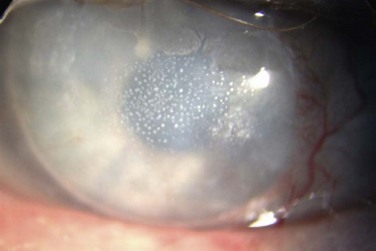
16 Giant papillary conjunctivitis is an inflammatory condition seen in the upper tarsal conjunctiva, initially reported by Spring in 1974.1 The author noted a papillary reaction, similar to that seen in patients with allergic conjunctivitis, though his findings were reported in soft contact lens wearers. Allansmith and colleagues further detailed the syndrome, suggesting that it may be immunologic in origin, with the proteinaceous deposits on the contact lenses serving as the antigen.2 As the constellation of findings is predominantly associated with the use of contact lenses, the disease is also referred to as contact lens-induced papillary conjunctivitis (CLPC); however, the condition has also been reported in patients with ocular dermoids, ocular prostheses, exposed sutures following ocular procedures, extruded scleral buckles, filtering blebs, exposed corneal deposits, as well as tissue adhesives (Fig. 16.1).3–10 Giant papillary conjunctivitis (GPC) is most often associated with wearing soft contact lenses, though it can occur with any type of contact lens. In a study of 221 patients, 85% were wearing soft contact lenses, with the remaining 15% of participants wearing rigid lenses.11 One report noted an average interval of 10 months for the development of GPC for soft lens wearers, compared to 8.5 years for rigid lens wearers.2 The type and material of the lens also contributes to the severity of the disease, with soft lens wearers suffering from more severe manifestations of disease than their counterparts in rigid gas-permeable lenses.11 Silicone hydrogel lenses also appear to have similar effects with prolonged use, though the findings are seen more commonly in earlier designs.12 Researchers have also studied the association of other atopic conditions in patients with GPC, due to the similarities between GPC and other immunologically derived ocular disorders (e.g. vernal keratoconjunctivitis). Allergic rhinitis and hay fever are often estimated to range 10–20% in the general population, and in the subset of GPC patients, the incidence has been reported to be as low as 12% to over 26%.11,13 One particular cohort reports that patients who suffer from allergies seem to have more severe signs and symptoms of GPC, compared to those who did not; however, the presence or absence of other allergic conditions did not have any effect on the ultimate treatment of those individuals or their long-term use of contact lenses.11 Neutrophils and lymphocytes are present in the epithelium and substantia propria of normal conjunctival tissue. Mast cells and plasma cells are also present, though they are sequestered to the substantia propria. In patients with GPC, these cells increase in number and are often found throughout the epithelium and the substantia propria, and are found in conjunction with other inflammatory cells, such as basophils and eosinophils.14 These findings, along with elevation of cytokines and chemokines in the tear film of GPC patients, suggest a possible allergic mechanism for the development of disease. Interleukin-6 (IL-6) along with IL-6 soluble receptor (IL-6sr) have been noted to be elevated four- to eightfold compared to controls, and IL-6sr has been postulated to be an important mediator in the formation of the papillae.15 Locally produced tear immunoglobulins (e.g. IgE, IgG, and even IgM in severe cases) are also found to be elevated in the tears of GPC patients, with the degree of elevation correlated to the severity of symptoms. It is interesting to note, that with discontinuation of lens wear and resolution of the signs and symptoms, these tear immunoglobulin levels return to normal.12 The proteinaceous deposits on the lens surface have classically been cited as the possible nidus for the development of inflammation and thus, the papillae associated with GPC. These various substances can cover 50% of the contact lens surface within 30 minutes of lens insertion, and 90% after 8 hours of wear time.16,17 Even with the best cleaning regimens involving enzymatic treatment, a residual coating still exists, and as new coating material is constantly built on the surface of the lens, the overall lens coating increases.18 The lens type and material also affect the rate and amount of accumulation of protein coating, as well as the total percentages of lipid, calcium and protein that deposit on the lens.12 Differences in the polymer content, structure and charge determine the extent to which protein is deposited on the anterior lens surface.19 The nature of these deposits is similar in patients with and without GPC. In addition, there are no morphologic or biochemical findings that differentiate the coating on the contact lenses in these two groups; however, those affected with GPC generally have more coating on their contact lenses, and lenses of GPC patients can promote a clinical picture of injection, thickening and a papillary reaction on the upper tarsal conjunctiva in monkeys in a laboratory setting.20 Cellular infiltrates seen in the biopsy samples from the monkeys are also similar to those seen in GPC; thus, the animal model strongly suggests that an antigen exists in the contact lens coating that may produce the same inflammatory reaction seen clinically as GPC.20 These findings support the allergic hypothesis for GPC, as does the fact that immunoglobulins G, A and M (IgG, IgA, and IgM), were also found in the protein deposits on GPC-associated contact lenses; however, eosinophil major basic protein, a material elaborated from eosinophils found in allergic reactions, was not found to a significant degree on lenses of GPC patients.21–24 In contrast, the mechanical hypothesis is supported by the association between GPC and inert objects, such as cyanoacrylate adhesives, exposed sutures or scleral buckle elements, dermoids and orbital prostheses. Researchers have postulated that the irritation and friction from the lens damages conjunctival epithelial cells and causes release of chemotactic factors (e.g. neutrophil chemotactic factor).24 Injection of these factors into the upper tarsal conjunctiva of rabbits produced a GPC-like reaction, suggesting that a combination of direct trauma and the resulting inflammatory cascade can stimulate a hypersensitivity reaction to lens-bound antigens. The biomicroscopic findings of normal tarsal conjunctiva, include a vascular arcade of fine, radiating vessels running perpendicular to the lid margin and a smooth, moist and pink surface. This has been termed a ‘satin’ appearance.2 Generally, the surface is devoid of papillae, or there may be a fine, fairly uniform papillary appearance detectable after the instillation of fluorescein dye and examination with a cobalt blue filter. These papillae, if present, are often smaller than 0.3 mm. Non-specific signs of inflammation, such as thickening of the tarsal conjunctiva with mild hyperemia, may be noted in early cases. In addition, bulbar conjunctival injection, superior corneal pannus, and corneal opacities may also be found on examination. As the disease progresses, non-uniform papillary changes develop, and finally giant papillae are seen, defined as a papillary reaction greater than 0.3 mm (Fig. 16.2).
Giant Papillary Conjunctivitis
Introduction
Epidemiology
Pathophysiology
Clinical Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ento Key
Fastest Otolaryngology & Ophthalmology Insight Engine