intraretinal hemorrhages, white-centered hemorrhages, or cotton-wool spots. Therefore, patients with macular hemorrhages may require close monitoring for the possible development of intracranial hemorrhages, and these patients may need platelet transfusions if such an intracranial hemorrhage occurs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree