10 
Definition
This chapter discusses glaucoma as a direct or indirect result of some lens abnormality. A careful assessment of this heterogeneous group of diseases will result in the selection of the appropriate management. This discussion does not include cases in which glaucoma and the lens pathology simply coexist and a cause-effect relationship is not present.1,2
How Is Glaucoma Associated with Lens Disorders Classified?
From a practical viewpoint these entities can be initially approached according to broad clinical features and then subdivided into more specific patterns of disease. We group together entities that have similarities either in their clinical picture or pathogenic mechanism. Accordingly, these glaucomas may be divided into four major categories: (1) glaucoma associated with ectopia lentis, (2) glaucoma associated with cataract, (3) glaucoma associated with exfoliation syndrome, and (4) glaucoma associated with aphakia and pseudophakia.
Frequent overlapping of clinical features and mechanisms of disease is commonly seen.2 As a result some clinical presentations fit more than one disease category. For example, an eye with phacolytic glaucoma may also have a dislocated lens and angle recession from prior trauma. It is understood that not all possibilities can be outlined separately, and more than one decision-making route may be needed to reach the proper diagnosis. Complex diseases are to be evaluated on a case-by-case basis. By using an approach based on questions and answers, this chapter guides the reader through the appropriate differential diagnosis to select the correct treatment.
Epidemiology and Importance
This is a very heterogeneous group of diseases that includes distinct hereditary and nonhereditary conditions. As a group they represent a small percentage of the total number of patients with glaucoma, but their impact on the health of the eye can be devastating if treatment is not instituted promptly.1 These patients usually present to ophthalmology clinics with a specific problem. With the exception of exfoliation syndrome, they are not the usual subjects for major population glaucoma studies. In general, the glaucoma associated with hereditary syndromes (e.g., homocystinuria, Weill-Marchesani syndrome) tends to present at an earlier age as the inborn lens abnormality progresses.2 These syndromes do not show a predilection for race or ethnic group and occur as a result of specific chromosomal abnormalities. Other entities, such as glaucomas associated with cataract or exfoliation syndrome, characteristically present in the elderly with variable severity. The presence of cataracts clearly increases with age,3 whereas the presence of exfoliation does show a predilection for certain ethnic backgrounds (see Glaucoma Associated with Exfoliation Syndrome, below).
GLAUCOMA ASSOCIATED WITH ECTOPIA LENTIS
Definition
What Is Glaucoma Associated with Ectopia Lentis?
This type of glaucoma is caused primarily by the abnormal position of the lens and its consequences.3 The various clinical conditions associated with ectopia lentis are listed in Table 10–1. Concurrent factors such as angle abnormalities or vitreous prolapse may play additional roles in the pathogenesis of the glaucoma.4
Isolated ectopia lentis |
Simple ectopia lentis |
Ectopia lentis et pupillae |
Systemic disorders |
Marfan syndrome* |
Homocystinuria* |
Weill-Marchesani syndrome* |
Hyperlysinemia |
Sulfite oxidase deficiency |
Ocular disorders |
Trauma |
Aniridia |
Megalocornea |
Others** |
aEntities only rarely associated with ectopia lentis are not considered in this list. |
Epidemiology and Importance
Congenital ectopia lentis is a rare condition, and Marfan syndrome, homocystinuria, and Weill-Marchesani syndrome represent more than 95% of cases. Marfan syndrome has a prevalence of 4 to 6 per 100,000,5 with 60 to 80% developing ectopia lentis. Homocystinuria is even more rare, having a frequency of 0.021% in the mentally retarded,5 with 90% developing ectopia lentis. Weill-Marchesani is more rare than Marfan and homocystinuria, and 80 to 90% of these patients develops ectopia lentis. Epidemiologic data on specific acquired conditions such as exfoliation syndrome will be mentioned when the pertinent entities are discussed.
Diagnosis and Differential Diagnosis
What Is the Pathogenesis of Glaucoma in Ectopia Lentis?
The following basic mechanisms of disease apply to most types of ectopia lentis (see Table 10–2). In general open-angle and angle-closure mechanisms can take place. Open-angle glaucoma has been divided in pretrabecular (usually membranes occluding the trabecular meshwork at the angle), trabecular (idiopathic and trabecular blockage by abnormal elements or distortion) and posttrabecular (Schlemm’s canal damage or elevated episcleral venous pressure). Angle closure can be caused by anterior (“pulling”) and posterior (“pushing”) forces, resulting in iris apposition to the cornea.1 Some specific differences will be pointed out when the pertinent entity is discussed.
Open-angle mechanisms consist of structural angle abnormalities and can contribute to the glaucoma in some syndromes.5 Pupillary-block angle closure is the most common mechanism and results from anterior displacement of the lens toward the pupil.2 The clinical presentation varies according to the degree and acuteness of the pupillary block. Therefore, acute, subacute, and chronic angle-closure glaucoma can occur. Vitreous prolapse around the dislocated lens can play an additional role in blocking the pupil and in some cases be the main factor.4 Total dislocation of the lens into the anterior chamber can occlude the pupil anteriorly causing an acute rise in intraocular pressure (IOP) (Tables 10–2 and 10–3). Finally, concurrent processes other than lens dislocation can contribute to the pathogenesis of glaucoma, such as trauma, hemorrhage, neovascularization, and cataract.
How Is Glaucoma in Ectopia Lentis Diagnosed?
The diagnosis of ectopia lentis begins with a good history and physical examination. A complete eye examination must be performed including a slit-lamp evaluation before and after maximal pupillary dilatation. After an initial external examination, a complete systemic workup is done to detect potentially serious conditions associated with ectopia lentis.5 The most noticeable conditions are cardiovascular complications in Marfan syndrome, and thromboembolic disease in homocystinuria (see below). Once a sustained elevation of IOP is documented, the diagnosis of ectopia lentis and glaucoma is made and the differential diagnosis can be outlined.
Open-angle mechanisms |
Pretrabecular |
Phacolytic |
Exfoliative |
Inflammatory elements |
Trabecular |
Trabecular trauma |
Trabecular inflammation |
Congenital anomaly* |
Angle-closure mechanisms |
Anterior type (“pulling”) |
PAS from trauma |
PAS from inflammation |
Posterior type (“pushing”) |
Pupillary block* |
Phacomorphic |
PAS, peripheral anterior synechiae. |
What Is the Differential Diagnosis of Glaucoma with Ectopia Lentis?
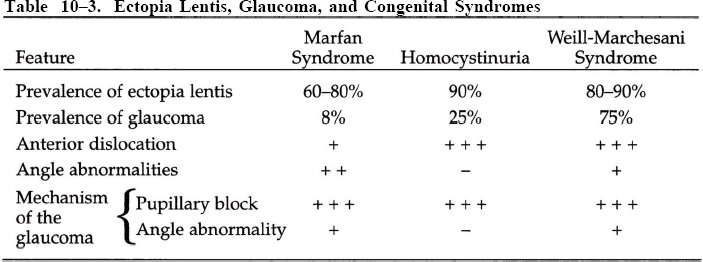
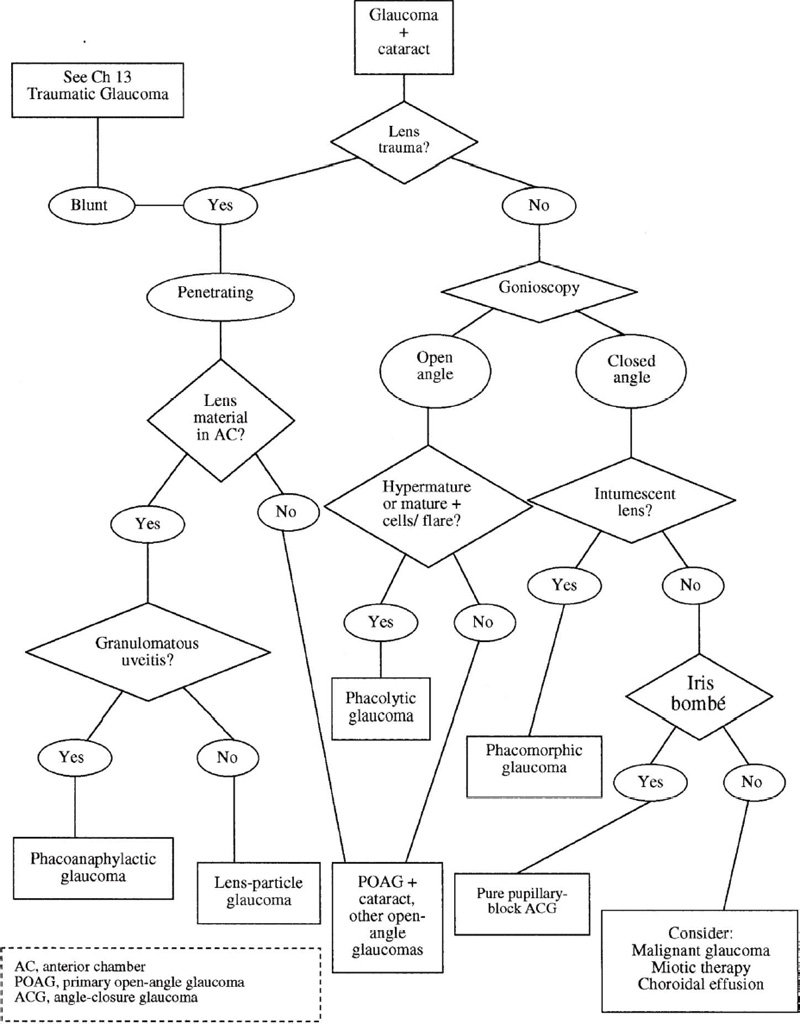
The list of all conditions associated with ectopia lentis is a long one;4 the most common ones are listed in Table 10–1. The differential diagnosis addresses the most common entities associated with glaucoma (Fig. 10–1).
Is There a History of Ocular Trauma?
The history of ocular trauma should be specifically sought, especially in cases of unilateral ectopia lentis and glaucoma. For a discussion of glaucoma associated with trauma see Chapter 13.
Figure 10–1. Glaucoma and ectopia lentis: differential diagnosis.
Can Ectopia Lentis be Nontraumatic?
For nontraumatic lens dislocations, the diagnostic workup of the glaucoma is similar in most entities.4,5
Are There Typical Systemic Abnormalities?
One must elicit a complete medical history to look for specific clinical features that are typical of syndromes associated with ectopia lentis. A referral for a comprehensive medical evaluation is essential. If systemic features are absent, the examination of the pupils will help narrow the differential diagnosis. These features are listed when each entity is addressed separately. One should know the typical clinical components of the most common systemic disorders associated with ectopia lentis as listed in Table 10–1. The importance of this assessment cannot be overemphasized because potentially serious systemic complications can be present when ectopia lentis is first diagnosed by the ophthalmologist. The occurrence and mechanisms of glaucoma in the most common congenital syndromes are compared in Table 10–3.
Are Both Pupils Eccentric (“Ectopic”)?
In this case, ectopia lentis et pupillae is the most likely diagnosis. This is an autosomal recessive condition in which both pupils are displaced in one direction and the lenses dislocated in the opposite direction. In some cases the lenses are small and spherical.5 Peripheral transillumination defects can be present in an iris that dilates poorly. Systemic abnormalities are usually absent. Glaucoma most commonly results from lens dislocation and secondary pupillary block.4–6 Concurrent ocular pathology includes cataract, severe axial myopia, and retinal detachment. Rarely, these patients may have marfanoid features.7
Are the Pupils in Normal Position?
If this is the case, exfoliation syndrome should be first excluded by careful anterior segment biomicroscopy. The presence of a dandruff-like material at the pupillary margin or lens surface and patchy pigment deposition at the angle will alert the examiner. In the absence of exfoliation, the diagnosis of simple ectopia lentis must be entertained. This syndrome is often inherited in an autosomal dominant fashion, although recessive transmission has been documented. The subluxation is usually bilateral, and sometimes asymmetric.1 The lenses are usually displaced superiorly and laterally and in severe cases they can dislocate into the anterior chamber.4,5 The dislocation can occur during the first decade (congenital type) or later in life (spontaneous type). Abnormalities in chromosome 15 (fibrillin gene) have been reported in a congenital case.8 A paucity of normal zonular fibers has been found in some cases.9 Glaucoma usually results from lens-induced secondary pupillary block in advanced stages10 and is more common in the late type of subluxation.5 Vitreous herniation can play a role in the pathogenesis of the pupillary block. When open, the anterior chamber angle has a normal appearance. Cataracts and retinal detachment can be present.4,5
Is Microspherophakia Present?
As the name implies, the lens diameter is decreased and the axial thickness is increased. The most common entity associated with microspherophakia is Weill-Marchesani syndrome.4 In addition, a hereditary combination of microspherophakia, ectopia lentis, and glaucoma has been recognized. This triad can also be associated with Marfan syndrome, homocystinuria, and other syndromes not usually linked to microspherophakia.5 Microspherophakia can also occur as an isolated feature.11
Does the Patient Have Systemic Features Typical of Weill-Marchesani Syndrome?
This autosomal recessive syndrome has striking phenotypic features that contrast with those seen in Marfan patients. Patients are short and stocky, with brachycephalia and a depressed nasal bridge. The hands and fingers are short and stubby, and the joints lack good mobility.5
What Is the Pathogenesis of the Glaucoma in Weill-Marchesani Syndrome?
Glaucoma occurs more often in Weill-Marchesani syndrome than in Marfan syndrome or homocystinuria,12,13 usually during the third or fourth decade of life. The dimensions of the lens (25% smaller, 25% thicker)4 create zonular elongation, rupture, and lens dislocation. Anterior migration of the lens usually induces glaucoma either by blocking the pupil posteriorly or by total luxation into the anterior chamber.12,14 In recurrent or chronic pupillary block the apposition of the peripheral iris to the cornea can result in peripheral anterior synechiae (PAS) and trabecular damage. In some cases, glaucoma occurs in the absence of lens dislocation, suggesting an open-angle mechanism (trabecular or angular abnormality).12 In the presence of elongated zonules, mid-dilation can precipitate acute angle-closure glaucoma even in the absence of ectopia lentis.15 Abnormal anterior chamber angles (abundant iris processes, iris root fraying) have been described but are not specific of this syndrome.16
Does the Patient Have Features Typical of Marfan Syndrome?
Patients with this autosomal dominant syndrome are tall, with slender fingers and toes (arachnodactyly), hyperflexible joints, and severe scoliosis resulting in pectus excavatum.5 Mutations on chromosome 15 can affect the synthesis of fibrillin, a connective tissue protein present in the zonules.17 Chromosome 5 mutations have also produced a similar syndrome.18 Cardiovascular abnormalities include aortic dilatation and dissecting aneurysm as well as mitral valve insufficiency.5
What is the Pathogenesis of the Glaucoma in Marfan Syndrome?
Marfan syndrome is associated with ectopia lentis in up to 80% of cases.4 The lens is usually displaced superiorly and frequently temporally. The lens zonules are reduced in number but structurally normal, which explains the low rate of progression of the dislocation, about 7.5%.19 As a result, glaucoma is not a common occurrence in Marfan syndrome, its incidence ranging from 5 to 8%.4,13,20 Pupillary block from lens dislocation has traditionally been thought of as the most common mechanism of glaucoma.5,13 Several abnormalities of the angle4,21 have been observed, such as a hypoplastic ciliary muscle, insertion of the longitudinal fibers onto the trabecular meshwork, and an apparent anterior iris insertion. In addition, Schlemm’s canal appears discontinuous, showing in some areas more than one channel.4 Interestingly, one report has suggested that open-angle mechanisms may be more common than previously thought.20 In addition, 15% of Marfan patients who undergo cataract extraction later develop open-angle glaucoma, a higher incidence than in nonoperated patients.4
Does the Patient Have Features Typical of Homocystinuria?
Some systemic features of homocystinuria are similar to those of Marfan syndrome. Patients are tall and slender, with fair skin and hair.4 Arachnodactyly is less marked than in Marfan syndrome. Mental retardation is present in 50% of cases,5 and the occurrence of multiple thromboembolic phenomena can be life threatening, especially after general anesthesia.
What Is the Pathogenesis of Glaucoma in Homocystinuria?
Bilateral, symmetrical ectopia lentis is slightly more common in homocystinuria than in Marfan syndrome (90% vs. 80%).4 Lens displacement occurs earlier in life and is usually inferior and lateral. In contrast to Marfan syndrome, the lens zonules in homocystinuria appear to be structurally abnormal.5 As the zonules disintegrate, the lens subluxation often progresses to total dislocation.13 The lens may migrate into the anterior chamber in up to 50% of cases, and posterior migration into the vitreous cavity is not uncommon.22 As a result, glaucoma is more common in homocystinuria than in Marfan syndrome4 (23% vs. 8%) and usually results from pupillary block. Angle abnormalities have not been reported1 (see Table 10–3). Glaucoma can result after cataract extraction, but not as frequently as in Marfan syndrome.
Treatment and Management
How Is Glaucoma Associated with Ectopia Lentis Managed?
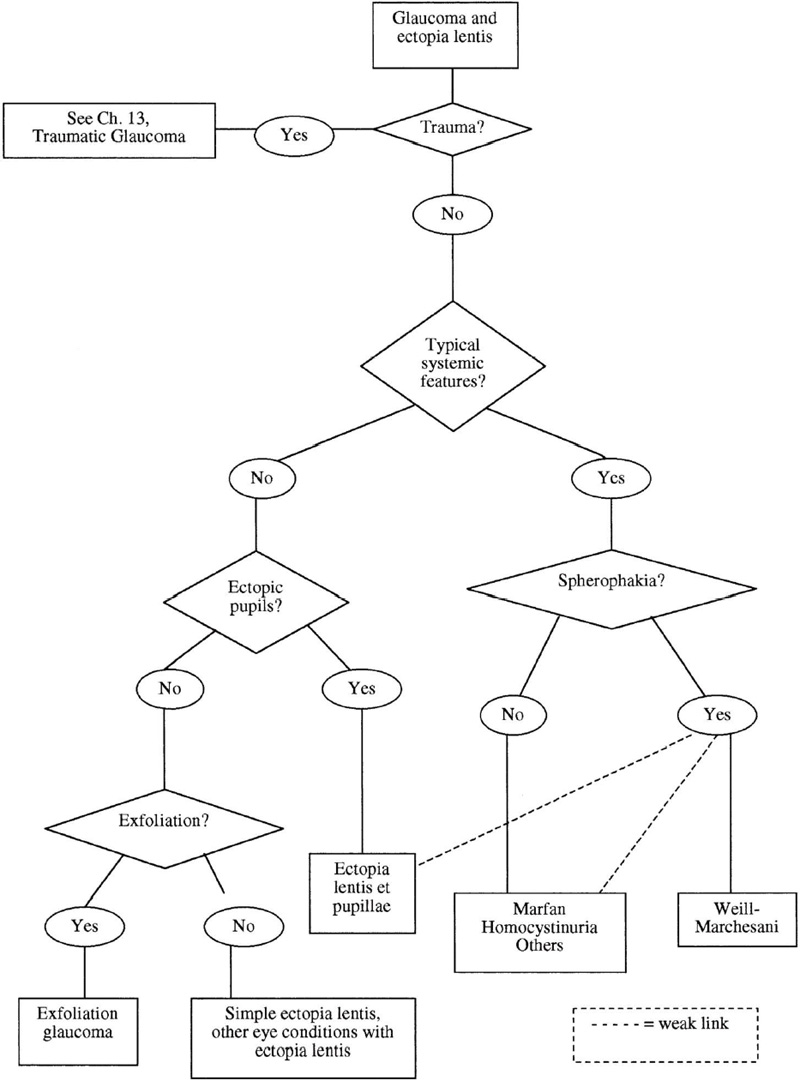
The treatment is dictated by the mechanism causing the disease, the most common being pupillary block. Open-angle mechanisms may coexist with pupillary block and are addressed separately. Figure 10–2 outlines the treatment choices based on the clinical picture.
Figure 10–2. Glaucoma and ectopia lentis: management.
Is There Pupillary-Block Angle-Closure Glaucoma?
In this situation the luxated or subluxated lens prevents the free flow of aqueous humor across the pupil into the anterior chamber. Aqueous accumulates behind the iris, pushing its peripheral portion against the trabecular meshwork.1,4 The speed and extent of the anterior migration of the lens will determine the clinical presentation and the treatment strategy.
The initial treatment of pupillary-block glaucoma in ectopia lentis includes placing the patient in a supine position, promoting vitreous dehydration with osmotic agents, and reducing IOP with beta-blockers, carbonic anhydrase inhibitors, and other drugs. These measures facilitate posterior migration of the lens away from the pupil1,4 but may have limited success.22 A peripheral iridotomy is usually performed to treat the pupillary block. The next treatment decision to be made depends on the location of the lens at the time of presentation.
Is the Lens Still in the Posterior Chamber?
In this case the lens should be moved away from the pupil. As a general rule, maximal pupillary dilatation will decrease the area of lens-iris contact, therefore diminishing the degree of pupillary block.1,4 Cycloplegics are useful to pull the iris-lens-ciliary body diaphragm back. These two actions, in addition to the initial measures, promote posterior displacement of the lens and may relieve the pupillary block. On the other hand, maximal pupillary dilatation may allow the passage of a completely dislocated lens through the pupil into the anterior chamber, an unwanted occurrence.4
Regardless of the success of the initial measures, the pupillary block can be overcome by creating a peripheral iridotomy (PI), usually with the neodymium: yttrium-aluminum-garnet (Nd:YAG) laser.1,4 If gonioscopy reveals no PAS, these patients can be placed on chronic miotic therapy to keep the lens behind the iris.4 A PI alone may not prevent subsequent anterior dislocation.22 If in addition the dislocated lens is creating a phacomorphic component (direct anterior pressure on the peripheral iris), lens extraction may be necessary. The PI will not be enough to resolve the angle closure in these cases. After the attack has been broken in the involved eye, prophylactic iridotomy should be performed in the fellow eye.4,22
If on the other hand post-PI gonioscopy reveals significant PAS or if trabecular damage is suspected, the management is dictated by the level of IOP and the degree of lens malposition. Visual disability from the dislocation is an additional factor to consider. If the dislocated lens can be kept in the posterior chamber, then medical treatment and filtering surgery can be sequentially used to control the IOP. Again, if the dislocated lens is adding a phacomorphic component and the IOP is uncontrolled, lens extraction becomes necessary.
In cases of microspherophakia (usually Well-Marchesani syndrome), an iridotomy can be placed prophylactically whether or not pupillary block has occurred.4 In general, miotics are not recommended because they relax the weak zonules, promoting anterior migration of the lens, and increasing the contact between iris and lens, therefore worsening the pupillary block1,15 (“inverse glaucoma”). Maximal pupillary dilation is the initial recommended strategy since mid-dilation of the pupil has been known to cause bilateral pupillary-block angle-closure glaucoma.15 Peripheral iridoplasty has also been tried successfully in the treatment of angle-closure glaucoma in Weill-Marchesani syndrome.23 For description and complications of peripheral iridoplasty, see Chapters 12 and 19.
Is the Lens in the Anterior Chamber?
In this case, if the lens is clear and pupillary block is not present, the initial management can be conservative. An attempt to reposition the lens can be made by maximally dilating the pupil and placing the patient in a supine position. Manual indentation of the central cornea has been successful as an adjunctive measure.24 If these measures are successful, a laser PI will prevent the recurrence of pupillary block, and chronic miotics will keep the lens in the posterior chamber. If these measures fail (the clear lens remains in the anterior chamber or adheres to the cornea) lens extraction is indicated to prevent further complications.
If pupillary block is present, the condition represents a true emergency because the IOP is usually very high. Delayed treatment will result in irreversible damage to the nerve, cataract formation, or corneal decompensation. The block occurs between the anterior iris and the posterior surface of the dislocated lens or as a direct pupillary occlusion by an entrapped lens. Initial measures should include hyperosmotics, aqueous suppressants, and placing the patient in a supine position. A laser PI can next be performed to relieve the pupillary block.1,4
If these measures are successful, the IOP will decrease and the anterior chamber will deepen as the angle opens. One then faces the following therapeutic alternatives. If the lens is cataractous, miotic therapy can keep the lens in the anterior chamber in preparation for lens extraction via a limbal approach. If the lens is clear, maximal pupillary dilatation after the resolution of the pupillary block may allow the lens to fall backward, and then it is managed with miotics as described above. If the lens remains in the anterior chamber despite medical therapy and PI, lens extraction is indicated.
Future Considerations
The key to successful management of this condition is early diagnosis. Prompt referral to an ophthalmologist will prevent life-threatening complications that can occur with some congenital syndromes. New techniques and instrumentation have made the surgical management of these conditions much safer. At this time, pars plana vitrectomy techniques with ultrasonic lens fragmentation offer a successful alternative both in adults25 and in children.26
GLAUCOMA ASSOCIATED WITH CATARACT FORMATION
Definition
How Is Glaucoma Associated with Cataract Formation Defined?
Cataract and glaucoma can be present in an eye in three different situations: (1) they can coexist independently, (2) both can be the result of the same pathologic process (e.g., trauma, inflammation), and (3) one can be the result of the other one. This section specifically addresses the third situation, where glaucoma is in some way the result of cataract formation or its complications.
Epidemiology and Importance
Both glaucoma and cataract independently increase in prevalence with age; therefore, they commonly coexist in the elderly. The Beaver Dam Eye Study evaluated these two issues in a large population study.27,28 The overall prevalence of primary open-angle glaucoma (POAG) was 2.1%, ranging from 0.9% in persons 43 to 54 years of age to 4.7% in persons 75 years of age and older.27 There was no significant effect of sex after adjusting for age. It is known that the prevalence of POAG is higher in black populations (see Chapter 2). The prevalence of age-related cataracts increased with age for both sexes, with women being more severely affected than men. Overall, 17.3% of patients had nuclear sclerosis and 6% had posterior subcapsular opacities.28 On the other hand, the occurrence of lens-related glaucoma is strongly linked to the duration of the cataract, with most types of glaucomas occurring in long-standing cataracts.29–31 Cataracts in the United States are removed relatively earlier than in the developing world. An average preoperative visual acuity of 20/60 was determined in one study.29 As a result, a lower incidence of lens-related glaucomas can be expected. More specific epidemiologic data is presented when each entity is discussed separately.
We are offered a unique opportunity to successfully treat the glaucoma by addressing the lens condition. With a better understanding of the mechanisms of disease, the terminology has become less confusing. Currently accepted definitions will be used to discuss this fascinating group of diseases.
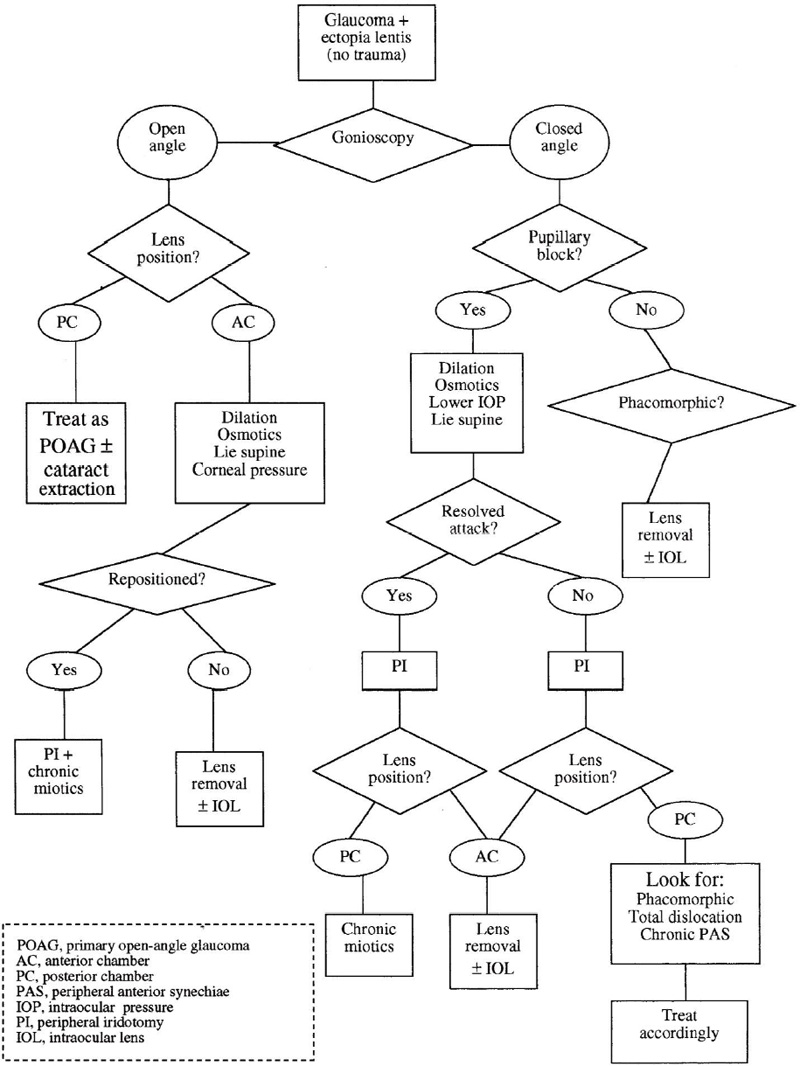
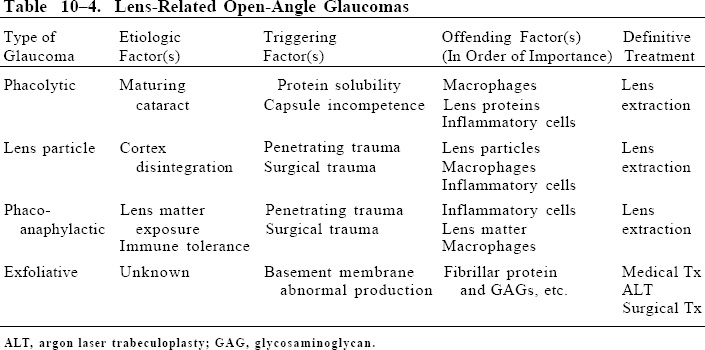
How Is Glaucoma Associated with Cataract Formation Classified?
Once again, the appearance of the angle and the mechanism of disease represent the major criteria to classify these entities. Table 10–4 outlines the etiologic and pathogenic factors involved in the production of the different cataract-related open-angle glaucomas. Table 10–5 describes the various mechanisms of glaucoma associated to cataract formation. Due to the association of phacoana-phylaxis with cataract surgery, this entity is discussed in a different section (see Glaucoma Associated with Aphakia and Pseudophakia, below).
Open-angle glaucoma (lens-induced glaucoma) |
Lens particle glaucoma |
Phacolytic (lens protein) glaucoma |
Phacoanaphylactic glaucoma |
Angle-closure glaucoma |
Pure pupillary block* |
Primary angle-closure glaucoma |
Lens enlargement + pupillary block |
Phacomorphic glaucoma (intumescent lens) |
Angle-closure glaucoma + large cataract (nonintumescent lens)** |
*A normal-sized lens in a small globe can generate pupillary block. This in essence represents a type of lensinduced glaucoma. |
Diagnosis and Differential Diagnosis
How Is Glaucoma Associated with Cataract Formation Diagnosed?
A good history and careful examination are always essential. As we determine the mechanisms of disease acting in a given patient we can then make the appropriate diagnosis and plan the treatment accordingly. Figure 10–3 outlines the diagnostic process and the differential diagnosis of these conditions. The management of these conditions will be discussed separately when each entity is discussed.
Is There a History of Trauma?
Glaucoma associated with ocular trauma is discussed in Chapter 13. Nevertheless two specific clinical entities caused by lens trauma are discussed in this chapter as they represent types of glaucoma essentially caused by lens-related mechanisms. These two are lens particle glaucoma and phacoanaphylactic glaucoma. The status of the lens capsule is the next question to be considered.
Has the Lens Capsule been Violated?
Capsular disruption can result from trauma, either surgical (extracapsular cataract extraction) or nonsurgical (penetrating). In both instances lens particles are released and continuously exposed to the inner ocular environment.31 Blunt trauma can in rare instances disrupt the lens capsule, and spontaneous ruptures have also been described. If the capsule has been disrupted, one should suspect the presence of lens material in the anterior segment of the eye. The next step is to determine if there is inflammation and assess the degree and nature of the reaction. If lens particles are seen floating in the anterior chamber, one should suspect lens particle glaucoma (see next section). If significant inflammation with granulomatous reaction is present, the possibility of phaco-anaphylaxis must be considered.
Figure 10–3. Glaucoma and cataract: differential diagnosis.
LENS PARTICLE GLAUCOMA
Definition
How Is Lens Particle Glaucoma Defined?
In this entity the release of lens particles is the result of trauma to the lens. This material circulates in the anterior chamber, blocking the trabeculum and causing a significant IOP elevation.31
Epidemiology and Importance
Extracapsular cataract surgery is the method of choice for surgeons in the United States29 and most countries around the world. Surgeons who operate on the anterior segment know that small amounts of cortex left in the eye cause no significant complications. This material is usually handled by the cellular and drainage mechanisms of the eye.30 As a result, postoperative IOP elevations and inflammation are usually moderate, transient, and responsive to medical treatment. As surgical techniques continue to improve, lens-related complications will decrease in frequency.
What Is the Pathogenesis of Lens Particle Glaucoma?
In some instances this material adopts a particulate pattern and causes a significant blockage of aqueous outflow.31 The resulting elevation in IOP is proportional to the amount of material released, stressing the mechanical nature of the obstruction and the resulting glaucoma. Macrophages, inflammatory cells, and debris can add to the blocking effect of the lens matter30 (see Tables 10–4 and 10–5).
Diagnosis and Differential Diagnosis
How Is Lens Particle Glaucoma Diagnosed?
The glaucoma can occur weeks, months, or even years after the trauma (or surgery).30 Patients usually present with ocular pain and decreased vision in one eye. White, fluffy lens material can be seen in the anterior chamber in addition to a moderate amount of cells and flare. In extreme cases, a hypopion may be present. The anterior chamber angle is usually open. Macrophages containing lens proteins (as in phacolytic glaucoma) have also been identified31 and may play a role in further blocking the trabeculum.30
In addition to the mechanical obstruction of the open angle by various components, untreated inflammation and its secondary changes (peripheral anterior or posterior synechiae, angle scarring, pupillary membranes, and pigment deposition) can play additional roles in the pathogenesis of the glaucoma.1,30,31 Cystoid macular edema can result in further visual loss.
What Is the Differential Diagnosis of Lens Particle Glaucoma?
The diagnosis of this condition begins with the documentation of either surgical or nonsurgical lens trauma. Typical fluffy material in the anterior chamber, some inflammation, and elevated IOP with an open angle are strong diagnostic components. The differential diagnosis with other conditions that may mimic lens particle glaucoma are discussed below and illustrated in Figure 10–3.
Phacoanaphylaxis is another entity that can follow traumatic capsular disruption and should be considered in the differential diagnosis. As inflammation is the overriding problem, the IOP tends to be low. In the few cases where the IOP is high, phacoanaphylactic glaucoma results. Granulomatous inflammation with large keratic precipitates strongly suggests phacoanaphylaxis rather than lens particle glaucoma.30
In phacolytic glaucoma the lens capsule is grossly intact and a mature or hypermature cataract is present. A history of trauma is not a typical feature of this syndrome. White, fluffy material is not seen because the capsule has not been ruptured. On the other hand, a phacolytic component may be present in lens particle glaucoma if macrophages engulf lens proteins and contribute to outflow blockage.30,31 In less typical cases (specially postsurgical), an aqueous sample should be examined to rule out infectious endophthalmitis. An intraocular tumor could seed cells into the anterior chamber, but a thorough preoperative examination should have diagnosed the problem.
Treatment and Management
How Is Lens Particle Glaucoma Treated?
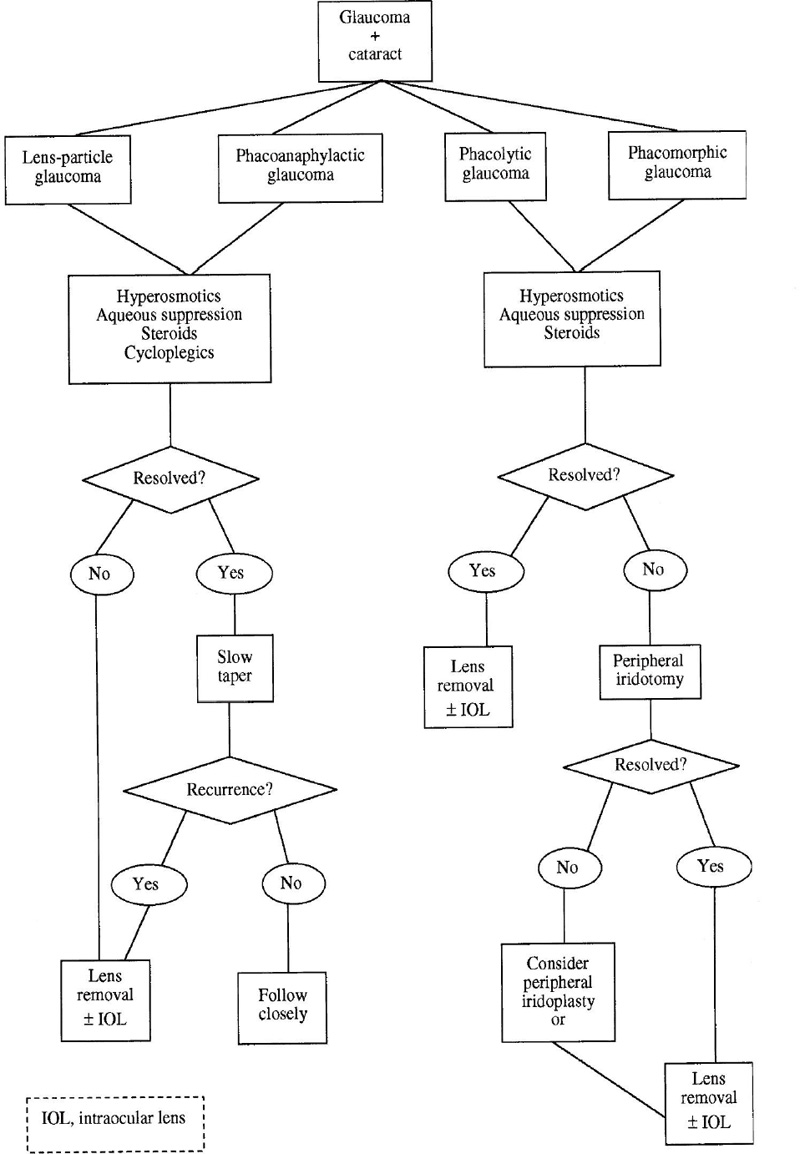
The initial therapy is medical and consists of aqueous suppressants, antiinflammatory drugs, and cycloplegics.30,31 If prompt improvement does not take place the definitive therapy consists of surgically removing all remaining lens fragments (Fig. 10–4). Delaying intervention can result in entrapment of lens material between capsular flaps or inflammatory membranes, making a late removal more problematic.30 Acting promptly when patients with a history of trauma or cataract surgery complain of sudden pain or decreased vision will prevent serious complications and permanent visual loss.
Can Nd:YAG Laser Posterior Capsulotomy Cause Lens Particle Glaucoma?
Some patients develop significant IOP elevation and inflammation following Nd:YAG laser posterior capsulotomy.32,33 Several features place this syndrome apart from classical lens particle glaucoma. First, the small amount of material released by the procedure does not explain an outflow obstruction on a purely mechanical basis. In addition there is no correlation between IOP level and amount of material floating in the anterior segment.30 It has been shown that the IOP elevation does result from decreased outflow, but the precise mechanism is not fully understood.33 Small, nonvisible lens particles or vitreous components blocking the trabeculum have been postulated as possible sources of obstruction.34,35 It may be better to reserve the term lens particle glaucoma for eyes with visible lens particles floating in the anterior chamber. This is not the case in the majority of patients with glaucoma after YAG capsulotomy. A small percentage of these patients will develop full-blown open-angle glaucoma and require conventional long-term medical therapy or filtering surgery.
Figure 10–4. Glaucoma and cataract: management.
Future Considerations
With current improvements in surgical techniques, lens particle glaucoma may continue to be seen more often in association with lens trauma than with cataract surgery. In both instances the removal of the lens material may require a more complex approach such as pars plana vitrectomy and lensectomy. It is hoped that future techniques will allow a safer IOL implantation in cases where the entire lens is removed.
Is There a Cataract, But a History of Trauma is Not Present?
When faced with a nontraumatic cataract and glaucoma, a crucial diagnostic element is the evaluation of the anterior chamber angle (see Fig. 10–3).
Is the Angle Open?
If the angle is open, one must carefully examine the lens to determine if one is dealing with a mature or hypermature cataract.
PHACOLYTIC GLAUCOMA
Definition
How Is Phacolytic Glaucoma Defined?
In this condition a particular type of lens proteins (see below) leak through the capsule and along with macrophages block the trabeculum, causing an IOP elevation. Usually a long-standing significant cataract is present.
What Is the Pathogenesis of Phacolytic Glaucoma?
If the cataract is mature or hypermature (rarely immature), the stage is set for phacolytic glaucoma. These cataracts have an increased amount of high molecular weight (HMW) soluble lens proteins.31 These proteins can leak through microscopic defects in the capsule and circulate in the anterior chamber. Current evidence indicates that the trabecular meshwork is blocked by both HMW proteins and macrophages containing engulfed proteins.35–37 It has been suggested that these proteins may be more specific and more closely responsible for the outflow blockage seen in phacolytic glaucoma.31 Crystals of calcium oxalate and cholesterol have also been identified in the anterior chamber38 (see Tables 10–4 and 10–5).
Epidemiology and Importance
Phacolytic glaucoma is uncommon in the United States, as cataracts are usually removed before they mature.29 Large series of patients with this entity come from countries where easy access to surgical eye care is not as readily available.38,39 In one such series, 45 consecutive patients were operated on during a 5-year period with excellent visual results and IOP control.38 There was no gender preference, and ages ranged from 45 to 85 years. Another series, reporting 44 phacolytic glaucomas and 49 phacomorphic (see next section) glaucomas diagnosed during 1 year, confirms the frequency of lens-induced glaucoma in other parts of the world.39
Diagnosis and Differential Diagnosis
How Is Phacolytic Glaucoma Diagnosed?
Because a cataract must be present, this disease usually presents in elderly adults. The sudden onset of open-angle glaucoma in an eye with a mature or hypermature cataract should be considered as phacolytic glaucoma until proven otherwise. These patients present with ocular pain and a prior history of decreased vision due to the cataract. A recent worsening in vision may have occurred.30 The eye appears injected and the IOP may be markedly elevated, causing corneal edema. The anterior chamber is formed, showing significant flare (soluble proteins) and variable amount of cells. These cells consist of small white cells and larger floating macrophages containing lens proteins.31 The filtration angle is open and appears grossly normal. The lens is opaque, and in some hypermature cataracts a brunescent nucleus rests inferiorly in a bag of liquefied cortex (morgagnian cataract). The anterior capsule may appear irregular or wrinkled, sometimes with whitish patches on its surface.31 In some cases the lens may luxate posteriorly, eventually falling into the vitreous cavity.
What Is the Differential Diagnosis of Phacolytic Glaucoma?
Refer to the section on differential diagnosis of lens particle glaucoma, above, for a comparison of phacolytic glaucoma with the most pertinent acute lens-induced glaucoma entities. If the history and examination are consistent and other types of open-angle glaucoma can be ruled out (e.g., neovascular, traumatic, inflammatory), the diagnosis can be reliably made on clinical grounds. If there is doubt, the microscopic examination of an aqueous sample looking for engorged macrophages is indicated. Using the Millipore® filter technique facilitates the identification of the macrophages.31 False negatives can occur, especially in eyes treated with steroids. Uveitis in the presence of a cataract (but not caused by it) is a major diagnostic category to be ruled out because the extraction of the cataract will cure phacolytic glaucoma but dangerously excacerbate the uveitis. Once again, in these cases the examination of the aqueous humor becomes critical.
As we continue to analyze the differential diagnosis in Figure 10–3 we reach another important question:
Treatment and Management
How Is Phacolytic Glaucoma Managed?
The initial treatment consists of hyperosmotic agents, aqueous suppressants, antiinflammatory drugs, and cycloplegics to temporarily control the disease (see Fig. 10–4). The definitive treatment currently consists of extracapsular extraction of the lens with or without intraocular lens implantation and should be carried out as soon as it is reasonably safe. Unless PAS or trabecular damage is present, the removal of the lens uniformly eliminates the glaucoma and provides excellent visual rehabilitation.39,40 Although not always feasible, the eye should be open after the IOP has been maximally lowered. If the IOP remains high, a paracentesis should be performed to partially decompress the globe before proceeding.1 If there is significant zonular dehiscence or difficulty opening the anterior capsule, an intracapsular lens removal30 with anterior chamber or sutured posterior chamber intraocular lens implantation can be considered. Some surgeons may choose to delay the implantation of the lens until the inflammation has subsided. In one large series the IOL implantation was not a factor affecting the final visual acuity (p = .18).41 Univariate analysis performed in this study showed that patients over 60 years of age with more than 5 days of disease had a higher risk of poor visual outcome. Visual acuity of light perception without projection has not been a poor prognostic indicator in many cases.39
Future Considerations
The management of phacolytic glaucoma consists of removing the lens, and the tendency is toward extracapsular surgery with primary IOL insertion.39,40 The use of viscoelastic materials has allowed a more controlled treatment of the capsule, and small-incision surgery may further improve the visual prognosis in these eyes. Cataract surgery in phacolytic glaucoma will continue to be a challenge.39
Is the Angle Closed?
If this is the case, the iris is being pushed against the cornea by either trapped aqueous humor or an enlarged lens. One or both of these components mechanically occlude the angle.
Is the Lens Intumescent?
This can be determined by careful anterior segment biomicroscopy complemented by ultrasonic studies. The axial diameter of the lens is significantly increased. Usually the lens appears white and the cataract is mature. The formation of an intumescent lens can occur over a variable period of time, often becoming noticeable by the pain induced by the elevated IOP. An intumescent lens in the presence of a closed angle is currently known as phacomorphic glaucoma (see Fig. 10–3).
PHACOMORPHIC GLAUCOMA
Definition
How Is Phacomorphic Glaucoma Defined?
This definition implies that the lens is mechanically exerting a direct “pushing” effect on the iris, causing the closure of the angle. This can result from an anteriorly dislocated lens or, most commonly, from an enlarged lens.1,2
Epidemiology and Importance
Because phacomorphic glaucoma due to an intumescent lens occurs in cases of advanced, long-standing cataracts, the concepts mentioned in the previous section on phacolytic glaucoma apply to phacomorphic glaucoma as well. Again, this is an uncommon entity in the United States, and large series come from overseas.41
What Is the Pathogenesis of Phacomorphic Glaucoma?
In an eye with a nontraumatic cataract and a closed anterior chamber angle, the possibility of phacomorphic glaucoma should be entertained. The term phacomorphic has been traditionally associated with an intumescent lens.1,2,31,35 Intumescence results from influx of water and swelling of the lens cortex, rarely the nucleus. This usually occurs in mature senile, diabetic, uveitic, and traumatic cataracts. The result is distention of the capsule and an increase of the axial diameter of the lens41 (see Table 10–5).
An enlarged lens can cause angle-closure glaucoma via two mechanisms. First, an increased iris-lens contact results in a relative pupillary block, and second, the enlarged lens can directly push the iris (phacomorphic effect) forward against the cornea, occluding the angle. Usually, whenever phacomorphic glaucoma is present, there is some degree of pupillary block.42,43 Eyes with narrow angles are more likely to suffer from this type of angle closure.4,43
Is the Lens Nonintumescent, But Still Large?
An increase in the axial diameter of the lens can also occur without intumescense, most commonly as a result of a growing cataract. In eyes with narrow angles (hyperopia, small globes with shallow anterior chambers), a phacomorphic component will result from simple lens enlargement, making acute pupillary-block glaucoma more likely.42 This is probably one of the mechanisms behind primary angle-closure glaucoma. In addition, a clear lens could become “too large” for the eye, acting mechanically to activate the mechanisms previously described. We see how the size of the lens and its spatial relationships with surrounding structures can create circumstances in which a pupillary-block component coexists with a phacomorphic component.42
Diagnosis and Management
How Is Phacomorphic Glaucoma Diagnosed?
The diagnosis is usually based on the clinical examination. We should suspect phacomorphic glaucoma in any eye with angle-closure glaucoma and an advanced cataract. Usually the vision is poor, the patient is in pain, and the eye is injected. The cornea can be edematous due to the increased IOP.4 The angle appears closed and cannot be opened upon reasonable corneal indentation. Low-grade inflammation can sometimes be observed in a uniformly shallow anterior chamber. If the examination of the fellow eye reveals a deeper central anterior chamber, it is likely that lens swelling is present in the involved eye.4
On clinical examination what differentiates phacomorphic glaucoma from pure pupillary-block glaucoma is the equal shallowness of the axial and peripheral anterior chamber. In pupillary block the iris bombé gives the axial chamber a greater depth than in phacomorphic glaucoma. An intumescent lens is commonly seen, but a totally dislocated lens in the posterior chamber can be present. Ultrasound biomicroscopy can neatly delineate the various surfaces involved in the pathogenesis of this and other types of angle-closure glaucoma.44
What Is the Differential Diagnosis of Phacomorphic Glaucoma?
Figure 10–3 illustrates the thinking pathway as we deal with patients with cataract and angle-closure glaucoma. Other causes of angle closure should be first ruled out. Usually a good history and a detailed anterior segment examination will identify traumatic glaucoma, neovascular glaucoma, exfoliation glaucoma, phacolytic glaucoma, and the various types of angle-closure glaucoma. In addition, the differential diagnosis includes miotic therapy, aqueous misdirection, and uveal effusion, all of which can exert the same effect on the iris and angle.42 As the view of the posterior pole is impeded by the cataract, a B-scan should be done to rule out a retrolenticular tumor causing the anterior displacement of the lens.45 Ultrasonography will also identify choroidal effusions and iris cysts, which can result in angle-closure glaucoma.44
Treatment and Management
How Is Phacomorphic Glaucoma Managed?
As in other entities discussed in this chapter, it is desirable to reduce inflammation and IOP medically before definitive surgical treatment is undertaken. The initial treatment, therefore, consists of hyperosmotics, aqueous supressants, and antiinflammatory agents. Cycloplegics may not be able to deepen the anterior chamber and may further crowd the angle. Miotics can worsen the pupillary block or create one by pulling the iris-lens diaphragm forward. The definitive therapy consists of removal of the lens with or without IOL placement.4,31,42 If the IOP can be medically controlled and a large intumescent lens is present, lens removal can be the first and definitive surgical approach.
It appears that in most cases there is a significant component of pupillary block; therefore, a YAG laser PI is indicated as an effective way of lowering the IOP to safe levels.4,42,46 If the pupillary block is broken and the IOP controlled, lens extraction can be performed under safer circumstances. A reasonable approach, therefore, would consist of medical treatment initially with a PI to follow in preparation for cataract removal. If a PI does not open the angle, then removal of the lens should be performed. Laser peripheral iridoplasty has also been suggested as an option for some phacomorphic glaucomas,4,47 but is not widely used in this setting.
In the presence of a visually significant cataract, the goals are to visually rehabilitate the eye and prevent permanent optic nerve and trabecular damage as well as peripheral anterior synechiae. Lens extraction under the best possible circumstances will achieve all these goals. The removal of an intumescent lens poses particular challenges as the milky cortex will leak out as soon as the anterior lens capsule is perforated. Initial decompression of the lens and generous use of viscoelastic material usually permits a more controlled anterior capsulotomy. Successful continuous-tear capsulorhexis has been performed using this technique, allowing in-the-bag IOL placement.48
Future Considerations
New techniques and viscoelastic use allow safe management of these eyes. When safe extracapsular surgery cannot be performed, pars plana lensectomy with anterior chamber or sutured IOL placement will continue to be an appropriate alternative.
GLAUCOMA ASSOCIATED WITH EXFOLIATION SYNDROME
Definition
How Is Exfoliation Syndrome Defined?
Exfoliation syndrome (ES) is a systemic basement membrane disorder that results in the production and deposition of abnormal material throughout the eye and other system organs. In conjunction with the lens abnormalities, a particular type of secondary open-angle glaucoma results in some patients.49,50
Epidemiology and Importance
The reported incidence and prevalence of this disease has significantly increased in recent years across the racial spectrum.51–56 An increased awareness of the disease and more thorough examinations under full pupillary dilatation partially explains this trend.57 Despite these data, the prevalence of ES in the general population remains linked to racial and ethnic factors, varying from almost zero among Eskimos to about 25% in Scandinavia and 38% in Navaho Indians.49,58 The prevalence of ES markedly increases with age in all races and ethnic groups.54,55,59 In the United States the Framingham Eye Study found ES in 0.6% of persons between 52 and 64 years of age and in 5% of persons between 75 and 85 years of age.60 African Americans have a lower prevalence of ES than European Americans of Scandinavian descent.61 Some reports indicate that ES may be more common in females,62 but others have shown no difference between the two sexes.61 No hereditary pattern has been determined in ES.63 Exfoliation syndrome has been described in a 17-year-old girl with congenital glaucoma who had undergone trabeculectomy and PI in infancy.64 This report linked iris surgery to the occurrence of ES.
What Is the Prevalence of ES in Patients with Glaucoma?
The reported average prevalence of ES in U.S. glaucoma populations is approximately 12%.65,66 Overseas this prevalence has varied from 1.4%67 to 75%68 and higher, reflecting the geographic and ethnic variability of this disease. A study from Spain found ES in 243 (44.5%) of 546 eyes with open-angle glaucoma.69
What Is the Prevalence of Glaucoma in Patients with ES?
The presence of ES markedly increases the incidence and prevalence of elevated IOP and glaucoma in a given age population.69–71 The frequency of glaucoma in ES populations varies from 7%62 to 48.9%.72 It has been suggested that ES may be a glaucoma risk factor on its own, independent of the IOP elevation documented in these patients.73 In longitudinal studies eyes with ES and normal IOP have a 5.3% probability of developing glaucoma in 5 years and 15.4% in 10 years. Thus, ES patients have a ten-fold increased risk of having or developing glaucoma compared with the general population.49 Higher figures have been reported.74
Diagnosis and Differential Diagnosis
How Is ES Diagnosed?
To a careful examiner the diagnosis of ES with a fully dilated pupil in an elderly patient should pose no difficulty.75 Early subtle signs can be detected in the absence of elevated IOP or full-blown features.76 The disease is in essence bilateral.77 Bilateral involvement has been more commonly reported in Europe78,79 than in the United States.62,80
The most striking feature is the presence of a dandruff-like white-gray material found more often on the anterior lens surface but actually distributed throughout the anterior segment. A granular sheet of this material can result from accumulation on the lens capsule.49,50,81 The continuous rubbing by the posterior iris wipes off the midperipheral portion of this material, leaving a central circle and the periphery intact.49 Rolled-up edges can often be seen at the margins. Exfoliation material commonly sits on the pupillary margin, giving the examiner a first diagnostic clue even before dilatation.82 ES material may also be seen on the iris, corneal endothelium, anterior chamber angle, lens zonules, and ciliary body. In addition it can be seen on the anterior vitreous face in aphakes83 and on intraocular lenses in pseudophakes.84 Involvement of the lens zonules results in their fragility and disruption.81,85 Partial or total lens dislocation can occur in advanced cases.49 Zonular weakness is a predisposing factor for intraoperative complications such as capsular rupture and vitreous loss during cataract surgery.86 A shallow anterior chamber due to weakened zonules may be present preoperatively.
As a result of the continuous rubbing of the posterior iris epithelium by the granular material, pigment is released into the anterior chamber. This pigment can be seen on the endothelium, anterior iris surface, and filtration angle. At the angle that is usually open, the pigment adopts a patchy configuration in contrast to the solid pattern seen in pigmentary dispersion syndrome.49,75,76 Pigment deposition can also be seen at Schwalbe’s line and in a wavy distribution in front of it (Sampaolesi’s line).50 As pigment is released from the central iris, transillumination defects develop in the area of the iris sphincter,3,49 but generalized transillumination of the iris has also been described.87 Ischemia of the iris has been shown by angiographic88 and fluorophotometric studies.
What Is the Nature of the Exfoliation Material?
Exfoliation material is an irregular meshwork of randomly oriented crossbanded fibrils within a loose fibrogranular matrix.49,89 It probably consists of macromolecules with protein and polysaccharide components.90 The precise biochemical nature of the material is not known, but there is evidence of the presence of glycosaminoglycans, fibronectin, chondroitin sulfate proteoglycans, amyloid P protein, and type IV collagen.49 Current data suggests that the exfoliation material is the result of an abnormal production of basement membrane, taking place in various eye structures and elsewhere in the body. Evidence of the production of this material has been found in the iris, lens, vascular endothelium, perivascular tissues, and zonular apparatus, among others. Extrabulbar and systemic production has also been documented.49,50,81
What Is the Pathogenesis of Glaucoma in ES?
Glaucoma occurs primarily through a secondary open-angle mechanism consisting of trabecular blockage by the exfoliation material and pigment.49,81,91 In addition, damage to the trabeculum49 and the juxtacanalicular tissue adjacent to the inner and outer walls of Schlemm’s canal92 can result from the deposition of the material. Exfoliation glaucoma can coexist with POAG in many patients. In contrast to most cases of POAG, exfoliation glaucoma can present as an acute open-angle glaucoma with corneal edema and very high IOP, in up to 25% of the cases.93 These eyes are congested, and if the anterior chamber is shallow they grossly resemble acute angle-closure glaucoma.91
Acute angle-closure glaucoma (ACG) in ES is less frequent than open-angle glaucoma.49 However, reports have documented an increased prevalence of occludable angles and ACG in patients with ES.94 Secondary angle closure in association with the use of miotics in ES has been reported.95 In eyes with narrow angles and ES, the acute glaucoma can be precipitated by weak zonules, allowing an anterior displacement of the lens. A similar mechanism produces the glaucoma associated with microspherophakia. The iris in ES is rigid, and an increased adherence to the pupil caused by the exfoliation material could further promote secondary pupillary block.96 Finally, ciliary block ACG (malignant glaucoma) has been reported in two patients with ES, presumably as a result of anterior lens displacement.97
Acute IOP elevations can occur in patients with ES when vigorous pupillary dilatation is induced. Sudden trabecular blockage by a large amount of released pigment is the explanation for this phenomenon.98 Marked elastosis of the lamina cribrosa in patients with exfoliation glaucoma has been found,99 suggesting that an intrinsic abnormality may render these optic nerves more susceptible to glaucomatous damage.
What Is the Differential Diagnosis of ES?
ES must be distinguished from pigmentary dispersion syndrome (PDS). This can usually be done without difficulty after a detailed examination. PDS occurs most commonly in myope young males. A Krukenberg spindle is usually present. Transillumination defects are midperipheral and radial in distribution, not central and patchy as in ES. Trabecular pigment deposition is usually dense and even. In general, the presence of exfoliation material is the hallmark of ES and makes the differential diagnosis easier. Other causes of lens subluxation can be considered and ruled out as mentioned in the pertinent section of this chapter.
What Are the Systemic Implications of ES?
The systemic nature of ES has been demonstrated by the presence of exfoliation material in the conjunctiva, extraocular muscles, retinal, ciliary and vortex vessels, and later in skin, lungs, liver, kidney, heart, and meninges.100–102 Despite extensive work in this area, no specific clinical entity has been reported to occur in the extraocular system as a result of ES.49,81
Treatment and Management
How Is Exfoliation Glaucoma Treated?
The lens is not the only source of exfoliation material; therefore, it is not surprising that the removal of the lens does not cure the glaucoma.1,4 Exfoliation glaucoma is otherwise treated in a manner similar to POAG. Therefore, the initial approach is medical, stepping up and adding antiglaucoma medications as needed to achieve a “target” IOP. The response of exfoliation glaucoma to medical therapy is less consistent and sustained than in POAG.103–107 There may be an insufficient “depot” function of topical drugs in the eyes of patients with exfoliation glaucoma. In one study, continuous delivery of pilocarpine achieved better IOP control than a four times a day schedule in patients with exfoliation glaucoma, suggesting that less drug is available between doses, resulting in a decreased hypotensive effect.104 Miotics may have the additional theoretical advantage of reducing the mechanical rubbing of the posterior iris surface, limiting the amount of pigment and exfoliation material released.49
When medical therapy fails, argon laser trabeculoplasty (ALT) has been effective in reducing IOP in these patients. The initial response has been in some cases greater than in POAG,105,108 but the long-term outcome has been similar for both groups.109 Others have reported a poorer response to ALT in exfoliation glaucoma.93 There may be an increased risk of IOP spikes due to pigment release.110 If pupillary block is present, an Nd:YAG laser PI would release less pigment than the argon laser.
The next step in the treatment of uncontrolled exfoliation glaucoma is incisional (filtering) glaucoma surgery. At this time partial-thickness techniques with suture modification are the preferred method of treatment. The surgical indications and techniques are basically the same as in POAG. The surgical outcome appears to be similar or better than in POAG.105 Postoperative complications may be enhanced by the disruption of the blood–aqueous barrier present in ES.111 The good results obtained with trabeculectomy suggest that surgery could be performed earlier than in POAG, as the failure rate of medical treatment and risks for optic nerve damage are higher.91 Trabeculotomy has been proposed as an alternative technique in selected cases,112 and in one series performed better than in POAG.113
What Is the Prognosis of Exfoliation Glaucoma vs. POAG?
In general, the course of exfoliation glaucoma is more severe than POAG as IOPs are higher at the time of diagnosis and throughout the disease. Furthermore, the progression of the optic nerve damage and visual field loss is more rapid than in POAG. More of these patients show poor response to medical therapy and a less sustained response to ALT. These results suggest that patients with exfoliation glaucoma may need earlier surgery than patients with POAG.114
Future Considerations
There has been more published work on ES than on all the other lens-related glaucomas combined, which reflects our current lack of knowledge about the precise etiology of this condition. A new technique called trabecular aspiration has been used to literally vacuum the trabeculum, removing pigment and exfoliation material.115 This technique has been used with and without cataract removal and has shown promising results 18 months after surgery.116 Ongoing clinical research is trying to determine if large-vessel abnormalities (aortic aneurysms) can be related to the presence of exfoliation material in some cases.81
GLAUCOMA ASSOCIATED WITH APHAKIA OR PSEUDOPHAKIA
Definition
How Is Glaucoma Associated with Aphakia or Pseudophakia Defined?
Glaucoma can occur in aphakic and pseudophakic eyes through specific pathogenic mechanisms. The denomination of these entities should include the specific mechanism involved, as aphakia or pseudophakia per se do not cause glaucoma. The terms aphakic glaucoma and pseudophakic glaucoma therefore should not be used alone.117 This section discusses eyes in which the absence of the natural lens or presence of an IOL is directly related to the occurrence of the glaucoma.
Epidemiology and Importance
The incidences of glaucoma in aphakia and pseudophakia have decreased and increased, respectively, since IOL insertion has become the norm during cataract surgery.29 Improvements in instrumentation and surgical techniques have had a great impact on the nature and frequency of IOP-related complications in these patients. These days, chronic glaucoma is not expected to result from uncomplicated cataract surgery, whether or not an IOL is implanted.118 In the past glaucoma was a common cause (30–40%) of enucleation of eyes after complicated intracapsular and extracapsular cataract surgery.119 With the improvement in IOL design and instrumentation, chronic glaucoma has become a less frequent event, ranging from 2.1%120 to 4%121 of cases. As phacoemulsification with in-the-bag IOL implantation becomes the standard technique, it is expected that the incidence of chronic glaucoma associated with extracapsular techniques will continue to decrease.122
What Is the Pathogenesis of Glaucoma in Aphakia and Pseudophakia?
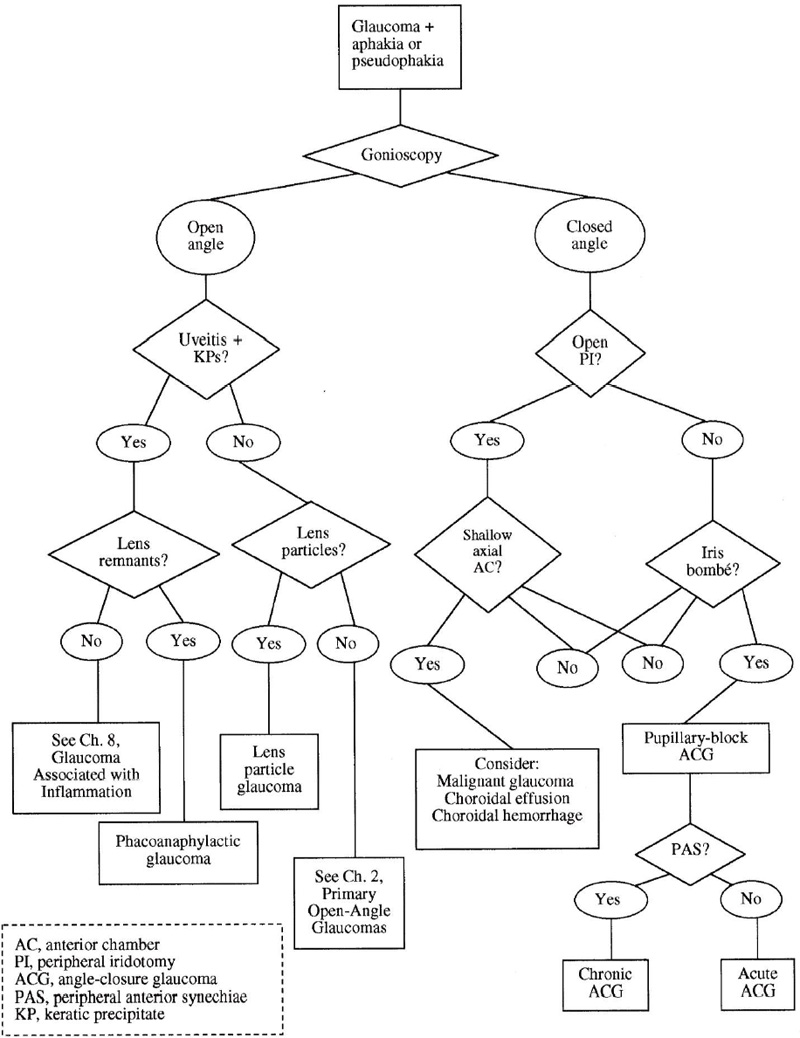
Glaucoma in aphakia and pseudophakia is best understood in terms of time of presentation, clinical features, and pathogenic mechanisms (Fig. 10–5).
Open-angle glaucoma can occur at different times after surgery. Early IOP elevations can result from inflammation or the presence of debris, cortical material, hemorrhage, or residual viscoelastic material in the anterior chamber.118–123 In some cases the IOP rises immediately after uneventful surgery without identifiable cause.124 Trabecular edema, distortion of outflow channels by sutures, and inflammation have been proposed as possible contributory factors.125 On the other hand, IOP elevations can take place a few weeks after surgery. Possible causes include vitreous in the anterior chamber, persistent hyphema or inflammation, lens particle mechanism, proteins and macrophages in phacoanaphylaxis, and steroid effect. In eyes without an intact posterior capsule and vitreous hemorrhage, ghost cells can block the trabeculum and cause persistent glaucoma.118,123 Late causes of open-angle glaucoma after cataract surgery include ghost cell glaucoma, chronic inflammation, late-occurring hemorrhage, Nd:YAG laser capsulotomy,126 and vitreous in the anterior chamber. Preexistent POAG can cause IOP elevation any time after surgery and should always be suspected when no other cause of the glaucoma is apparent.125
Figure 10–5. Glaucoma in aphakia or pseudophakia: differential diagnosis.
Angle-closure glaucoma can result from a number of mechanisms. In the past, flat or shallow anterior chambers and inflammation after intracapsular cataract extraction often resulted in extensive PAS and secondary angle closure. With improved closure techniques and sutures, this complication has become infrequent. Instead, pupillary block is the most common mechanism responsible for ACG in aphakia and pseudophakia.118,123,127
Pupillary block in aphakia usually results from vitreous apposition to the pupil when the anterior chamber is shallow and a peripheral iridectomy is absent.117 In these eyes aqueous misdirection (malignant glaucoma) can be difficult to distinguish from pupillary block. Pupillary block in pseudophakia can be caused by anterior chamber or iris-supported IOLs if a PI was not performed.128,129 This complication has been reduced, but not eliminated, with current extracapsular techniques and posterior chamber IOL implantation.130,131 When pupillary block does occur, it can be caused by posterior synechiae to the IOL from inflammation or blood. Capsular components and cortical material can contribute to this process, adhering to the iris or IOL and even blocking an existent PI.125 In addition, loose vitreous can migrate anteriorly and block the pupil after complicated cataract surgery or after posterior capsulotomy.132
In the absence of pupillary block, PAS and ACG may result from prolonged inflammation, hemorrhage, shallow anterior chamber, or faulty wound closure with iris incarceration in the wound.117,125 The haptics of anterior chamber IOLs are known to promote PAS formation, although this complication has become less frequent with current lens designs.125 Fibrous, epithelial or endothelial tissue obliterating the anterior chamber angle can result in postoperative secondary glaucomas (discussed elsewhere in this book).
Diagnosis and Differential Diagnosis
How Is Glaucoma in Aphakia or Pseudophakia Diagnosed?
The diagnostic approach and differential diagnosis outlined in Figure 10–5 refer to subacute or chronic glaucoma. Early, transient postoperative elevations of IOP are discussed previously in this section. Once elevated IOP is confirmed in an aphakic or pseudophakic eye without preexistent glaucoma, the first crucial step is in determining the configuration of the anterior chamber and the angle.
Is the Angle Open?
If this is the case, we should first rule out the possibility of intraocular inflammation as the cause of the glaucoma.
Is Inflammation Present?
If anterior segment inflammation is present, one must determine if residual lens matter is playing a role in the inflammation. In cases of full-blown uveitis and keratic precipitates, a thorough examination after maximal pupillary dilatation may reveal the presence of cortical material. The possibility of phacoanaphylaxis should then be entertained. In the absence of this material, other causes of uveitis should be explored (see Chapter 8).
Treatment and Management
The management of glaucoma associated with aphakia or pseudophakia varies according to the mechanism of disease and the entity in question. Phacoanaphylaxis will be discussed separately, as it involves distinct clinical features and pathogenic mechanisms.
PHACOANAPHYLAXIS
Definition
How Is Phacoanaphylaxis Defined?
Phacoanaphylaxis is an uncommon immunologic and inflammatory condition triggered by the exposure of the internal eye to lens matter. It is essentially a granulomatous uveitis rarely associated with glaucoma.133 It is discussed in this section because it can occur following cataract surgery.
What Is the Pathogenesis of Glaucoma in Phacoanaphylaxis?
The basic inciting event in phacoanaphylaxis is usually the traumatic disruption (surgical or nonsurgical) of the lens capsule (see Fig. 10–3). The subluxation of an intact lens into the vitreous cavity has been considered another triggering mechanism.134 It is now thought that somehow the immune tolerance to lens proteins is lost and a granulomatous reaction is initiated by the immune system of the eye, resulting in phacoanaphylaxis.135
Open-angle glaucoma can result from trabecular inflammation as well as debris and cells blocking the trabeculum.28,133 Two basic angle-closure mechanisms take place: peripheral anterior synechiae can permanently occlude the filtration angle, and posterior synechiae can cause secondary pupillary block. In addition, a steroid-induced IOP elevation can take place over the inflammatory glaucoma.1
Diagnosis and Differential Diagnosis
How Is Phacoanaphylaxis Diagnosed?
The disease can present hours to months after the lens injury or surgery.28 The vision is usually reduced and the eye is injected. The severity of the uveitis is variable, but usually keratic precipitates are present and rarely lens material can be seen in the anterior chamber.1,28 Vitreous inflammation may result from an extension of the anterior uveitis. The offending lens residues can usually be seen. Depending on the duration and severity of the disease, posterior or peripheral anterior synechiae may be already present.133 In severe, protracted cases, neovascularization of the iris or even phthisis bulbi can occur. If doubt exists as to the nature of the inflammation, an infectious etiology should be promptly ruled out by obtaining aqueous and vitreous samples for examination.
What Is the Differential Diagnosis of Phacoanaphylactic Glaucoma?
The diagnosis of this condition can be difficult, and often is definitively made by histopathologic examination. An aqueous sample may show macrophages similar to those in phacolytic glaucoma.136 Because trauma to the lens usually precedes both lens-particle and phacoanaphylactic glaucoma, these two conditions can be confused. Fortunately, the removal of all lens material cures both diseases. Inflammation tends to be more significant in phacoanaphylaxis, and large keratic precipitates (KPs) are not usually seen in lens particle glaucoma. A reaction that follows immediately after the injury is most likely to be lens-particle mediated because in most cases a certain time is required for the eye to sensitize to lens components.28 In bacterial endophthalmitis (posttraumatic or postsurgical) usually a hypopion will be present. Low-grade infectious endophthalmitis caused by Propionibacterium acnes or fungi should be considered in delayed cases. Other possible causes include reactions to components used during surgery and phacolytic glaucoma. The presence of inflammation in the fellow eye should raise the suspicion of sympathetic ophthalmia, although certainly more than one mechanism may be acting in the same patient.133
Treatment and Management
How Is Phacoanaphylactic Glaucoma Managed?
The initial treatment consists of topical antiinflammatory therapy along with antiglaucoma medications. Almost uniformly the uveitis recurs despite continuing therapy.28,133 The definitive treatment is the removal of all lens residues from inside the eye. This is currently done via a pars plana approach to gain access to lens material located posteriorly. Often the capsule and therefore the IOL may have to be removed.28 An anterior chamber or sulcus-placed IOL may have to be removed. Intensive postoperative steroid therapy must be monitored for the possibility of steroid-induced glaucoma. Histopathologic examination of the surgical specimen must then be performed to confirm the clinical diagnosis. If the glaucoma persists after the removal of the lens material, other open-angle or angle-closure components should be appropriately addressed. Glaucoma filtering surgery with antimetabolites may be needed in most of these patients.
After completing our discussion of phacoanaphylaxis we continue to analyze Figure 10–5. We now continue the discussion of glaucoma and aphakia/ pseudophakia, and again turn to the question of inflammation.
Is Inflammation Absent from the Eye?
In this case we can diagnose these patients as having POAG in the presence of aphakia or pseudophakia. This category includes cases of preexistent POAG, new-onset POAG, and trabecular damage from previous inflammation, pigment deposition, or other unknown factors. For management purposes, this last group can be grouped to POAG, with some special considerations on a case-by-case basis.
Is the Angle Closed?
If this is the case, the next critical issue is whether or not a functioning PI (or iridectomy) is present. Pupillary block is the most common cause of ACG.
In the absence of an open PI, pupillary block is the most likely acting mechanism. Further certainty exists if a characteristic iris bombé configuration is present (anterior chamber is deeper axially than peripherally). The chronicity of the condition will be reflected by the presence of posterior or peripheral anterior synechiae. Depending on the case, posterior synechiae can form between the iris and the vitreous face, anterior chamber IOL, posterior chamber IOL, or intact posterior capsule. In aphakic eyes the iris bombé configuration is less evident. If this configuration is not present, one should consider the possibility of aqueous misdirection or malignant glaucoma.127
If a functioning PI is present, pupillary block is most likely not the mechanism responsible for the angle closure. It is crucial to clearly determine the patency of the PI by paying attention to the opening itself rather than the transillumination defect. If doubt remains, another PI should be performed. The most common entity to cause angle closure in the presence of a patent PI is the so-called malignant glaucoma. The pathogenic mechanism is multifactorial, including posterior aqueous misdirection and ciliary block by vitreous at the ciliary body. Characteristically, the anterior chamber is uniformly shallow and in extreme cases the vitreous or IOL can touch the endothelial surface. This entity is discussed in Chapter 12.
How Is Open-Angle Glaucoma in Aphakia and Pseudophakia Managed?
If open-angle glaucoma is present in aphakia or pseudophakia and it is not related to inflammatory lens-related mechanisms, the management is similar to that of POAG, with some exceptions. First, epinephrine derivatives are usually avoided due to the possibility of inducing cystoid macular edema.127,137 Second, strong miotics (e.g., cholinesterase inhibitors) can be used more freely as the risks of cataract formation or angle narrowing are less critical. Argon laser trabeculoplasty is the next therapeutic step and can be more effective in pseudophakia than in aphakia but overall less effective than in phakic eyes.28,138,139
When glaucoma filtering surgery becomes necessary in noninflamed aphakic and pseudophakic eyes with open angles, several considerations are worth mentioning. First, partial-thickness (guarded) operations with suture manipulation are currently preferred over full-thickness procedures due to the higher rate of complications with the latter technique. Second, due to altered conjunctival and Tenon’s capsule anatomy, the procedure is technically more difficult. Areas with mobile, nonadhered conjunctiva should be selected. Third, the rate of intra- and postoperative complications is increased in this group of patients. Finally, the long-term success rate is significantly decreased when compared to phakic eyes, although the precise causes of this phenomenon are poorly understood.139,140 Drainage devices are an alternative when filtering surgery has failed to control the glaucoma. Cyclodestructive procedures are usually the last resort. The reader is referred to Chapter 19 for a complete discussion of these matters.
How Is Angle-Closure Glaucoma in Aphakia and Pseudophakia Managed?
Only aspects specifically pertinent to the absence of the natural lens or the presence or an IOL are addressed in this section. The reader is referred to specific chapters when a more general approach is indicated.
The initial management of ACG regardless of the mechanisms involved depends on the level of IOP and status of the eye. In acute symptomatic cases, hyperosmotics and aqueous suppressants are indicated. Once the IOP has been lowered and the eye is quiet, any subsequent treatments have a greater chance of succeeding.
If an open PI is not present and an iris bombé configuration strongly suggests pupillary block, the treatment of choice is an Nd:YAG laser peripheral iridotomy. More than one may be needed if posterior synechiae have created loculated pockets of fluid behind the iris. Once the pupillary block has been, overcome the next issue is whether or not PAS is present. If the treatment is prompt, PAS may be prevented. Glaucoma filtering surgery may be necessary if the synechiae persist and less invasive procedures such as peripheral iridoplasty have not been effective. See Chapter 5 for a complete discussion on the treatment of acute and chronic secondary angle-closure glaucoma.
If a typical iris-bombé configuration is not present, or if doing the PI does not change the configuration of the anterior chamber, the possibility of aqueous misdirection should be raised. Of course, if an open PI was present on presentation, this would be the first diagnostic suspicion in a patient with a shallow anterior chamber and elevated IOP. See Chapters 12 and 19 for a complete discussion on malignant glaucoma.
Future Considerations
As practice patterns continue to evolve29 glaucoma in aphakia will become a rarity. The management of this entity will vary as new drugs and surgical techniques appear. Glaucoma in pseudophakia, on the other hand, may continue to be a challenge. Prevention through improved surgical techniques and early detection are essential to ensure a good visual outcome.
References
2. Ritch R, Shields BM (eds). The secondary glaucomas. St. Louis: CV Mosby, 1982.
5. Nelson LB, Maumenee IH: Ectopia lentis. Surv Ophthalmol 1982;27:143–160.
9. Seland JH: The lenticular attachment of the zonular apparatus in congenital simple ectopia lentis. Acta Ophthalmol 1973;51:520–528.
19. Maumenee IH: The eye in the Marfan syndrome. Trans Am Ophthalmol Soc 1981;79:684–733.
31. Epstein DL: Diagnosis and management of lens-induced glaucoma. Ophthalmology 1982;89:227–230.
57. Roth YB, Epstein DL: Exfoliation syndrome. Am J Ophthalmol 1980;89:700–707.
66. Roth M, Epstein DL: Exfoliation syndrome. Am J Ophthalmol 1980;89:477–481.
79. Madden JG, Crowley MJ: Factors in the exfoliation syndrome. Br J Ophthalmol 1982;66:432–437.
82. Sugar HS, Harding C, Barsky D: The exfoliation syndrome. Ann Ophthalmol 1976;8:1165–1181.
83. Caccamise WC: The exfoliation syndrome in the aphakic eye. Am J Ophthalmol 1981;91:111–112.
96. Bartholomew RS: Pseudoexfoliation and angle-closure glaucoma. Glaucoma 1981;3:213–217.
98. Mapstone R: Pigment release. Br J Ophthalmol 1981;65:258–263.
128. Moses L: Complications of rigid anterior chamber implants. Ophthalmology 1984;91:819–825.
140. Skuta GL, Parrish RK II: Wound healing in glaucoma filtering surgery. Surv Ophthalmol 1987;32:149–170.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree