Headache and facial pain are a common complaint in the otolaryngologist’s office. Ninety percent of Americans experience headache in their lifetime. Referral is often made to determine if headache is sinus in origin, but in this chapter we see that sinogenic causes of headache and facial pain are infrequent. Primary headache disorders are much more common. Secondary causes of headache and facial pain comprise an extensive list. The otolaryngologist should be able to identify sinus pathology and diagnose and treat other common causes of headache.
Headache and facial pain can be grouped into primary, secondary, and other etiologies. Primary headaches include migraines, tension-type, cluster headaches, and chronic daily headaches (CDHs). Other primary headache disorders are beyond the scope of this chapter. Secondary headaches include those that have specific etiologies identified. This group can include trauma, vascular disorders, infections, neuralgias, neoplastic causes, and others. Facial pain can be divided into peripheral or central causes. Peripheral facial pain makes up the larger of the two and includes disorders of the head and neck that refer pain to this region. Examples include temporomandibular joint (TMJ) syndrome and various neuralgias. Central facial pain is secondary to intracranial pathology like neoplasms or vascular disorders. For simplicity, secondary headache and peripheral facial pain disorders have been grouped together in this chapter.
ANATOMY AND PHYSIOLOGY
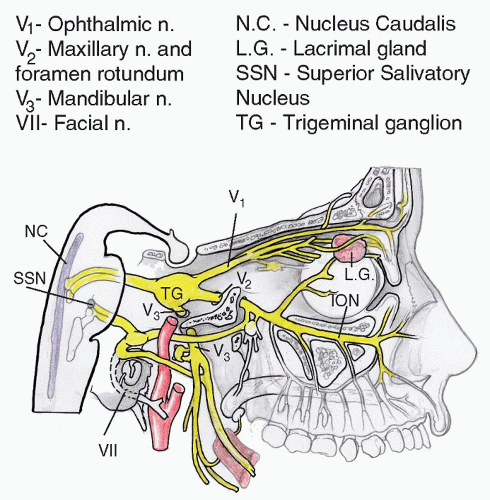
The brain is not a sensory organ and therefore does not perceive pain, but the surrounding structures in the brain have nociceptive fibers that recognize pain. Intracranial structures that are pain sensitive include major venous sinuses, large cerebral vessels, upper cervical nerves, and cranial nerves (CNs) V, VII, IX, and X. The trigeminal nerve and its branches provide the majority of the somatosensory innervation to the head and face region. The trigeminal nerve is a mixed nerve containing sensory and motor components. The nerve exits the ventrolateral aspect of the pons and divides into three main branches from the Gasserian ganglion; the ophthalmic V1, maxillary V2, and mandibular V3 divisions. Disease in the anterior or middle cranial fossa refers to the scalp or face anterior to the coronal suture. Lesions of the posterior fossa structures refer to the back of the head and upper neck. The sphenoid sinus and sella refer to the vertex of the head. Pain from diffuse intracranial disease may cause both anterior and posterior head pain (
1).
Electrical stimulation of the trigeminal ganglion causes a cascade of events that are thought to cause headache. These electrical impulses trigger neurogenic plasma extravasation. This initiates a sterile inflammatory response, which leads to pain. There is also an increase in extracerebral blood flow and release of calcitonin gene-related peptide (CGRP) and substance P (SP) (
2). CGRP is the most potent peptide vasodilator and its release causes vasodilation, mast cell degranulation, and plasma extravasation. SP is involved in inflammatory processes and pain perception. Pain impulses from the dilation and inflammation are transmitted from the trigeminal nerve to the trigeminal nucleus caudalis (TNC) in the brain stem. Because activation of the TNC can result in referred migraine pain to the ophthalmic and maxillary regions, patients may present with pain or pressure felt around the eyes and sinuses. The superior salvatory nucleus (SSN) that carries cranial parasympathetic fibers lies in close proximity to the TNC. Stimulation of the TNC can cause parasympathetic symptoms of rhinorrhea, congestion, and lacrimation. A form of central sensitization takes place during migraine, which is evident by symptoms of allodynia. Allodynia is a common finding of pain from non-noxious stimuli like touching the scalp or hair (
Fig. 19.1).
Depicted is the trigeminal nerve with its three major branches; ophthalmic, maxillary, and mandibular. The TNC is close to the superior salivary nucleus (SSN), which houses parasympathetic fibers. Activation of the TNC can cause reflex activation of the SSN giving rise to rhinorrhea, congestion, and lacrimation.
PRIMARY HEADACHES
Migraine is the most common primary headache and one of the leading causes of chronic illnesses and disability. Its prevalence is estimated at 18% of the US female population and 6% of the US male population (
3). Two-thirds of women experience migraine before or during menses and these can worsen early in pregnancy. There is a significant decrease in episode frequency after menopause. About 70% of sufferers have a first-degree relative with migraines.
Migraine headaches are recurrent attacks lasting 4 to 72 hours. They are usually unilateral, pulsatile in nature, and of moderate to severe intensity. Attacks are often aggravated by physical activity. They are associated with nausea and/or photophobia and phonophobia. Most patients report at least one trigger of their migraine headaches. Common precipitating factors are emotional stress, hormonal changes in women, fasting, weather changes, sleep disturbances, odors, and alcohol (
4).
Patients with migraine often have prodromal symptoms such as neck stiffness, euphoria, depression, fatigue, anorexia, food cravings, fluid retention, drowsiness, and enhanced alertness that begin 24 to 48 hours before the onset of headache. Fifteen to thirty percent of migraine sufferers have an aura preceding the pain. Auras are focal neurologic symptoms presenting as visual, motor, and sensory disturbances. Most auras develop slowly and may follow one another in succession starting with visual symptoms followed by sensory disturbances. Visual auras are most common and often present as zigzag figures near the point of fixation (fortification spectrum), moving geometric patterns, flashes of light, and scotomas. Sensory disturbances are frequently described as pins and needles affecting a small or large area of one side of the body and face. Numbness may also occur alone or in conjunction with other visual and sensory auras. Some patients experience a postdromal period where sudden head movements may precipitate short lasting pain in the location of the antecedent migraine headache. During this period, some patients feel tired and others have a sense of euphoria.
The diagnosis of migraine is clinical and relies on efficient history taking skills and detailed physical exam. The International Headache Society (IHS) divides migraines into two major subtypes; migraine without aura and migraine with aura. The latter is further subdivided into (i) typical aura with migraine headache, (ii) typical aura with nonmigraine headache, (iii) typical aura without headache, (iv) familial hemiplegic migraine, (v) sporadic hemiplegic migraine, (vi) basilar-type migraine. Each subtype has specific diagnostic criteria (
Table 19.1). There are no diagnostic tests for migraine and neuroimaging is not necessary in most patients. A head computed tomography scan (CT) or magnetic resonance image (MRI) should be obtained if there are unexplained abnormal findings on neurologic examination, rapidly increasing frequency of headaches and atypical headaches that do not fulfill the strict diagnostic criteria established by the IHS.
Treatment for migraine headaches consists of acute headache resolution, avoidance of known triggers, and prevention of subsequent events. For mild to moderate nondisabling pain, oral nonsteriodal anti-inflammatory drugs (NSAIDs), acetaminophen, and aspirin are appropriate first choice agents. Caffeine may enhance the effect of the medications. Some patients do not respond to mild analgesics and need specific abortive therapies for acute migraine attacks. The triptans are serotonin 1b/1d agonists that inhibit the release of vasoactive peptides, promote vasoconstriction, and block pain pathways in the brainstem. They are used in outpatient situations because they are available in oral preparations, nasal sprays, and subcutaneous injections (
Table 19.2).
Ergotamine and dihydroergotamine are other abortive therapies with similar pharmacology to the triptans, which are commonly used in emergency rooms and hospitalized patients. Ergots are serotonin 1b/d receptor and alpha-adrenergic receptor blockers that cause arterial and venous vasoconstriction. Dihydroergotamine is preferred over ergotamine for its safety profile. It is available for intravenous, intramuscular, subcutaneous, and intranasal use. Antiemetics are also used, alone or in combination with analgesics, for the treatment of acute migraine attacks. Commonly used agents include intravenous metoclopramide, intravenous and intramuscular chlorpromazine,
and prochlorperazine. Abortive therapy is more effective if given early in the course of the headache. Patients should be treated with the safest, least expensive medications and advance to migraine-specific alternatives if the initial treatment fails.
Preventive treatment for migraine headache is indicated when headaches become recurrent (greater than four headaches per month), long lasting (>12 hours), and interfere with daily activities. Commonly used therapies include antihypertensives, antidepressants, anticonvulsants, herbal remedies, and acupuncture. Botulinum toxin injection to
trigger points (
6) and surgical resection of trigger points like glabellar muscles and zygomaticotemporal branch of the trigeminal nerve are effective therapies for selected patients with moderate recurrent migraine that are difficult to manage with standard therapy (
7).
TENSION-TYPE HEADACHE
Tension-type headache (TTH) is the most common type of primary headache in the general population. Epidemiologic studies have shown prevalence as high as 80% between 20- and 40-year-olds. Women are affected more than males. TTH tends to peak in the fourth decade with decreasing prevalence with increasing age. Sustained contraction of pericranial muscles was believed to be the cause of TTH, but studies have failed to prove a causative relationship. Terms like stress headache and muscle-contraction headache have been abandoned. The pathogenesis of TTH is unclear and is likely multifactorial. In the episodic form there is activation of peripheral nociceptors around blood vessels in muscles and tendon insertion resulting in increased muscle tenderness and headaches. In the chronic form, general pain sensitivity in the central nervous system is increased due to repetitive and sustained pericranial myofascial nociceptor activation (
8).
TTH attacks are mild to moderate in intensity and are usually less debilitating than migraine attacks. The pain is constant, nonthrobbing, and localized to the occipitonuchal or bifrontal regions bilaterally. It is often described as tightness, fullness, or “viselike.” Attacks are variable in duration, lasting from 30 minutes to 7 days. They are not associated with prodromal periods or auras. Nausea and vomiting are extremely uncommon. Muscle tenderness in the head, neck, and shoulders are usually associated with the headaches and its intensity will parallel that of the attack.
The IHS divides TTHs into an episodic and chronic form, each with specific diagnostic criteria (
Table 19.3).
Patients with episodic TTH have fewer than 15 attacks per month and do not cause a significant impact in quality of life or performance. They are further subdivided into infrequent episodic TTH (less than one episode a month) or frequent episodic TTH (more than one, but less than 15 attacks per month). Individuals with chronic subtypes have more than 15 attacks per month. Chronic forms evolve from episodic forms and are associated with greater economic and personal costs.
Although TTHs are the most common primary headache, patients do not routinely seek medical attention. The history will reveal the quality and duration of the attacks. Physical exam will reveal normal blood pressure, oxygen saturation, and no neurologic deficits. Tenderness may be elicited in the scalp or neck muscles. As for all primary headaches there are no diagnostic tests available for TTH. Imaging of the brain is indicated if the pain is sudden and severe in order to exclude other conditions such as subarachnoid hemorrhage. Stress has been reported to be the most common precipitant of TTHs. Anxiety, poor posture, and depression have also been associated with the development of attacks. Attacks are not precipitated by food, weather changes, or exposure to noxious odors.
The treatment of TTHs ranges from nonpharmacologic therapies to use of potent analgesics. Over-the-counter analgesics (NSAIDs, aspirin, and acetaminophen) are considered first-line therapies and have been shown to be beneficial in most cases (
9). NSAID in combination with caffeine works better than NSAIDs alone, but carries a greater risk of side effects. Patients often try a number of medications before seeking medical attention. These medications should not be used more than 10 days a month to decrease the risk of medication overuse headaches. Preventive treatment of TTHs is indicated if the attacks are frequent, long lasting, or they have a significant impact on quality of life. Tricyclic antidepressants, \\serotonin-norepinephrine reuptake inhibitors, and anticonvulsant medications have been tried with variable success.