Giant Retinal Tears: Surgical Approach
Derek Y. Kunimoto
Mitchell Fineman
Giant retinal tears are defined as circumferential retinal tears that extend 90 degrees (three clock hours) or more (Fig. 6-69.1). Most giant retinal tears are idiopathic, occur most commonly in males, and are associated with high myopia.1,2 The second most common cause of giant retinal tears is blunt ocular trauma. Systemic conditions, such as Marfan or Stickler syndrome, account for a few cases.3 Other rare causes of giant retinal tears include tears occurring along the posterior edge of large chorioretinal scars (e.g., as in acute retinal necrosis)4 and tears along the edge of large chorioretinal abnormalities (e.g., as in coloboma). The incidence of giant retinal tears is approximately 1 in 2 million people, and is present in about 1 in 200 rhegmatogenous retinal detachments.1
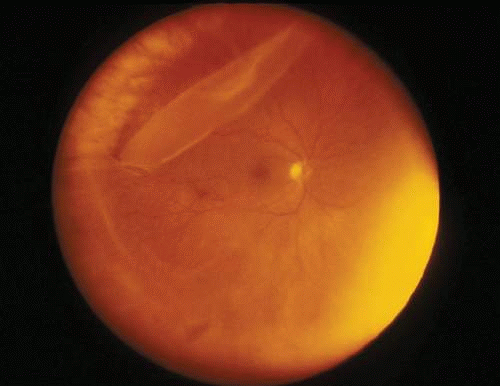 Figure 6-69.1. Equator-plus photograph of a right eye demonstrating a giant retinal tear as defined by a greater than 3 clock-hour retinal tear |
Giant retinal tears are distinguished from retinal dialyses by two features. First, retinal dialyses occur at the insertion of the retina at the ora serrata, whereas giant retinal tears occur more posteriorly; second, retinal dialyses have an intact overlying retina–vitreous interface, whereas giant retinal tears have a separated retina–vitreous interface posterior to the tear (Fig. 6-69.2). The distinction between these two entities is important because their management may differ.
 Figure 6-69.2. Digital color montage photograph demonstrating a superotemporal and temporal giant retinal tear with associated retinal detachment. The macula is still attached. |
Previously, the presence of a giant retinal tears has been associated with a poor visual prognosis. Advances in the last 30 years that have improved clinical outcomes of this entity include vitrectomy microsurgery, and the use of fluid-air exchange, perfluorocarbon liquids, and silicone oil.
Preoperative Examination
The edge of the tear should be examined to determine whether the overlying vitreous is attached both anteriorly and posteriorly. This helps in distinguishing giant retinal tears from retinal dialyses (Fig. 6-69.3). The edge of the tear should also be examined for edge inversion or folds, which can occur with epiretinal tissue proliferation, representing proliferative vitreoretinopathy (Fig. 6-69.4). Flap mobility can be tested by examining the patient in an upright and supine position. In cases of an inverted flap, some authors have found it helpful to examine the patient in the prone position, with the examiner lying underneath the examination table. In this position, if an inverted flap unfolds poorly, early proliferative vitreoretinopathy should be suspected.
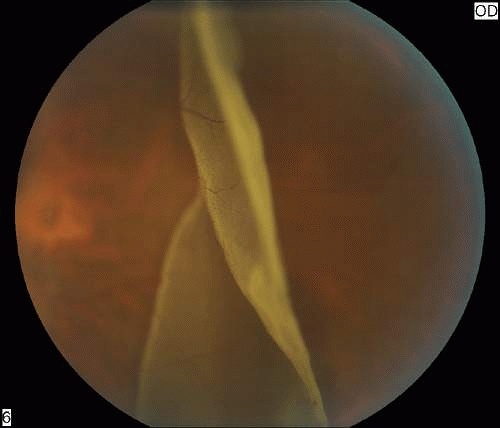 Figure 6-69.4. Color photograph demonstrating early proliferative vitreoretinopathy at the edge of the tear from the eye shown in Figure 2. |
The location of the break should be noted because this will affect the type of tamponade selected and the postoperative positioning. The presence and position of additional breaks will also influence whether a scleral buckle will be used and where it will be positioned.
Surgical Management
The general principles of managing giant retinal tears include unfolding the posterior flap of the tear, flattening the retina, and tacking down the retina with a chorioretinal adhesion.
Giant retinal tears without associated retinal detachment can be treated with demarcation laser retinopexy (Fig. 6-69.5). Postoperative follow-up is critical in these eyes because progression to retinal detachment can occur rapidly.
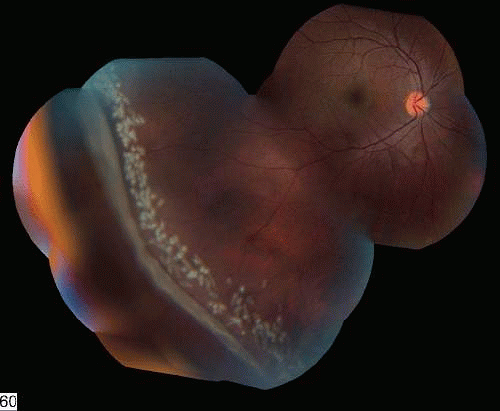 Figure 6-69.5. Digital color montage photograph of a right eye with a giant retinal tear without significant retinal detachment treated with demarcation laser retinopexy. |
The management of giant retinal tears associated with retinal detachment is surgical, including vitrectomy and possible scleral buckling. Adjunctive agents include perfluorocarbon liquids and silicone oil. Assessment of the patient’s lens status is important because giant retinal tears frequently occur in a predominantly phakic age group.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



