Jaw Cysts: Introduction
Cysts of the maxilla and mandible are common occurrences. Bone cysts occur more frequently in the jawbones than in any other bone because of the presence of epithelium from odontogenic elements (eg, teeth) and nonodontogenic epithelial remnants of embryonic structures.
A cyst is defined as an epithelial-lined pathologic cavity that may contain fluid or a semisolid material. A group of cystic lesions devoid of an epithelial lining is classified as pseudocysts. A jaw cyst is usually located deep within the jawbone, but it may occur on a bony surface, producing a saucerization.
- Well-defined, totally or predominantly radiolucent, and sometimes expansile lesions.
- Usually slow growing and benign.
- Initially asymptomatic unless long-standing with significant enlargement or secondary infection.
- Usually initially discovered on routine dental X-rays.
- Requires histopathologic examination for diagnosis.
Jaw cysts encompass a group of lesions that are variable in their incidence, etiology, location, clinical behavior, and treatment. The most common jaw cyst is the radicular cyst, which is odontogenic and inflammatory in nature. The odontogenic developmental cyst is the second most common jaw cyst. Nonodontogenic cysts, pseudocysts, and ganglionic cysts of the temporomandibular joint (TMJ) are much less common. Cysts occur in both the mandible and the maxilla: inflammatory radicular cysts occur around the roots of nonvital teeth; odontogenic developmental dentigerous cysts and keratocysts occur in the common regions of impacted and unerupted teeth; nonodontogenic developmental cysts are found in regions of epithelial embryonic remnants; pseudocysts usually present in site-specific regions; and ganglionic cysts develop in the TMJ. Each type of jaw cyst usually has a specific behavior pattern, ranging from small 5- to 6-mm osteolytic defects to massive involvement of the jaw and contiguous structures.
The classification of jaw cysts includes (1) odontogenic cysts, (2) nonodontogenic cysts, and (3) pseudocysts. The ganglion cyst, which presents in the TMJ, has been added to this conventional classification for completeness; it is significant to clinicians managing the pathology of the head and neck region.
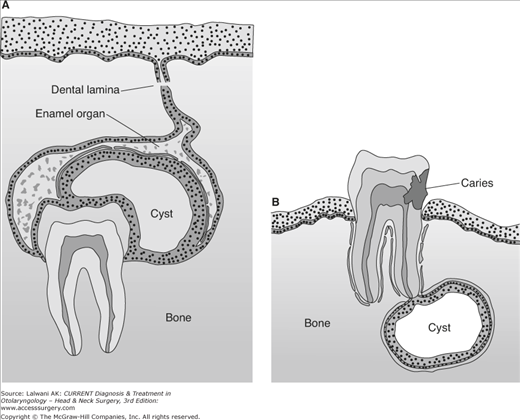
The pathogenesis of jaws cysts varies according to the specific cyst type. Inflammatory cysts derive their epithelial lining from the proliferation of odontogenic epithelium within the periodontal ligament; dentigerous developmental cysts result from the proliferation of reduced enamel epithelium. Figure 25–1 illustrates the development of dentigerous and radicular cysts. Cystic lesions may also result from cortical bone defects or trauma, they may represent reactive lesions, or they may have an unknown pathogenesis. It has been shown that there is an osmotic pressure gradient that produces fluid accumulation within the cyst lumen and generates pressure, creating cyst expansion.
It may be possible to prevent odontogenic jaw cyst formation through the immediate treatment of nonvital teeth and the removal of impacted or unerupted teeth. Strategies should include preventing the progression of jaw cysts to large, destructive lesions that require aggressive management. Prevention is aided by routine and regular dental and oral examinations with appropriate imaging.
The patient with a small cyst is usually asymptomatic. Symptoms such as pain and swelling occur when the cyst becomes secondarily infected. The patient may report an unpleasant or even foul taste if the cyst has discharged into the mouth through a sinus tract. Teeth contiguous to all cysts, except radicular cysts, have vital pulps, unless coincidental disease of these teeth exists. Tooth vitality can be assessed with electrical pulp testers or ice. Erupted teeth contiguous to a large cyst may maintain their vitality, despite the loss of a significant amount of supporting alveolar bone. Benign jaw cysts rarely produce loosening of adjacent teeth unless the cyst becomes very large. Large cysts can displace the roots of teeth that can be evident clinically, on an X-ray, or both. The clinical absence of one or more teeth, as seen on routine dental X-rays, may suggest the presence of a developing dentigerous cyst.
Extensive cysts in the anterior maxilla may extend under the nasal floor, creating nostril distortion. An infected maxillary cyst may involve the maxillary sinus, producing maxillary sinusitis. Large mandibular cysts may involve the mandibular canal and its contents, the inferior alveolar neurovascular bundle. The mandibular canal and its contents can be deflected inferiorly without producing a neurosensory deficit. However, if an acute infection develops with pus accumulation, a decrease in lower lip sensibility may be observed.
The typical radiographic appearance of a jaw cyst is that of a well-defined, round-to-oval, unilocular or multilocular radiolucent cyst that is circumscribed by a dense periphery of reactive bone. Periapical and panoramic X-rays usually suffice for imaging small- to medium-sized cystic lesions, but computed tomography (CT), including cone beam, scans are indicated for large, expansile lesions. Anatomic structures such as the mental foramen, the incisive foramen, and the maxillary sinus may be misinterpreted as pathologic cystic lesions.
Needle aspiration of a suspected jaw cyst can reveal valuable diagnostic information. Aspiration of blood from the lesion may indicate the presence of a vascular lesion or an aneurysmal bone cyst. If aspiration of a solid lesion (eg, a tumor) is attempted, no fluid can be aspirated and withdrawing the plunger of the syringe is difficult. Aspiration of a light, straw-colored fluid containing cholesterol crystals (known by their characteristic “shimmering” effect in light) is consistent with a benign odontogenic cyst. Aspiration of a whitish-to-pale-yellow material that appears similar to pus usually reveals an odontogenic keratocyst (OKC) that contains desquamated cells and keratin. A cyst that has been present for a long time and has become infected may contain a thick yellow or brown material that is difficult to aspirate.
A histopathologic examination is essential for establishing a definitive diagnosis. For small lesions, excisional biopsy is appropriate; for large lesions, an incisional biopsy is indicated to establish a diagnosis, develop a treatment plan, and obtain appropriate informed consent.
An orderly approach to a differential diagnosis of a jaw lesion can be accomplished by grouping possible lesions into six main categories: (1) cysts, (2) odontogenic tumors, (3) benign nonodontogenic tumors, (4) inflammatory jaw lesions, (5) malignant nonodontogenic neoplasms of the jaw, and (6) metabolic and genetic jaw diseases. An assessment of the radiographic appearance, patient age, and location of the lesion enables the clinician to establish a reasonable differential diagnosis that should ultimately be confirmed by histopathologic examination. A definitive histopathologic diagnosis may rule out more serious lesions (eg, cystic ameloblastoma).
Complications related to the destruction caused by a jaw cyst and the surgical treatment required include loss of teeth and bone; infection; cyst recurrence; neurosensory deficits; oral or facial sinuses; oral, antral, or nasal fistulas, or a combination of these three complications; and pathologic jaw fracture. Carcinoma arising in an odontogenic cyst is a rare occurrence and requires aggressive treatment.
Because contiguous structures—including displaced teeth, resorbed roots, alveolar bone, the maxillary sinus, and the mandibular canal—may be involved or encroached upon, jaw cysts usually require surgical management. However, jaw cysts that demonstrate slow or no progression of growth may be managed by observation in the elderly or severely medically compromised individuals. The exact nature of the surgery depends on the size, location, and clinical behavior of the specific type of cyst. Treatment is necessary because (1) cysts usually increase in size, causing local tissue destruction and usually becoming infected, and (2) extensive involvement of the mandible is capable of creating a potential pathologic fracture.
Specific Types of Jaw Cysts
- Epithelial-lined, developmental, odontogenic cysts.
- Second most common type of jaw cyst associated with the crown of an impacted, unerupted, or developing tooth.
- Well-defined, radiolucent, sometimes expansile lesion.
- Usually slow growing and benign.
- Initially asymptomatic unless long-standing with significant enlargement or secondary infection.
- Usually discovered on routine dental X-rays.
- Requires histopathologic examination for diagnosis.
Fifteen to eighteen percent of jaws cysts are dentigerous, surround the crowns, and attach at the cementoenamel junction of unerupted teeth. The lower third molars and the upper canines are the most commonly involved teeth.
Dentigerous cysts derive their epithelium from the proliferation of the reduced enamel epithelium after the tooth enamel is formed. The cyst develops subsequent to an accumulation of fluid between the remnants of the enamel organ and the contiguous tooth crown. The expansion of this intrabony cyst is associated with an increase in the osmolality of the cyst fluid secondary to the migration of inflammatory cells into the cyst lumen. Epithelial proliferation may also occur simultaneously.
Regular dental and oral examinations with appropriate imaging can identify developing cystic jaw lesions before any significant bony destruction can occur. The removal of impacted teeth, when indicated, serves as a preventive measure.
Small dentigerous cysts rarely produce clinical symptoms. Larger cysts can produce a bony expansion, which creates an intraoral swelling, an extraoral swelling, or both. They also can result in facial asymmetries or can become secondarily infected, which results in pain.
The most common radiographic appearance of a dentigerous cyst is that of a well-delineated round-to-oval mass that is associated with an unerupted tooth, which may possibly be displaced. Figure 25–2 demonstrates a typical dentigerous cyst as observed on a panoramic X-ray. Periapical and panoramic X-rays can illustrate the extent of the cyst and contiguous anatomic structures. With large lesions, CT scanning is helpful in assessing the degree of expansion perforation and the involvement of adjacent structures.
Needle aspiration with possible biopsy of the lumen of a suspected cystic lesion can give confirmatory diagnostic information and rule out a vascular lesion. If there has not been significant expansion of the cyst, with thinning of the bony cortex, it will not be possible to penetrate the bone using a needle and syringe technique. In these cases, if aspiration is desired, a small mucosal incision, followed by drilling a small hole through the buccal cortex, enables needle aspiration. Aspiration of a light, straw-colored fluid is characteristic of a dentigerous cyst. Histopathologic examination reveals a thin, nonkeratinized cyst lining. Inflammatory changes may produce epithelial hyperplasia. Mural hemorrhage can result in cholesterol clefts, giant cells, and hemosiderin in the wall of the cyst. Hyaline bodies (eg, Rushton or hyaline bodies) may be present in the epithelium.
The differential diagnosis should include OKCs, ameloblastomas, cystic ameloblastomas, ameloblastic fibromas, and nonodontogenic tumors.
Complications related to the damage created by an expanding jaw cyst include bony destruction, infection, oral or facial sinuses, weakening of the jaw, displacement of teeth, resorption of adjacent tooth roots, encroachment on the maxillary sinus floor, and deflection of the inferior alveolar canal. The transformation of the epithelial lining of a dentigerous cyst into an ameloblastoma is also possible. Dysplasia or the carcinomatous transformation of the epithelial lining is possible, but rare. Complications related to the surgical management of cysts include devitalization of adjacent teeth, postoperative infection, neurosensory deficits, oral-antral fistulas, jaw fracture, and cyst recurrence.
The treatment of choice consists of enucleation of the cyst and removal of the associated tooth. The surgical exposure is observed in Figure 25–3. The surgical flap can be repositioned and sutured with primary closure. Even large, bony cavities can regenerate new bone over several months’ time. If the tissue breaks down, the cavity can be packed with a ¼-inch gauze and gradually advanced over 7–10 days, followed by frequent saline irrigations to allow healing by secondary intention. For extremely large surgical defects, primary bone grafting with autogenous cancellous chips can accelerate the healing process. Marsupialization of the cyst may be considered.
The prognosis after treatment of the cyst is excellent, with the expectation that the surgical defect will heal. The recurrence rate for the cyst is very low.
- A variant of the dentigerous cyst.
- Presents as a bluish swelling on the alveolar ridge crest at the site of an erupting tooth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree