Imaging Modalities in Ophthalmology
14.1 PLAIN FILMS
Description
Images of radiopaque tissues obtained by exposure of special photographic plates to ionizing radiation.
Uses in Ophthalmology
May be used to identify or exclude radiopaque intraorbital or intraocular foreign bodies. However, computed tomography (CT) is the study of choice to evaluate for foreign bodies, as CT has greater contrast sensitivity over radiography. Plain films remain a valid screening modality before magnetic resonance imaging (MRI) if an occult metallic foreign body is suspected. Plain films should not be used for the diagnosis of orbital fractures.
14.2 COMPUTED TOMOGRAPHY
Description
CT uses ionizing radiation and computer-assisted formatting to produce multiple cross-sectional planar images. Possible image planes include axial, direct coronal, reformatted coronal, and reformatted parasagittal images. Bone and soft-tissue windows should always be reviewed in both axial and coronal orientations (see Figures 14.2.1–14.2.3). Orbital studies use 3-mm or thinner slices. Radiopaque iodinated contrast allows more extensive evaluation of vascular structures and areas where there is a breakdown of the normal capillary endothelial barrier (as in inflammation).

FIGURE 14.2.1. Axial soft-tissue window of inferior orbit shows abnormality, which is difficult to assess.

FIGURE 14.2.2. Coronal soft-tissue window shows a large blowout fracture of the orbital floor. This finding could have been missed on axial study, demonstrating the importance of reviewing both axial and coronal images.
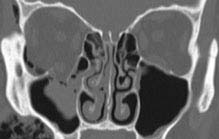
FIGURE 14.2.3. Coronal bone window shows the fracture again. In bone windows, the soft-tissue detail fades, but bone detail is enhanced, allowing for better examination of bony anatomy.
Uses in Ophthalmology
1. Excellent for defining bone abnormalities such as fractures (orbital wall or optic canal), calcification, or bony involvement of a soft-tissue mass.
2. Locating suspected intraorbital or intraocular metallic foreign bodies. Glass, wood, and plastic are less radiopaque and therefore more difficult to isolate on CT.
3. Soft-tissue windows are good for determining some pathologic features, including orbital cellulitis/abscess, noninfectious inflammation, and tumors. May be useful in determining posterior scleral rupture when clinical examination is inconclusive, but B-scan ultrasonography may be more sensitive.
4. Excellent for imaging paranasal sinus anatomy and disease.
5. Head CT helpful for locating parenchymal, subarachnoid, subdural, epidural, and retrobulbar hemorrhage in either acute or subacute setting.
6. Imaging modality of choice for thyroid-related orbitopathy. See 7.2.1, Thyroid Eye Disease.
7. Any loss of consciousness requires CT of the brain. CT of the brain does not provide adequate detail of the orbital anatomy, and vice versa.
Guidelines for Ordering an Orbital Study
1. Always order a dedicated orbital study if ocular or orbital pathology is suspected. Always include views of paranasal sinuses and cavernous sinuses.
2. Order both axial and coronal views.
3. When evaluating traumatic optic neuropathy, request 1-mm cuts of the orbital apex and optic canal to rule out bony impingement of the optic nerve.
4. When attempting to localize ocular or orbital foreign bodies, order 1-mm cuts.
5. Contrast may be necessary for suspected infections or inflammatory conditions. Contrast is helpful in distinguishing orbital cellulitis from abscess. However, contrast is not mandatory to rule out orbital inflammation or postseptal involvement. Relative contraindications for contrast include renal failure, diabetes, congestive heart failure, myeloma, sickle cell disease, multiple severe allergies, and asthma. Check renal function in patients in whom renal insufficiency is suspected.
NOTE: The radiologist may recommend premedication with corticosteroids if contrast is required and a prior allergy is suspected. Follow the protocol recommended by your radiology department.
6. Obtain pregnancy test before obtaining CT scans in females of childbearing age if possible.
7. CT angiography (CTA) is helpful in diagnosing intracranial vascular pathology, including aneurysms. It is available on all multidetector CT scanners and in general is more sensitive than magnetic resonance angiography (MRA). However, it requires the use of intravenous iodinated contrast.
8. CT scans may be obtained in children with careful consideration of the risk of radiation exposure versus benefits of performing the scan. Each CT scan exposes children to radiation with a cumulative risk over their lifetime. Radiation exposure from CT scans in children is of particular concern when serial imaging is required. In these cases, MRI is often a better choice for children, although sedation may be needed.
NOTE: Many radiology centers have pediatric protocols for CT scans that limit the amount of radiation exposure. If available, these should be considered when imaging children.
14.3 MAGNETIC RESONANCE IMAGING
Description
1. MRI uses a large magnetic field to excite protons of water molecules. The energy given off as the protons reequilibrate to their normal state is detected by specialized receivers (coils) and that information is reconstructed into a computer image.
2. Obtains multiplanar images without loss of resolution.
3. The basic principles of MRI are listed in Table 14.3.1. Figures 14.3.1 to 14.3.3 provide specific examples.
TABLE 14.3.1 Summary of MRI Sequencesa
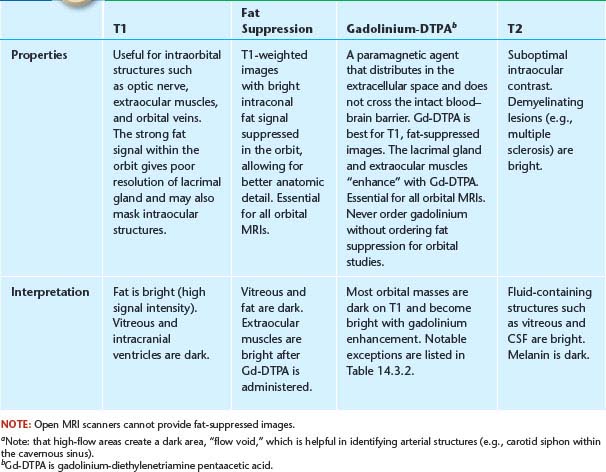
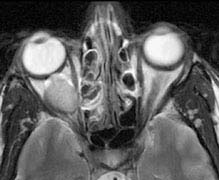
FIGURE 14.3.3. Axial T-2-weighted image. The vitreous is hyperintense (bright) relative to the orbital fat. The lesion is also bright but in some cases may be isointense with the surrounding fat.

FIGURE 14.3.1. Axial T-1-weighted image without fat suppression or gadolinium. The vitreous is dark (hypointense) relative to the bright signal from fat. A well-circumscribed mass is clearly visible in the right orbit, also hypointense. Most orbital lesions are dark in T1 prior to gadolinium injection. The notable exceptions are listed in Table 14.3.2.
TABLE 14.3.2 Tissues/Lesions That Appear Bright (Hyperintense) Relative to Vitreous Before Gadolinium Injection
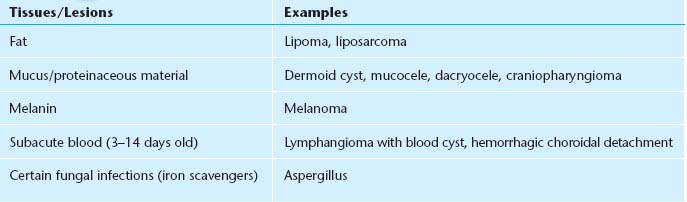

FIGURE 14.3.2. Axial T-1 image with fat suppression and gadolinium. Note how both the vitreous and fat are dark, but the extraocular muscles become bright. The orbital mass is now clearly visible. This technique should be performed in all orbital MRIs.
4. Contrast studies can be ordered using gadolinium, a well-tolerated non–iodine-based paramagnetic agent.
Uses in Ophthalmology
1. Excellent for defining the extent of orbital/central nervous system masses. Signal-specific properties of certain pathology may be helpful in diagnosis (see Table 14.3.2).
2. Poor bone definition (e.g., fractures).
3. Excellent for diagnosing intracranial, cavernous sinus, and orbital apex lesions, many of which affect neuro-ophthalmic pathways.
4. For suspected neurogenic tumors (meningioma, glioma), gadolinium is essential in defining lesion extent.
5. All patients with clinical signs or symptomatic optic neuritis from suspected demyelinating disease should undergo brain MRI [fluid-attenuated inversion recovery (FLAIR) images are especially useful]. See Figure 14.3.4 and 10.14, Optic Neuritis.
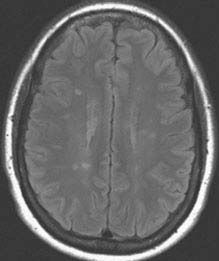
FIGURE 14.3.4. MRI with FLAIR sequence of demyelinating lesions in multiple sclerosis.
6. Fat suppression should always be used in conjunction with intravenous gadolinium to enhance the visualization of the underlying pathology (e.g., optic neuritis, fat-containing lesions).
7. Diffusion-weighted imaging can help differentiate the various phases of cerebral infarction (e.g., hyperacute, acute, subacute, and chronic).
Guidelines for Ordering the Study
1. For the vast majority of orbital studies, a head coil is indicated to provide bilateral orbital views extending to the optic chiasm.
2. Intravenous gadolinium is useful for augmenting ocular, orbital, and perineural masses. In patients who have kidney failure, nephrogenic systemic fibrosis is a rare complication of gadolinium that occurs weeks to months after administration. It is characterized by a thickening and hardening of the skin, especially over extremities and trunk. There is no known proven therapy. Evaluate renal function in patients in whom renal insufficiency is suspected.
3. Contraindications to MRI: Severe claustrophobia, marked obesity, cardiac pacemakers, some cardiac valves, suspected magnetic intraocular/intraorbital foreign bodies, spinal stimulators, vagal nerve stimulators, stapes implants, and specific breast and penile implants. Titanium plates and newer aneurysm clips are MRI safe as are gold weights placed in the eyelids. When in doubt, ask the radiologist to look up the specific device in an MRI safety catalog. Any patient with a poorly documented implanted device should NOT be scanned with MRI.
14.4 MAGNETIC RESONANCE ANGIOGRAPHY
Description
Special application of MRI technology in which signal from flowing blood is augmented while signal from stationary tissues is suppressed. MRA allows for three-dimensional rotational reconstruction.
Uses in Ophthalmology
1. Suspected carotid stenosis, occlusion, or dissection.
2. Suspected intracranial and orbital arterial aneurysms (e.g., pupil involving third cranial nerve palsy), arteriovenous malformations, and acquired arteriovenous communications.
3. Suspected orbital or intracranial vascular mass. Note that MRA is best for imaging high-flow and large-caliber lesions. Lower-flow lesions (e.g., varix) are not well seen. MRA also has limited potential in visualizing cavernous sinus fistulas; color Doppler studies and conventional arteriography are more sensitive in making this diagnosis.
Guidelines for Ordering the Study
Cerebral arteriography remains the gold standard for diagnosis of vascular lesions but carries significant morbidity and mortality in certain populations. Currently, the limit of MRA is an aneurysm larger than 2 mm. However, the sensitivity is highly dependent on several factors: hardware, software, and the experience of the neuroradiologist. Despite these potential limitations, MRA remains a safe and sensitive screening test, especially when coupled with MRI for concomitant soft-tissue imaging. CTA in many situations can provide a suitable replacement for conventional angiography.
14.5 MAGNETIC RESONANCE VENOGRAPHY
Magnetic resonance venography is helpful in diagnosing venous thrombosis. MRI and magnetic resonance venography are an essential part of the workup of any patient presenting with bilateral optic disc swelling. See 10.15, Papilledema.
14.6 CEREBRAL ARTERIOGRAPHY
Description
This interventional examination entails intra-arterial injection of radiopaque contrast followed by rapid-sequence x-ray imaging of the region of interest to evaluate the transit of blood through the regional vasculature. Unlike MRA or CTA, catheter arteriography allows the option of simultaneous treatment of lesions by intravascular techniques. Arteriography is the gold standard for diagnosing intracranial aneurysms but is being replaced in many centers by CTA.
Uses in Ophthalmology
1. Suspected arteriovenous malformations, carotid cavernous fistulas, cavernous sinus fistula, and vascular masses (e.g., hemangioma, varix).
2. Evaluation of ocular ischemic syndrome or amaurosis fugax due to suspected atherosclerotic carotid, aortic arch, or ophthalmic artery occlusive disease. Usually carotid Doppler US, MRA, or CTA is adequate for diagnosis.
NOTE: Conventional arteriography is contraindicated in patients with suspected carotid artery dissection (catheter placement may propagate the dissection).
14.7 NUCLEAR MEDICINE
Description
Nuclear medicine imaging uses radioactive contrast (radionuclide) that emits gamma radiation, which is then gathered by a gamma ray detector. The classic types of radionuclide scanning known to ophthalmologists include bone scanning, liver–spleen scanning, and gallium scanning. Positron emission tomography (PET) is useful in determining metabolic activity within a lesion and may be coupled with CT for anatomic detail.
Uses in Ophthalmology
1. Scintigraphy (e.g., with technetium-99): Useful for assessing lacrimal drainage physiology in patients with contradictory or inconsistent irrigation testing.
2. Systemic gallium scan: Useful for detecting extraocular sarcoidosis and Sjogren syndrome.
3. Technetium 99m-tagged red blood cell study: Occasionally used to distinguish cavernous hemangioma/hemangiopericytoma from other solid masses in the orbit.
4. PET: The use of PET for the diagnosis and management of orbital disease is still an evolving technique. Limitations in this area include the high background metabolic activity of the adjacent brain which may mask orbital abnormalities, the size of the orbital pathology (current PET scanners have a resolution of about 7 mm), and the relatively indolent nature of most orbital lymphomas (decreasing the intensity of the signal on PET). PET is extremely useful in the diagnosis and surveillance of systemic pathologies, including lymphoma and metastases, and at present, this remains the primary role of PET in the management of orbital disease.
14.8 OPHTHALMIC ULTRASONOGRAPHY
A-SCAN
Description
(See Figure 14.8.1.)
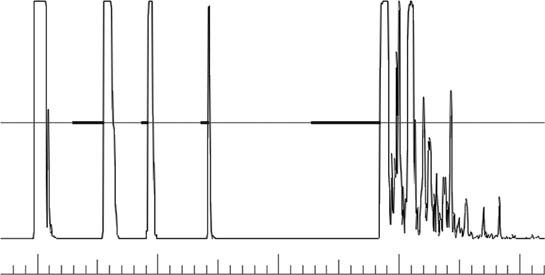
FIGURE 14.8.1. Normal A-scan US.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


