Keratoconus and Other Noninflammatory Corneal Thinning Disorders
Atul Jain
Yannis M. Paulus
Glenn C. Cockerham
Kenneth R. Kenyon
Corneal thinning disorders are a significant cause of visual disability due to structural instability and loss of surface regularity. This chapter will address noninflammatory conditions leading to corneal thinning, including the most common entity, keratoconus (KC), as well as pellucid marginal degeneration (PMD), keratoglobus (KG), and Terrien’s marginal degeneration (TMD) (Table 1). This schema will not discuss corneal thinning disorders secondary to or associated with inflammation and necrosis, such as peripheral ulcerative keratitis and Mooren ulcer.
TABLE 1: Noninflammatory Corneal Thinning Disorders. | |
|---|---|
|
KC
KC is a bilateral noninflammatory condition in which the cornea assumes a conical shape due to thinning of the corneal stroma. The term KC means “conical cornea.” The thinning and axial ectasia result in visual impairment from irregular astigmatism, myopia, and subsequent scarring.1 KC generally manifests at puberty and can progress either slowly, stabilizing over approximately 10 years, or relatively rapidly, leading to severe irregularity of the corneal surface. In the last decade, new insights into the genetic and biochemical abnormalities in KC have been reported. New therapies have been described, which appear to halt progression of KC in some cases.
Epidemiology and Genetics
Although familial in nature, no exclusive pattern of inheritance exists. The incidence of KC varies between 50 to 230 per 100,000 in the general population (about 1 per 2000) with an estimated prevalence of about 54 per 100,000, without any reported ethnic or gender preponderance.1,2,3
KC occurs in association with a variety of ocular and systemic diseases, including Down syndrome, atopic disease, contact lens use, and connective tissue diseases.4,5,6,7 Table 2 provides a comprehensive list of diseases reported to have an association with KC. Vigorous eye rubbing has been noted as an important factor in the genesis of corneal thinning and is a common behavior in many of the noted associations, including Down syndrome, atopy, and contact lens use.
TABLE 2: Conditions Associated with KC. | ||||||
|---|---|---|---|---|---|---|
| ||||||
Less than 2% of KC cases are associated with a genetic disorder; the remainder of cases are considered sporadic8 Heredity is important in some cases as evidenced by twin studies, the bilaterality of the disorder, familial aggregation, and genetic studies.8,9,10,11,12 A distinct gene or mutation has not yet been identified as a cause of KC. Candidate genes associated with some cases of KC include the VSX1 homeobox and superoxide dismutase 1 (SOD1) genes.13,14 Suggested biochemical mechanisms in the pathogenesis of KC include stromal thinning through the actions of collagenolytic proteinases (metalloproteinases), decreased expression of aquaporin 5,15,16 and apoptosis of stromal keratocytes.17
Clinical Findings
The typical presentation of a patient with early KC is increasing myopia and inability to achieve previous levels of vision despite appropriate refraction. This progression usually occurs in the second or third decade. Subtle irregular astigmatism is often the first clinical finding in KC and is evidenced by a distortion of the retinoscopic reflex, which is known as “scissoring.” Other helpful clinical signs include Munson’s sign, a “V” shaped conformation of the lower eyelid produced in downgaze by the ectatic cornea (Fig. 1), and Rizzuti’s sign, a focused beam of light produced at the nasal limbus by illumination originating temporally.18,19
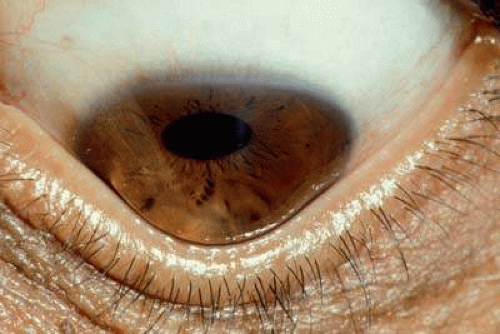 FIGURE 1. KC. Munson’s sign, an indentation of the lower eyelid by protruding cornea, is present in this advanced case of KC. |
Slit-lamp findings include central or paracentral stromal thinning, most commonly inferiorly or inferotemporally, and conical protrusion (Fig. 2). Fleischer’s ring, a brown line representing iron deposits circumscribing the base of the cone, may be seen with white light but is best visualized as a dark line using the blue light of the cobalt filter. Vogt’s striae are very fine vertical lines located in the deep stroma and Descemet’s membrane that disappear with gentle pressure. Anterior stromal scars and enlarged corneal nerves may be noted.20,21 Acute hydrops occurs when Descemet’s membrane is stretched beyond its elastic breaking point. Such a rupture leads to sudden, profound corneal edema (Fig. 3). Endothelium bridges the gap within 6 to 8 weeks with gradual stromal deturgescence and residual stromal scarring of varying severity.
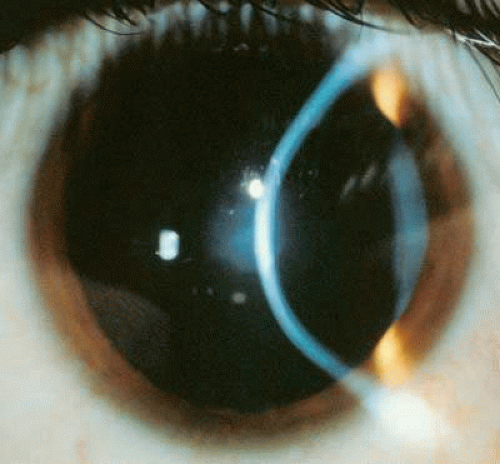 FIGURE 2. KC. The tangential slit lamp beam demonstrates paracentral corneal thinning and protrusion. |
 FIGURE 3. KC. Inferior corneal edema has occurred from rupture of stretched Descemet’s membrane with tear of endothelium (acute hydrops). |
Ancillary testing for KC has classically consisted of the interpretation of a reflection from the anterior corneal surface. Reflection of a hand-held Placido disc can be visualized at the slit lamp and allows a qualitative determination of degree and orientation of regular (orthogonal) astigmatism, as well as detection of irregular astigmatism through distortion of the ring pattern. Standard keratometry, which has been in clinical use for over a century, continues to be helpful in the diagnosis of corneal disturbances. In 1854 Herman von Helmholtz used of a low-power telescope to view an image reflected from the precorneal tear film and realized that the curvature of the anterior cornea can be calculated from the ratio of the size of the apparent reflection (mire) to the actual size.22 Helmholtz calculated the corneal stroma index of refraction to be 1.3375, which also accounts for the estimated power of -5 diopters for posterior cornea. Corneal power is derived from the calculation K (diopters) = 337.5/radius. Irregular astigmatism is evident through distortion of the reflected mires. Limitations of standard keratometry include the underlying assumption that the cornea is spherical. This assumption holds to a reasonable approximation within the 3 mm central area tested by the keratometer, but it does not hold beyond this. Keratometry only tests two points on the corneal surface and lacks the ability to quantitate or store images.
A major advance is computerized videokeratography (CVK), which captures a reflected image of concentric rings and quickly analyzes ring location, size, and regularity. CVK allows assessment of the paracentral and peripheral cornea, overcoming the limitations of standard keratometry. Standard algorithms allow derivation of axial maps, tangential maps, and surface elevation maps, which are depicted by a color scale. Additional indices performed by CVK include simulated keratometry, surface regularity or symmetry, and potential visual acuity based on corneal characteristics. CVK is useful in the diagnosis and follow-up of KC and other corneal thinning disorders. Subclinical KC, or forme fruste KC, is characterized by asymmetric astigmatism with increased power in the inferior meridian. Rabinowitz and McDonnell suggested the use of screening guidelines for KC based on the typical inferior location of conical protuberance.23 This inferior-superior (I-S) index is based on five superior and five inferior data points, which are located 3 mm from the corneal center. An I-S value greater than 1.4 D is suggestive of KC. A central corneal power greater than 47.2 D has also been identified as a risk factor for KC.23 Limitations of CVK include the ability to image only the anterior surface, and assumptions that may not include unusual presentations.
The Orbscan Analyzer (Bausch and Lomb, Rochester, NY, USA) uses a scanning slit beam with a Placido disc to make a representation of the anterior corneal surface. The Orbscan then mathematically recreates the posterior cornea, anterior iris, and lens from the previously acquired data. It has been found to be more accurate in the periphery, however it tends to overestimate the posterior cone height. However, because the Orbscan is able to evaluate both the anterior and posterior corneal surfaces, it is able to detect subtle steepening that might represent very early KC, which is very useful when evaluating a patient for possible keratorefractive procedures.24,25
Pathology of KC
Stromal thinning with ectasia is characteristic of KC. Iron deposition in the epithelium at the cone base is demonstrated with an iron stain, such as Prussian blue. Focal breaks in Bowman’s layer with plugs or facets of epithelial cells and collagen may be found.26 The epithelium has an irregular thickness and has an abnormal basement membrane in areas where Bowman’s layer is destroyed.21,27,28 Ultrastructural examination in areas of healed hydrops reveals torn edges of Descemet’s membrane with characteristic scrolling due to retraction. Endothelial cells adjacent to the torn edges slide over the exposed surface of posterior stroma with deposition of a new thin Descemet’s membrane.29
Treatment
Management of KC varies depending on disease severity. In mild cases of KC, adequate visual correction may be obtained with spectacles or soft contact lenses. As the disease progresses, corneal steepening often requires a rigid lens to correct irregular astigmatism. A variety of lens designs and materials are available, but patience and experimentation are usually necessary to achieve an acceptable vision. Computerized topography is helpful in obtaining paracentral keratometric values and demonstrating cone location. Central cones are generally easier to fit, whereas cones located off-axis lead to lens decentration. Fluorescein staining will demonstrate the cone apex touching the posterior contact lens surface.3
Intracorneal rings (Intacs) (Addition Technologies Inc., Des Plaines, IL, USA) are approved by the Federal Drug Administration (FDA) for treatment of KC in patients older than 21. Placement of one or two rigid rings made of polymethylmethacrolate (PMMA) into corneal stroma provides biomechanical splinting and allows the central cornea to assume a more spherical shape. A stromal thickness less than 450 microns is a contraindication for Intacs use.30
Cross-linking of stromal collagen with topical riboflavin 0.1% and UVA 370 nm laser has been reported to strengthen the cornea and arrest progression of KC. The underlying principle behind this treatment is that cross-linking of stromal collagen increases corneal rigidity and prevents further ectasia. The corneal epithelium is removed from the central corneal and riboflavin is applied to the stroma every 5 minutes and irradiated for 30 minutes. Three and five year data on patients with progressive KC who underwent cross-linking show a halt in the progression of KC in all eyes and a mild regression of KC (decreased steepening) in some eyes.31,32 This is a promising new therapy in the treatment of progressive KC.
The traditional method of vision restoration in advanced KC is full-thickness penetrating keratoplasty, which replaces the thinned and unstable cornea with a mechanically sound donor tissue. KC has a high success rate (93% to 96%) for a clear graft at 1 to 2 years, which is probably due to the healthy recipient’s endothelium and lack of ocular comorbidities. Up to 86% of transplanted eyes achieve a best-corrected visual acuity of 20/40 or better with contact lens use.33,34,35,36,37 Because patients may be left with significant myopia or astigmatism after grafting, patients should be counseled that the goal is visual rehabilitation with the use of a contact lens.16,38
KG
KG is a bilateral cause of corneal ectasia characterized by a protrusion of a clear, limbus-to-limbus thin cornea of normal to moderately increased diameter.39,40 KG resembles megalocornea, except the cornea is uniformly thinned to 20% of normal thickness, particularly in the periphery and midperiphery. It is non- or minimally progressive.
Epidemiology and Genetics
KG is extremely rare with an estimated incidence substantially below that of KC and PMD.1 Two forms of KG have been noted: an acquired adult form and a congenital juvenile-onset form. The acquired form may be an end-stage of KC. It has been associated with vernal keratoconjunctivitis,4,42,43 blepharitis, and orbital diseases causing proptosis.44 The congenital form has been associated with three autosomal recessive disorders: Ehlers-Danlos syndrome type VI, Leber’s congenital amaurosis,45,46 and brittle corneal syndrome with associated blue sclera and red hair (a mimic of Ehlers-Danlos syndrome type VI, but with normal lysyl hydroxylase activity).41,47,48,49,50,51 KG may be associated with scleral thinning, but is not associated with atopy.41
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


