Fig. 7.1
Boston Keratoprosthesis prognostic categories as described by Yaghouti et al. [10]. A Kaplan-Meier analysis for survival of ambulatory vision (visual acuity between 20/20 and 20/200) was performed for 53 eyes with KPro types I and II. In this study, a clear difference in visual acuity attrition was elucidated for each of the following four patient categories: noncicatrizing graft failure, ocular cicatricial pemphigoid, chemical burns, and Stevens-Johnson syndrome (Reprinted with permission from Lippincott Williams & Wilkins, Inc.)
7.2 Preoperative Considerations
The Boston KPro is available in two models: KPro type I and KPro type II. The selection of a type I or type II device for a particular patient relies upon the severity of the underlying ocular surface disease and dry-eye status. The type I device, which was approved by the US Food and Drug Administration (FDA) in 1992, is the most commonly used model and is favored in the eyes with adequate blink mechanism and tear secretion. The type II device, with its anterior nub protruding through a permanent tarsorrhaphy, prevents evaporative tear loss and allows for better protection of the ocular surface. Hence, the KPro type II is the preferred alternative in patients with severe autoimmune disease or end-stage dry eye.
A meticulous ocular exam is required to identify the eyes with a good visual potential and to appropriately plan the KPro procedure. Slit-lamp examination should focus on the overall health of the ocular surface and quality of the tear film. Lid anatomy, blink and tear secretion rates, ocular surface inflammation, cicatrization, keratinization, and the presence of epithelial defects are important considerations to determine which patients are better suited for a type II device. In practice, the presence of symblepharon, ankyloblepharon, or ocular surface keratinization and the absence of normal lid function strongly suggest KPro type II implantation.
7.3 Indications
It is difficult to unequivocally define the indications for KPro as they continue to evolve. However, general guidelines can help identify good candidates for this procedure. Preoperative visual acuity (VA) should range from 20/100 to light perception (LP), with most patients having a VA of 20/400 or worse. Poor vision should be due to corneal opacification, and the probability of success with standard keratoplasty should be low due to a history of prior failed graft, LSCD, severe neurotrophism, or corneal vascularization. As much as possible, the surgeon should demonstrate good retinal and optic nerve function. There should be a reasonable prospect for the restoration of meaningful vision.
While the preoperative diagnosis is a crucial factor influencing outcomes, one cannot overemphasize the importance of long-term commitment from both the patient and the surgeon. Potential candidates should have realistic expectations and understand the importance of continued adherence to the postoperative prophylactic regimen. Lifelong regular follow-up by an ophthalmologist and ready access to a multi-specialty care team are essential to prevent and manage complications.
7.4 Contraindications
KPro surgery should not be considered in patients for whom traditional keratoplasty holds a good chance of success. On the other hand, the presence of ocular comorbidities such as end-stage glaucoma, retinal pathology, or phthisis is a contraindication to KPro surgery. Typically, this includes patients with a preoperative vision without central fixation or nasal projection or absence of LP. While KPro was traditionally reserved for patients with bilateral blindness, good vision in the contralateral eye is no longer considered a contraindication [12]. Finally, KPro surgery should be avoided in patients that are unable or unwilling to adhere to the postoperative follow-up and prophylactic regimen.
7.5 Specific Indications for KPro Surgery
7.5.1 Classic Prognostic Categories
7.5.1.1 Autoimmune Diseases
Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis
SJS and TEN are part of a spectrum of severe cutaneous adverse reactions affecting both the skin and at least one mucous membrane. In the acute stage, extensive ocular surface inflammation develops in 50–84 % of patients with SJS or TEN [13–16]. Chronic ocular disease is characterized by corneal conjunctivalization, neovascularization and scarring, ocular surface keratinization, symblepharon formation, and severe eyelid deformities such as trichiasis and entropion [17].
SJS and TEN are recognized to have the poorest prognosis following ocular surface reconstruction. The eyes with SJS and TEN are particularly vulnerable to corneal melt, leak, infection, and extrusion following KPro [5]. These eyes may be candidates for either KPro type I or II, depending on the severity of ocular surface disease. With appropriate patient selection and postoperative management, good outcomes can be achieved (Figs. 7.2 and 7.3) [18].
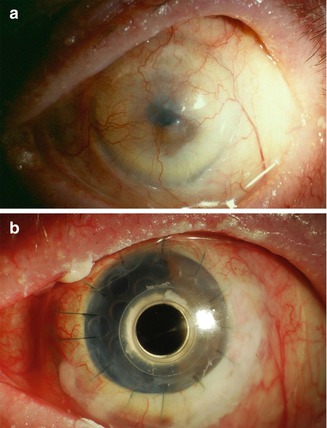
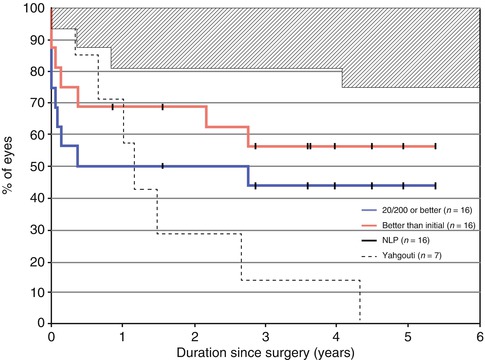
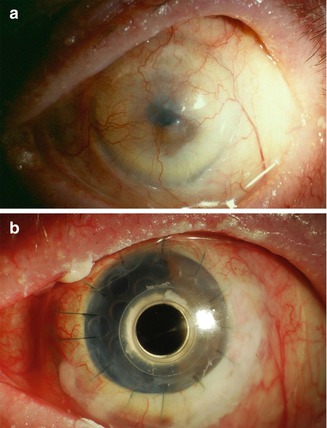
Fig. 7.2
Slit-lamp photographs of the left eye of a 62-year-old patient with Stevens-Johnson syndrome. Preoperative vision was CF due to limbal stem cell deficiency with neovascularization and scarring (a). Following KPro type I implantation, vision improved to 20/40. This level was maintained for 29 months postoperatively. Vision ultimately declined to 20/400 following an intraoperative suprachoroidal hemorrhage
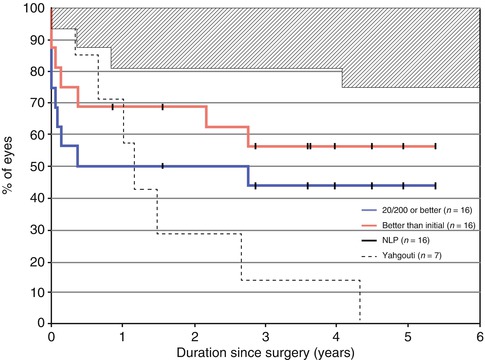
Fig. 7.3
Kaplan-Meier analysis of 16 eyes with Stevens-Johnson syndrome implanted with a Boston KPro. Primary outcomes were loss of 20/200 vision or better (blue), loss of any vision better than preoperative (red), and loss of light perception (shaded area). The results of this study by Sayegh et al. (2008) [18] are compared to those of Yaghouti et al. (2001, dashed line) [10] and demonstrate the improved outcomes of KPro implantation in this high-risk population (Reprinted with permission from Elsevier Inc.)
Mucous Membrane Pemphigoid
MMP is an autoimmune blistering disease of the mucosal membranes characterized by linear autoantibody deposition in the epithelial basement membrane zone. MMP with ocular involvement (MMPO), previously known as ocular cicatricial pemphigoid (OCP), is a subset of MMP affecting the conjunctiva primarily [19]. The disease is characterized by a blistering conjunctivitis and progressive subepithelial fibrosis leading to forniceal shortening and symblepharon formation. Ankyloblepharon, severe dry eye, LSCD, and surface keratinization mark the end stage of the disease [20, 21]. Systemic immunosuppression is necessary to control active disease and prevent scarring and progression to corneal blindness. In patients with advanced MMP, visual rehabilitation requires surgery. Following KPro, patients with MMP tend to have better prognosis than those with SJS and TEN, but the risk of tissue necrosis, aqueous leak, and prosthesis extrusion remains [5, 22, 23]. Patients with MMP are older and thus, have a higher chance of having ocular comorbidities such as glaucoma and retinal detachment. These patients are also prone to skin retraction around the anterior nub following KPro type II implantation.
7.5.1.2 Chemical Burns
Chemical injuries cause widespread ocular damage that may lead to LSCD and edema-related corneal opacity, glaucoma, cataract, and retinal detachment (Fig. 7.4). Rapid visual rehabilitation is possible with KPro implantation, but the prognosis is guarded compared to that of other non-autoimmune diseases. Indeed, the progressive loss of vision secondary to uncontrolled glaucoma has been well described following KPro surgery [11, 24]. The eyes with alkaline burns tend to have a worse prognosis than those with acid burns (Fig. 7.5).
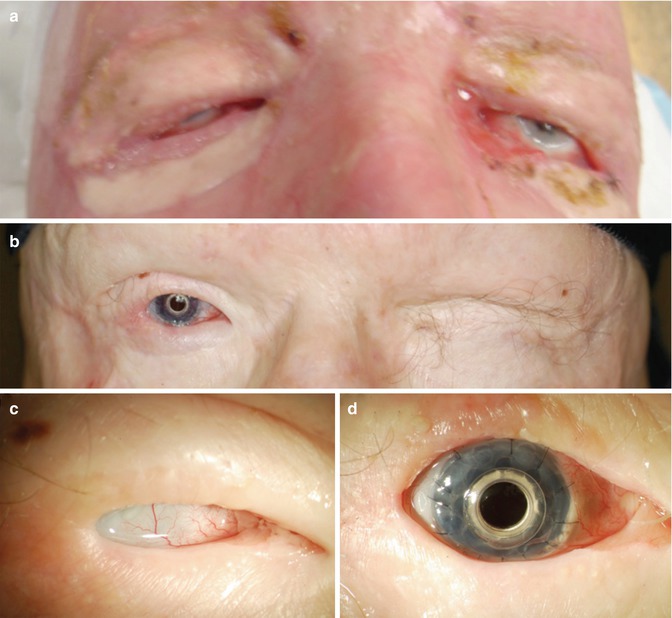
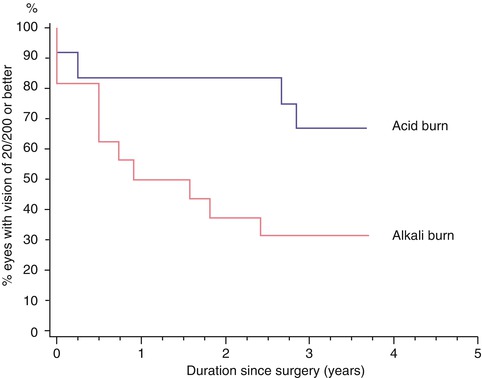
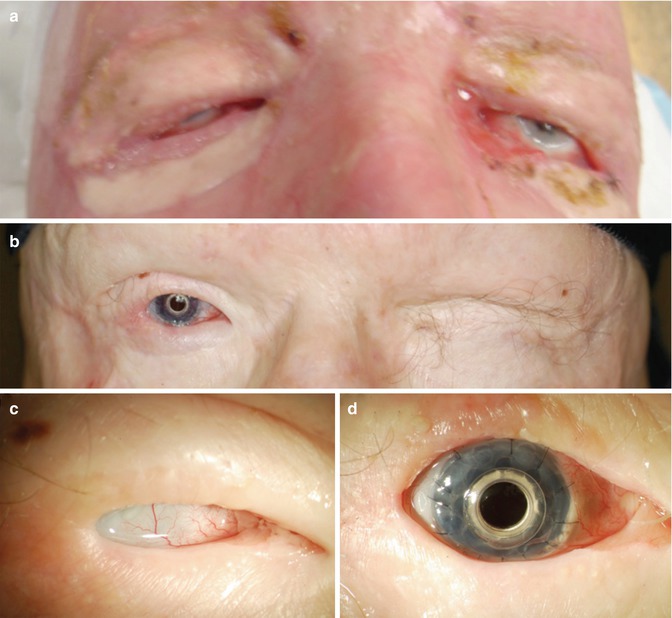
Fig. 7.4
Slit-lamp photographs of a 31-year-old patient with bilateral sulfuric acid burns (a, c). Recurrent corneal necrosis and perforation of the right eye was treated with two corneal grafts performed 2 months apart. Tarsorrhaphy was performed bilaterally. Preoperative vision was light perception in both eyes. KPro type I was implanted in the right eye (b, d). Visual acuity improved to 20/60 and was maintained at this level up to the last available follow-up (18 months)
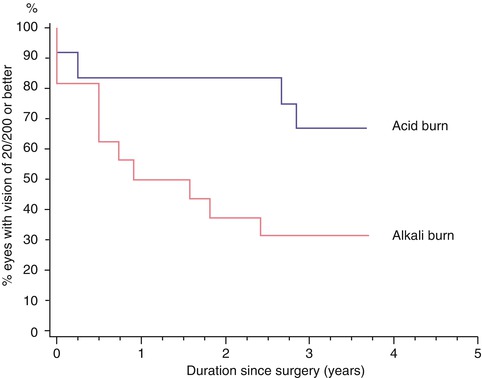
Fig. 7.5
Kaplan-Meier survival analysis of 28 eyes with chemical burns. In this study, Cade et al. compare the survival of ambulatory vision of 20/200 or better between 12 eyes with acid burns (blue) and 16 eyes with alkali burns (red) [10]. Glaucoma progression and retinal detachments were the most common causes of visual decline (Reprinted with permission from Lippincott Williams & Wilkins Inc.)
7.5.1.3 Multiple Graft Failures
Standard corneal transplantation remains the preferred approach in the management of corneal blindness. However, the long-term outcomes of repeat PKP are especially disappointing. Only 20–64 % of repeat grafts survive at 5 years and 11–41 % survive at 10 years [25–30]. Lower survival is seen with each subsequent regraft [28]. Repeating standard PKP in eyes at high risk for graft failure places additional strain on the already limited resources of corneal donor tissue. In this context, KPro appears to be reasonable alternative to further PKP. Prior failed graft was the most common indication for KPro in all of the most recent case series (Table 7.1) [12, 31–36]. These case series have demonstrated the safety and efficacy of KPro type I for the visual rehabilitation of the eyes with multiple graft failures.
Table 7.1
Summary data from multicenter and single-center Boston Keratoprosthesis case series that included all preoperative diagnostic categories
Zerbe (2006) [31] | Chew (2009) [36] | Aldave (2009) [12] | Dunlap (2010) [32] | Robert (2011) [33] | Greiner (2011) [34] | Patel (2011) [35] | International (2012) [80] | |
|---|---|---|---|---|---|---|---|---|
# eyes | 136 | 37 | 50 | 126 | 47 | 40 | 58 | 107 |
Prior failed graft, % | 54 | 78 | 84 | 89 | 57 | 48 | 81 | 44 |
Preoperative diagnosesa | ||||||||
SJS/TEN | 1 | 3 | 8 | 1 (0/7) | 2 (0/5) | 2.5 (0/5) | 0 | 8 |
MMP | 4 | 5 | 2 | 4 (3/14) | 0 | 2.5 (0/5) | 2 (2/18) | 5 |
Chemical injury | 15 | 5 | 10 | 4 (1/29) | 9 (15/0) | 25 (0/48) | 5 (4/9) | 27 |
ABK/PBK | 14 | 41 | NS | 28 (30/14) | 9 (11/10) | 0 | 17 (19/9) | NS |
# prior PKP | 2.24 | 1.9 | 2.3 | NS | 1.2 | 1.4 | 2.4 | NS |
Preoperative VA | ||||||||
Median | HM | CF | NS | HM | CF | CF | HM | |
(Range) | (20/100 – LP) | (20/100 – LP) | (20/200 – LP) | (20/100 – LP) | (20/150 – LP) | (20/200 – LP) | (20/100 – LP) | |
% eyes with VA | 99 | 100 | 96 | 98 | 98 | |||
≤ 20/200 | ||||||||
7.5.2 Expanding Indications
7.5.2.1 Primary KPro
Patients with a poor prognosis following traditional PKP and patients that are unable to tolerate the systemic immunosuppression (SI) needed for LSCT are considered to be good candidates for KPro implantation as a primary procedure. KPro holds the benefits of rapidly providing a clear and astigmatically neutral visual axis while sparing the patient from the hazards of multiple repeated PKPs and long-term systemic immunosuppression (SI).
The potential indications for KPro haveexpanded with reports in the recent literature showing good anatomical and visual outcomes in eyes with various pathologies (Table 7.2). Kang et al. have demonstrated that for eyes with selected preoperative diagnoses, the survival rate of primary KPro compares favorably with those of PKP and LSCT [3]. However, it is important to note that despite promising case reports and small series, larger cohorts with longer-term follow-up are needed to clarify the role of KPro in such populations.
Table 7.2
Results of Boston Keratoprosthesis case series for specific diagnoses
Diagnosis | # eyes | KPro type I, % | Device retention rate, % | Postoperative VAa | Follow-up, mean (range) | |
|---|---|---|---|---|---|---|
Sayegh (2008) [18] | SJS/TEN | 16 | 37 | 100 | 50 % ≥ 20/40 (BA) | 3.6 yrs (10 mo–5.6 yrs) |
75 % ≥ 20/200 (BA) | ||||||
Pujari (2011) [23] | SJS/TEN | 12 | 0 | 50 | 0.91 (CFS) | 107.9 person-yrs |
MMP | 15 | 0 | 60 | 0.64 (CFS) | ||
SJS/TEN/MMP combined | ||||||
34.5 % ≥ 20/30 (BA) | ||||||
79.3 % ≥ 20/200 (BA) | ||||||
Cade (2011) [11] | Chemical burns (16 alkali; 12 acid) | 28 | 82 | 75 (overall) | (20/20 – NLP) | 57 mo (1–162 mo) |
78 (type I) | 61 % ≥ 20/60 (BA) | |||||
32 % ≥ 20/60 (LF) | ||||||
60 (type II) | 79 % ≥ 20/200 (BA) | |||||
46 % ≥ 20/200 (LF) | ||||||
Harissi-Dagher (2008) [24] | Severe trauma (70 % chemical burns) | 30 | 100 | 90 | 20/80 (20/20 – NLP) | 35 mo (1–108 mo) |
77 % ≥ 20/200 (BA) | ||||||
53 % ≥ 20/60 (BA) | ||||||
Kang (2012) [3] | Primary KPro | 21 | 90 | 91 | 71.4 % ≥ 20/200 (LF) | 15 mo (6–36 mo) |
19 % ≥ 20/40 (LF) | ||||||
Sejpal (2011) [38] | LSCD | 23 | 100 | 75 | 69 % ≥ 20/50 (1 yr) | 22.1 mo (0.5–59 mo) |
89 (excluding SJS) | 88 % ≥ 20/50 (2 yrs) | |||||
67 % ≥ 20/50 (3 yrs) | ||||||
Basu (2012) [39] | LSCD | 8 | 100 | 100 | 20/40 (LF) | 8 mo (6–9 mo) |
(20/25–20/200) (LF) | ||||||
63 % ≥ 20/40 (6 mo) | ||||||
Hou (2012) [41] | Failed PKP after KLAL | 7 | 100 | 85.7 | 20/400 (LF) | 19.5 mo |
(20/25 – CF at 3 ft) (LF) | ||||||
43 % ≥ 20/200 (LF) | ||||||
Akpek (2007) [44] | Aniridia | 16 | 100 | 100 | 20/200 (20/60 – HM) (LF) | 17 mo (2–85 mo) |
63 % ≥ 20/200 (LF) | ||||||
Bakhtiari (2012) [47] | Aniridic fibrosis syndrome | 9 | 100 | 100 | 20/400 (BA) | 26 mo (6–48 mo) |
(20/200 – CF at 2 ft) (BA) | ||||||
Yildiz (2010) [50] | Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy | 2 | 100 | 100 | 20/25–20/40 (LF) | 2 yrs |
Khan (2007) [55] | Herpetic keratitis | 17 | 100 | 100 | 88 %: 20/25–20/70 (BA) | 14 mo (6–72 mo) |
73 %: 20/25–20/70 (LF) | ||||||
Utine (2010) [59] | Chronic hypotony and corneal opacity
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|