9

Hyperfunctional Facial Lines
Facial aging is a multifactorial process involving changes to skin, subcutaneous fat, muscle, and the underlying facial skeleton. Notable among these changes are hyperfunctional facial lines, rhytides, which develop with repetitive muscle activity. Over time, these lines deepen and remain apparent, even when the underlying musculature is relaxed. Both photodamage and smoking significantly accelerate these changes.
The ability of botulinum neurotoxin (BoNT) to reduce the appearance of facial lines was first noted in patients receiving treatment for hyperfunctional disorders such as hemifacial spasm and blepharospasm. Subsequent placebo-controlled studies confirmed the safety and efficacy of botulinum neurotoxin type A (BoNT/A) for the reduction of dynamic upper facial lines.1,2 BoNT/A (Botox Cosmetic; Allergan, Irving, CA) was approved by the Food and Drug Administration (FDA) in 2002 for the temporary treatment of moderate to severe glabellar lines, and this remains the only FDA-approved cosmetic indication for both onabotulinumtoxinA (Botox) and abobotulinumtoxinA (Dysport; Medicis Pharmaceutical, Scottsdale, AZ). Data from the American Society for Aesthetic Plastic Surgery 2010 database indicates that treatment with BoNT/A for the reduction of facial lines is currently the most common aesthetic procedure in the United States, and its use has increased 50% during the 8-year survey period from 2002 to 2010. In 2010, 2.4 million procedures were performed with BoNT/A and 1.3 million procedures were performed with hyaluronic acid fillers, which together accounted for approximately 65% of all nonsurgical cosmetic procedures performed that year.3
There is now a substantial body of evidence supporting the safety and efficacy of BoNT/A for reduction of dynamic upper facial lines. However, extensive clinical experience has shown both BoNT/A and BoNT/B to be highly efficacious primary or adjunctive treatments of not just glabellar rhytides, but also rhytides associated with hyperfunctional frontalis, orbicularis oculi, nasalis, orbicularis oris, depressor anguli oris, mentalis, and platysma muscles. It is also effective at reducing brow ptosis and the appearance of a hypertrophic pretarsal orbicularis oculi muscle.4–7 In addition to the reduction of dynamic facial lines, recent research suggests that mild glabellar lines in repose are also reduced, although the mechanism of this “smoothing” phenomenon is not completely understood.8
Reduction of dynamic facial lines may result in a more youthful appearance, as well as decreased inaccurate social interpretation of facial gestures suggesting anger or frustration. The goal of BoNT/A treatment is not only to reduce the appearance of rhytides, but also to prevent the development of deep rhytides and thereby delay or avoid more invasive rejuvenation procedures. Based on an expanded facial rejuvenation paradigm incorporating three-dimensional volume restoration, BoNT/A is frequently used in conjunction with dermal fillers to meld facial movement control, recontouring, and volume enhancement to provide a more relaxed, youthful appearance.4
 Workup
Workup
Patients should be interviewed regarding their medical history, medications, and prior cosmetic or reconstructive surgery. BoNT injection is contraindicated in patients with infection at the injection site, in patients with a known hypersensitivity to any ingredient in the formulation (including human albumin, saline, milk [abobotulinumtoxinA only]), in those receiving aminoglycosides, and in pregnant or lactating women. BoNT injection is relatively contraindicated in patients with disorders of the neuromuscular junction, myasthenia gravis, motor neuron disease, or Eaton-Lambert syndrome.9 Furthermore, caution should be exercised in those patients with surgical alteration of facial anatomy, excessive dermatochalasis, and deep dermal scarring, as the effect of BoNT/A may be limited regarding the desired cosmetic outcome. Patients with active viral or bacterial illness have higher levels of circulating antibodies, which may decrease the efficacy of BoNT/A. Therefore, we recommend against BoNT/A injections in the setting of infection.
 Botulinum Neurotoxin Formulations
Botulinum Neurotoxin Formulations
Both BoNT/A (Botox, Dysport) and BoNT/B (Myobloc [rimabotulinumtoxinB]; Solstice Neurosciences, Inc., South San Francisco, CA) are approved for cosmetic use. InconobotulinumtoxinA (Xeomin; Merz Pharmaceuticals, Greensboro, NC) is not approved for cosmetic use. Although Botox/Dysport conversion ratios of 1:2.5, 1:3, and 1:4 have been reported in the literature, it is important to note that potency units for BoNT products are specific to each preparation, and are not interchangeable.4 BoNT/B is generally considered less suitable for cosmetic use due to pain at the injection site due to low pH and shorter duration of effect.4,10 Compared with Botox, Dysport may have a larger diffusion radius.11
General Considerations
Treatment planning and goals must be individualized according to specific anatomic variables including the location and depth of rhytids, size and position of facial musculature, brow position, eye shape, and skin type, as well as individual characteristic facial gestures and ethnic background. Examination during muscle activation as well as during repose is required to appreciate the contributions of the various muscles to facial rhytides. It should be noted that substantial differences exist between various ethnic aesthetic ideals. Therefore, additional treatment planning and customization may be required with different ethnic groups. Clarifying goals, addressing anxieties, and dispelling misconceptions regarding the effects of BoNT/A are particularly important components of every consultation.
Most practitioners counsel the patient regarding the previously mentioned factors, as well as the role of dermal fillers in facial volume contouring, so that realistic goals and expectations may be established prior to initiating treatment with BoNT/A alone or in conjunction with other nonsurgical procedures. Although this chapter does not discuss volume contouring, the clinician is encouraged to become familiar with its use.
Doses are basic guidelines that should be modified based on individual anatomy, patient preference, and clinician judgment. For BoNT/A, the solution is reconstituted according the standard formulation of 4 mL of saline per bottle, yielding 2.5 units (U) per 0.1 cc. These injections are typically performed using a 1.0-cc tuberculin syringe. An alternative reconstitution strategy is to use 1 mL of saline per 100-U bottle, yielding 1 U per 0.01 cc, injected with a 0.1-cc syringe. This technique creates smaller injection aliquots, which decreases the appearance of the bolus at the injection sites. The choice of the injection needle and syringe depends on the individual technique as well as on the specific application. Most practitioners use 29- to 32-gauge, ½- to 1¼-inch needles with 1-cc tuberculin syringes, 0.3-cc syringes, or 0.1-cc syringes (BD Medical, Franklin Lakes, NJ). The 0.1-cc syringes are particularly suited for use with the 1 U/0.01 cc dilution. Smaller gauge needles decrease injection pain, but become dull sooner, with subsequent loss of this advantage after multiple injections.
Although topical anesthesia is generally not required, some practitioners may use topical anesthetic such as lidocaine, ice, or massagers such as the Buzzy (MMJ Laboratories, 32 Sutherland Place NE, Atlanta, GA 30307) for vibration anesthesia in sensitive areas.
The depth of injection depends on the thickness of the skin, the amount of subcutaneous adipose tissue, and the size of the injected muscle. Most cosmetic injections do not require electromyographic (EMG) guidance, but it may be helpful in locating deeper or thinner muscles, such as the risorius or platysma.9
Complications of cosmetic BoNT/A injection can be grouped into three categories: local, locoregional, and systemic. Local complications include pain, erythema, ecchymosis, and hematoma formation. Locoregional complications are related to excessive weakening of facial and neck musculature or diffusion of the BoNT/A to adjacent muscles, resulting in brow ptosis, eyelid ptosis, facial asymmetry, oral incompetence, dysarthria, and dysphagia. These complications are dose and technique related, and may be avoided by injection of small volumes and using EMG guidance, when necessary. Systemic complications, including fatigue, generalized weakness, and nausea, are extremely rare, even when larger doses are used.4 However, patients who receive large and frequent doses are at risk for developing neutralizing antibodies to the toxin, which will render the patient resistant to future BoNT/A therapy.12
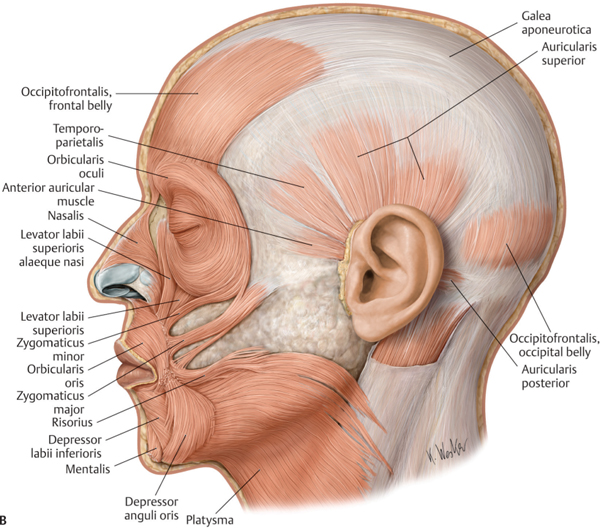
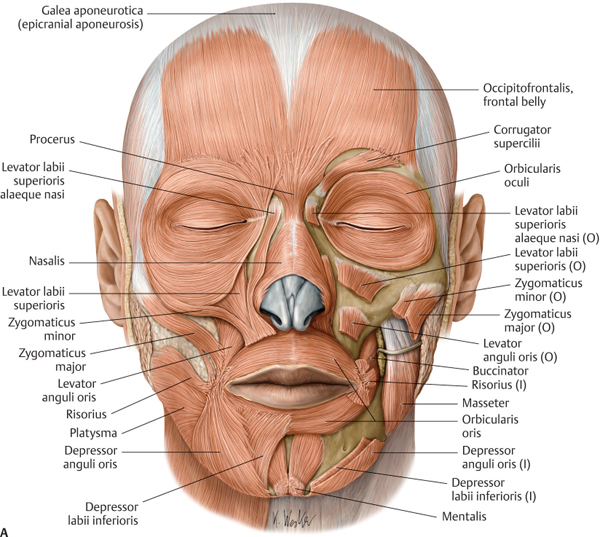
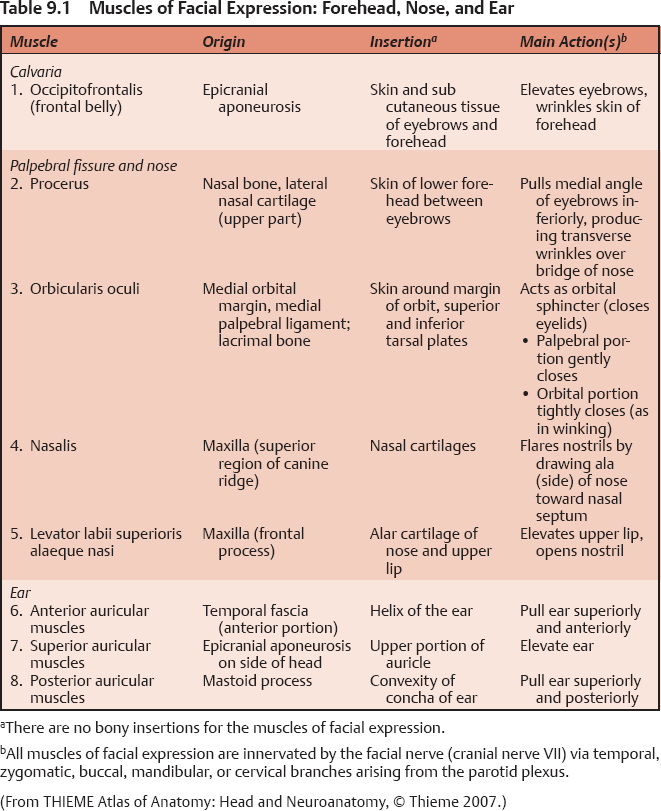
Fig. 9.1 (A-B) Muscles of facial expression. (From Atlas of Anatomy, © Thieme 2008, Illustration by Karl Wesker.)
Horizontal Forehead Lines
Anatomy
The frontalis muscle elevates the brows and the skin of the forehead, resulting in horizontal lines often associated with aging (Figs. 9.1 and 9.2; Table 9.1). Although BoNT/A injection of the frontalis muscle reduces the appearance of horizontal facial lines, if used without concurrent injection of the brow depressors (see Glabellar Lines, below) it may have the undesirable effect of lowering the brows.
Fig. 9.2 Occipitofrontalis muscle. (From Atlas of Anatomy, © Thieme 2008, Illustration by Karl Wesker.)
Technique
Four to eight points (1.5–2.5 U BoNT/A per point) are injected in a curved horizontal line or two rows for a large forehead, crossing both the medial and lateral fibers at least 1.5 cm above the brow (Fig. 9.3). Most practitioners now inject less BoNT/A in the frontalis muscle than they have in the past, thereby avoiding the “frozen face” look associated with paralysis of the frontalis muscle. Rather than immobilization, the goal of treatment should be a more relaxed, natural appearance. Typical starting doses for women range between 6 and 15 U, with men usually requiring higher doses of 6 to >15 U.
Follow-Up
If inadequate correction of horizontal forehead rhytids or overarching of the brows is noted, additional BoNT/A may be injected a minimum of 7 days after the initial injections, at which time the expected effect of the initial BoNT/A should be achieved.
Complications
Keep in mind that the frontalis muscle is a brow elevator, so keep the injection sites well above the brow and keep doses low to decrease the risk of brow ptosis. Doses greater than 20 U are more likely to result in complications. Brow ptosis may be managed with an additional corrugator injection or injection of the depressor supercilii directly below the brow.
The medial fibers of the frontalis are usually stronger than the lateral fibers. Isolated injection of the medial fibers can result in the overarched “Spock eyebrow” caused by unopposed lateral fiber compensation to medial fiber injection. This phenomenon may also be seen following glabellar injections, whereby the weakened brow depressors, the corrugator and procerus, are unable to counteract the unopposed lateral frontal fibers. Low-dose injections to the upper lateral frontalis muscle will correct this undesirable effect.
Upper eyelid ptosis (blepharoptosis) may occur if the lateral injection is performed too close to the eyebrow, and diffusion occurs into the levator palpebral superioris. This phenomenon may be avoided by applying digital pressure below the injection site to prevent migration of the bolus. Should blepharoptosis occur, it may be partially ameliorated with apraclonidine or phenylephrine ophthalmic drops, which stimulate Mueller’s muscle to elevate the upper eyelid. Most cases of blepharoptosis are mild to moderate and resolve within 2 to 3 weeks.13
Glabellar Lines
Anatomy
The glabellar complex is composed of the procerus, corrugator supercilii, depressor supercilii, and orbicularis oculi, all of which are brow depressors (Figs. 9.1 and 9.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree