Essentials of Diagnosis
General Considerations
The larynx serves three important functions: airway protection, regulation of respiration, and phonation. Injury to the larynx resulting from trauma can therefore be devastating. Fortunately, laryngeal trauma is rare and occurs in only a small percentage of trauma victims. Standardized protocols have been developed to help guide the accurate evaluation and identification of injuries requiring operative intervention. Early diagnosis and treatment are critical to prevent dire consequences, including death.
Pathogenesis
The relatively low incidence of laryngotracheal injuries results from the natural defenses that the body has to protect the vital structures that allow us to breathe. The relatively high position of the sternum and low position of the mandible along with the thick musculature of the lateral neck allow only a relatively short segment of the airway to be exposed.
Furthermore, there is a naturally protective reflex that causes the head to be flexed downward when startled, allowing for further protection of this region. Injury typically occurs when the body cannot protect this area. This generally occurs in motor or recreational vehicle accidents, assaults (including domestic violence), sports injuries, or strangulation. In motor vehicle accidents, the laryngeal skeleton and/or cricoid cartilage may be shattered between the steering wheel and the cervical spine. Clothesline injuries, although rare, may result classically in cricotracheal separation and bilateral recurrent laryngeal nerve injuries.
The pediatric age group deserves special mention because children have anatomic differences that make the management of laryngeal injuries a distinct entity when compared with the management of similar injuries in adults. Although children are less prone to laryngeal fracture owing to the high position of the larynx in the neck and the increased pliability of the laryngeal cartilage, their diminutive anatomy makes them more vulnerable to life-threatening complications from the injury.
Penetrating trauma to the neck is challenging because up to 30% of patients have multiple structures injured. Penetrating neck trauma usually results from stabbings or gunshot wounds. The severity of a penetrating injury is determined by the mass and velocity of the missile. Therefore, generally, high-velocity, large-caliber bullets will create more damage. However, a variety of bullet types are available that can increase local tissue damage, either by breaking up or exploding on contact or by spiraling in the tissues.
Because of sophisticated intensive care units, critically ill patients are being sustained longer on ventilatory support with the potential long-term consequences of affected speech and airway patency. Such complications may include scarring of the laryngeal structures, subglottic or tracheal stenosis, formation of granulation tissue, and vocal fold paralysis/paresis. Although the true incidence is unknown, complication rates of 4–19% have been reported after prolonged intubation; therefore, converting an intubated patient to a tracheotomy is often contemplated after 5–7 days. The benefits of tracheotomy as a management strategy for the prolonged intubation patient include the ability to (1) decrease dead space, (2) improve pulmonary toilet, (3) increase comfort and decrease the need for sedation, (4) ease the process of weaning, and (5) lessen the risk of long-term complications.
Many factors determine the severity of intubation injury. Anatomic variations predispose some patients to a difficult or traumatic intubation. Underlying illness, infection, and reflux laryngitis all may exacerbate the injury. Although glottic edema and superficial ulceration may be seen within just hours of intubation, the use of large-diameter endotracheal tubes, excessive patient movement, repeated self-extubation, overinflated endotracheal tube cuffs, and prolonged intubation increase the risk of long-term damage.
Intubation-related injuries may be reduced by eliminating or controlling the above-listed factors. We routinely ensure that patients are maintained on antireflux medications while intubated. In addition, we attempt to ensure that cuff pressures are kept low. However, as we demonstrated in a recent paper, serial measurement of cuff pressures does not ensure proper pressure maintenance.
Arytenoid dislocation is a special consideration that has been reported as a result of intubation problems. The cause is likely either extreme force applied directly to the arytenoids by a laryngoscope or endotracheal tube or careless extubation with an inflated cuff. The diagnosis is controversial. Some clinicians propose that it is often misdiagnosed and may actually represent the appearance of new onset vocal fold paralysis.
Clinical Findings
The evaluation of a patient with a suspected laryngeal injury begins with a detailed history (when possible) that specifically addresses the following items: (1) the development of symptoms, (2) the mechanism of injury, and (3) the trajectory of any involved weapons. This information is often difficult to elicit in a patient with multiple traumas because the ability to provide information is compromised by the severity of the injuries. These injuries can include communication deficits caused by concomitant head injuries or illicit substance abuse. Common symptoms include hoarseness, pain, dysphagia, odynophagia, and dyspnea. The failure to elicit these symptoms, however, does not ensure the integrity of the airway. Therefore, a high index of suspicion is mandatory in any patient with neck trauma.
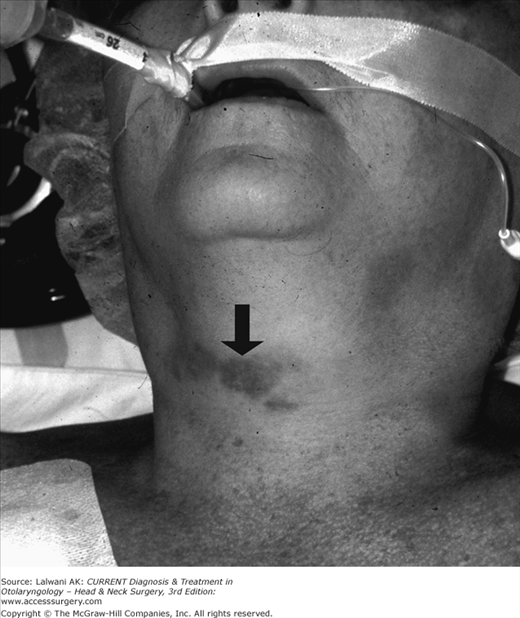
The physical examination begins with careful attention to the voice and breathing. The presence of hemoptysis, stridor, or crepitus should alert the physician to a high probability of airway injury. Point tenderness or flattening of the thyroid cartilage prominence is suggestive of an acute laryngeal fracture. Penetrating trauma may involve multiple vital structures such as the esophagus or the carotid neurovascular bundle. An expanding hematoma, a pulse deficit, or the presence of a bruit and thrill all are signs of vascular injury. The prompt diagnosis of these life-threatening injuries requires a methodical investigation. Further evaluation is directed by careful attention to subtle signs and symptoms (Figure 34–1).
One of the most important instruments in diagnosing laryngeal trauma is the fiberoptic nasopharyngoscope. In using this device, the larynx should be evaluated carefully for vocal cord mobility and arytenoid symmetry. Notation should also be made regarding findings of edema, hematoma, soft tissue tears, and exposed cartilage. An attempt should also be made to evaluate the upper trachea by direct examination if the patient tolerates the exam.
Plain-film x-rays of the chest and soft tissue neck films continue to be essential components in patient evaluation. Any abnormal air surrounding the trachea, mediastinum, or thorax may be the first sign of impending tension pneumothorax and airway embarrassment.
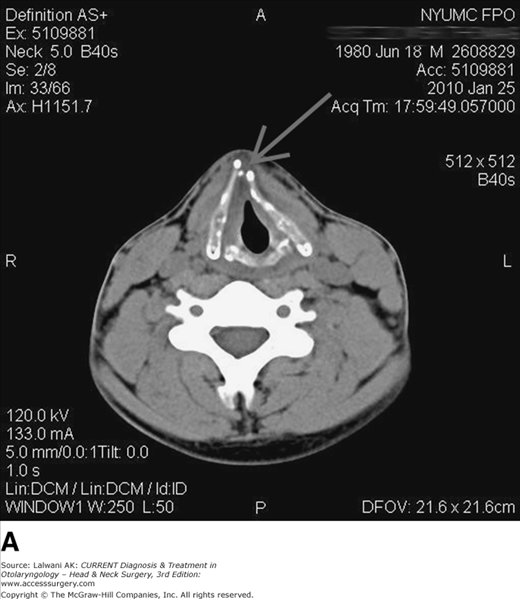
High-resolution fine-cut CT of the larynx is the best radiographic tool available to evaluate laryngeal trauma. It is especially helpful when the examination is normal but there is a high index of suspicion for occult laryngeal injury. A CT scan is not mandatory in patients with injuries that obviously require operative intervention or in asymptomatic patients with an unremarkable physical examination. However, CT scanning, especially with 3D reconstruction (Figure 34–2), may be valuable in helping to plan the operative procedure in a patient with a controlled and stable airway.