Gonioscopy
Ronald L. Fellman
George L. Spaeth
INTRODUCTION
Routine gonioscopy is an essential component of vision care. It remains a tremendously valuable diagnostic and therapeutic adjunct to ophthalmic care and is vital in order to classify glaucoma. With this is mind, the practice of gonioscopy should be at an all-time high considering angle-closure glaucoma causes blindness in more people worldwide than open-angle disease.1,2 However, a recent study of initial office visits for glaucoma in the United States found gonioscopy documented in only 46% of cases while evaluation of the disc was noted in 94%.3 A similar study in Britain documented gonioscopy in only 23% of subjects with glaucoma even though the majority of ophthalmologists thought it was necessary.4
Why is gonioscopy underutilized? Gonioscopy remains a lost art because there are typically no signs or symptoms associated with early angle compromise that prompt an angle examination. For example, in early angle-closure disease, the patient has no complaints, the slit-lamp examination usually appears normal and there is nothing to prompt the ophthalmologist to look at the angle. This is best exemplified by the fact that 80% of angle-closure glaucoma cases are asymptomatic: only 20% have the acute variant.5 The eye has an astounding anterior chamber angle reserve that may hide disease for years. However, when that is exhausted, glaucomatous field loss and elevated intraocular pressure (IOP) may rapidly progress.
Lack of routine gonioscopy often culminates in misdiagnosis, maloccurrence, and maltreatment. Routine gonioscopy detects early angle compromise in time to preserve vision in countless patients. This chapter is dedicated to that mission.
CLASSIC GONIOSCOPY AND ADJUNCTIVE METHODS OF CHAMBER EVALUATION
Classically, gonioscopy involves viewing the chamber angle through a goniolens or gonioprism. Twenty-first century gonioscopy offers much more. There are a plethora of gonioprisms and goniolenses to fit a variety of diagnostic and therapeutic tasks. In addition, the technological advances of ultrasound biomicroscopy (UBM), Scheimpflug photography, optical coherence tomography, and ophthalmic endoscopy augment our understanding of angle mechanics (Table 1). The ability to correlate classic gonioscopy with new imaging techniques of the chamber angle facilitates a better understanding of chamber angle anatomy, physiology, and pathophysiology.6
TABLE 1. Clinical Methods of Viewing the Anterior Chamber Angle | |||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||
These new clinical modalities inspire a modern-day definition of gonioscopy, namely: the evaluation and management of the eye based on the visualization of the anterior chamber angle constitute the field of gonioscopy. Gonioscopy currently consists of direct and indirect gonioscopic techniques performed with variable-sized gonioprisms, goniolenses, and viewing devices. Ophthalmic endoscopy is a relatively new technique that allows the surgeon to view the chamber angle directly during surgery. Imaging of the chamber angle with UBM and photography adds valuable angle information that is correlated with gonioscopy. Ophthalmologists who take advantage of these techniques and devices provide superior care through a rapid assessment of the angle situation. The focus of this chapter is classic gonioscopy, the benefits of which are currently the greatest for practitioners on a day-to-day clinical basis.
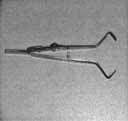
The ultimate goal of gonioscopy is to preserve or improve vision through the systematic evaluation and management of the anterior chamber angle. This requires the skill necessary to use a variety of instruments in order to accomplish a specific gonioscopic task (Fig. 1). In addition, the accurate recording and classification of visualized structures is imperative to document angle structures and note their changes over the lifetime of the patient. Physicians who integrate gonioscopy into their practice are able to examine, evaluate, document, and appreciate the appearance of the normal angle and its immense variability. A thorough understanding of normal is imperative in order to recognize and treat angle pathology.
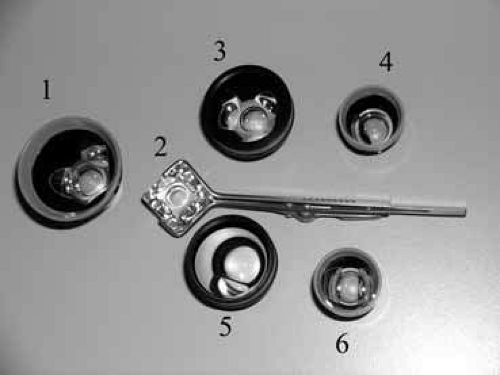 Fig. 1 It is desirable to master more than one gonioscopic instrument to diagnose and treat the anterior chamber angle accurately. One gonioscopic device is insufficient to diagnose and treat eye diseases related to the anterior chamber angle. This figure demonstrates several instruments used in the office. For example, the Zeiss or comparable lens, number 2, (Table 1, II), is best for obtaining a rapid painless view of the angle and is especially helpful for evaluating eyes with narrow angles; lens number 5 (Magna View lens, Ocular Instruments, Bellevue, WA) allows a magnified view of the angle greater than a Goldmann for trabeculoplasty (magnification 0.93 versus 1.3); the classic Goldmann lens, number 1, is excellent for residents learning gonioscopy because the lens allows a large 140-degree field of view and stabilizes the globe better than a Zeiss-type lens. Because of anatomic variation of the width of palpebral fissures, the construction and size of the contact diameter of the Goldmann lens varies from 13 to 18 mm. The smaller lenses have one or two mirrors. The authors typically use the following gonioscopy lenses: a Zeiss or equivalent lens, Goldmann lens (13 mm, 15 mm, 18 mm) and Magnaview lens (trabeculoplasty) in the clinic and a Koeppe (magnified view), Barkan (goniotomy), and Posner (able to autoclave) in the operating room. This totals eight different gonioscopy devices to perform the specific functions necessary to examine and treat the chamber angle on a daily basis. |
UNDERSTAND WHY THE ANTERIOR CHAMBER ANGLE CANNOT BE SEEN ROUTINELY: GEOMETRIC OPTICS AND SNELL’S LAW ARE THE ANSWER
A refresher course in geometric optics7 and limbal anatomy is a must for ophthalmologists who want to understand the inability to see the chamber angle. Understanding why the angle is ordinarily hidden should increase the desire to view it.
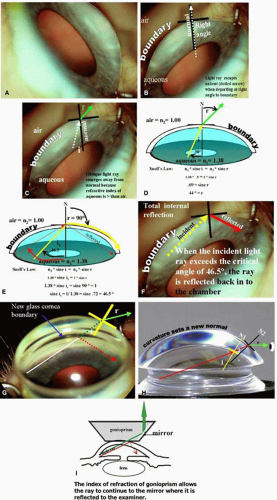
The optics of gonioscopy centers on the following point: how much and in which direction will a light ray bend as it emerges from the anterior chamber into air? Geometric optics revolves around constructing a normal to the interface; the normal is 90 degrees to the boundary interface. All the ray racings are based on the construction of this normal (Fig. 2).
LEARN THE NORMAL ANGLE LANDMARKS
Each and every angle is like a fingerprint, unique yet ordinary. It is imperative to understand the normal angle thoroughly. A comprehensive understanding of normal is mandatory in order to differentiate peripheral anterior synechiae (PAS) from iris processes, normal angle vessels from new angle vessels, plateau iris, a narrow angle, angle recession, a small cleft that causes hypotony, and countless others. The physician must appreciate normal angle variability in order to find early disease, yet at the same time avoid misdiagnosis and unnecessary treatment based on gonioscopic findings.
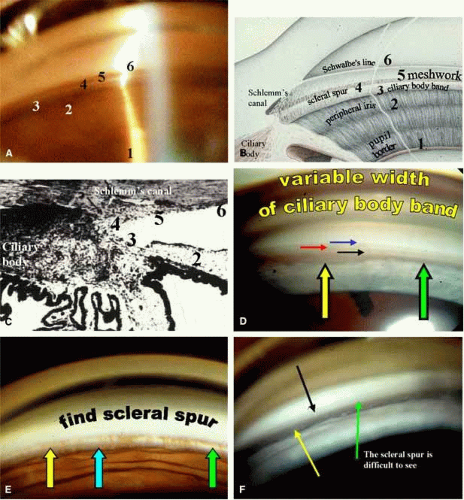
Gonioscopy requires a fusion of higher level skills including: hand–eye coordination, angle anatomy, physiology and pathophysiology of outflow structures and disease correlates, to name a few. There are several key landmarks that guide the gonioscopist through the iridocorneal angle in a systematic way; otherwise the angle loses its unique identity. The scleral spur is the visual landmark for maximum angle orientation. If the scleral spur is not located, suspect an abnormal angle or at least an unusual one. All outflow anterior to the spur is trabecular and the remaining uveoscleral outflow is posterior. Initially it is helpful to visualize the angle from a diagram that is correlated with a goniophotograph and then histophotograph (Fig. 3).
Initially gonioscopy should be performed in every apparently normal eye until familiar with normal. Physicians who look at the angle daily will rapidly become proficient at differentiating normal from abnormal in a matter of seconds. Others who only look at the angle when abnormality is suspected will take much longer and may never become efficient gonioscopists.
If possible, first find the scleral spur for rapid orientation. Then, to avoid confusion, observe the six structures in order from the iris to the cornea. If unable to find recognizable landmarks, look in another region of the angle.
Pupil Border
A scan across the chamber into the iridocorneal angle starts by looking for blood vessels, iris cysts, and dandruff-like particles in the pupillary border. If posterior chamber pathology such as misdirection, tumors, or cyclitic membranes is suspected, the pupil is dilated and gonioscopy repeated. The anatomy of the posterior chamber is easier to visualize with a gonioprism while the pupil is dilated. The fundus can also be viewed through the contact lens.
Peripheral Iris
Where the iris inserts onto the inner wall of the eye is identified, then the peripheral configuration of the iris is described and the angular approach of the iris to the cornea characterized. The peripheral iris may be flat, steep, or bow posterior; insertion is made anywhere from ciliary body to cornea with an angular approach of 0 degrees to 45 degrees.
Ciliary Body Band
The ciliary body band is that portion of the ciliary body muscle seen on gonioscopy (see Fig. 3D). The band is usually tan, gray, or dark brown, and typically narrow in hyperopes and wide in myopes. The root of the iris normally inserts onto the ciliary body band. If the iris inserts directly into the scleral spur, the ciliary body band is not seen easily.
Scleral Spur
The scleral spur is consistently the most notable landmark in the chamber angle (see Fig. 3E). Inability to locate the scleral spur is a cause for concern because obfuscation of the spur especially due to the peripheral iris is a tell tale sign of angle closure disease. The scleral spur appears as a white circumferential band. This white band represent the attachment of the ciliary body to the sclera and if found, the trabecular meshwork is directly anterior. The scleral spur separates conventional trabecular outflow from uveoscleral outflow and cyclodialysis clefts appear posterior to the spur.
Trabecular Meshwork
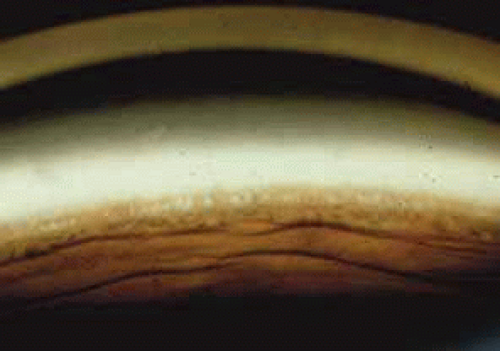
The trabecular meshwork extends from the scleral spur to Schwalbe’s line and typically has a ground-glass appearance best seen with sclerotic scatter. Pigment in the meshwork usually accumulates in the posterior division and facilitates identification. However, any angle structure may accumulate pigment. The junction of the mid and posterior meshwork is the favored location for trabeculoplasty. When there is no pigment in the meshwork, the ground-glass appearance is essential to define the outflow system and the corneal optical wedge is helpful in delineating nonpigment outflow systems (best seen with the Goldmann gonioprism).
Schwalbe’s Line
Schwalbe’s line is the termination of Descemet’s membrane and is the most anterior angle structure identifiable. Schwalbe’s line marks the forward limit of the trabecular meshwork and is easily identified where the anterior and posterior reflections of the corneal optical wedge meet.
NORMAL VARIABILITY OF THE CHAMBER ANGLE
Angle Vessels
There are certain features that differentiate normal from abnormal angle vessels. Normal angle vessels rarely bridge the scleral spur and do not branch. They are usually single vessels without arborization (Fig. 4). Normal angle vessels are seen in 62% of individuals with blue eyes and only 9% with brown eyes.8
Iris Processes
Iris processes (Fig. 5) may be confused with peripheral anterior synechiae. Iris processes are most common nasally and gradually diminish with increasing age.9
Schlemm’s Canal
The canal (Fig. 6) is located directly anterior to the scleral spur and is normally not seen. However, during gonioscopy, blood may reflux in to the canal exposing its dimensions. The canal is approximately 300 μm in width, 36 mm in length, and 30 μm in height.
Angle Pigmentation
A minimal amount of angle pigment is expected but excessive angle pigmentation should prompt the examiner to search for its cause (Fig. 7). This may be caused by pigmentary glaucoma, pseudoexfoliation, trauma, uveitis, or tumors.
 Fig. 7 Angle pigment. Excessive angle pigment always demands an explanation. It is common to see some pigment dusting the inferior portion of the angle, especially in individuals over age 50. Figure 3A reveals moderate trabecular pigment. Excessive trabecular pigment at the 12 o’clock position occurs in only 2.5% of individuals and is usually pathologic. This goniophotograph shows excessive trabecular pigment representing pigmentary dispersion syndrome.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|