General Ophthalmic Problems
13.1 ACQUIRED CATARACT
Symptoms
Slowly progressive visual loss or blurring, usually over months to years, affecting one or both eyes. Glare, particularly from oncoming headlights while driving at night, and reduced color perception may occur, but not to the same degree as in optic neuropathies. The characteristics of the cataract determine the particular symptoms.
Signs
(See Figure 13.1.1.)
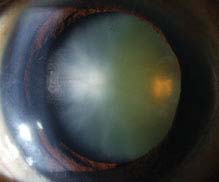
FIGURE 13.1.1. Cataract.
Critical. Opacification of the normally clear crystalline lens.
Other. Blurred view of the retina with dimming of red reflex on retinoscopy. Myopic shift or the so-called “second sight.” A cataract alone does not cause a relative afferent pupillary defect (RAPD).
Etiology
 Age-related: Most common. Mature, hypermature, and morgagnian.
Age-related: Most common. Mature, hypermature, and morgagnian.
 Presenile: Diabetes, myotonic dystrophy, and atopic dermatitis.
Presenile: Diabetes, myotonic dystrophy, and atopic dermatitis.
 Trauma: Penetrating, concussion (vossius ring), and electric shock.
Trauma: Penetrating, concussion (vossius ring), and electric shock.
 Toxic: Steroids, miotics, antipsychotics (e.g., phenothiazines), and others.
Toxic: Steroids, miotics, antipsychotics (e.g., phenothiazines), and others.
 Secondary.
Secondary.
—Chronic anterior uveitis. See 12.1, Anterior Uveitis (Iritis/Iridocyclitis).
—Ionizing radiation.
—Tumor (ciliary body).
—Acute angle-closure glaucoma: Glaucom-flecken. See 9.4, Acute Angle-Closure Glaucoma.
—Degenerative ocular disease: Retinitis pigmentosa, Leber congenital amaurosis, Gyrate atrophy, Wagner and Stickler syndromes associated with posterior subcapsular cataracts, and others.
 Endocrine/Metabolic.
Endocrine/Metabolic.
—Diabetes: Juvenile form characterized by rapidly progressing white “snowflake” opacities in the anterior and posterior subcapsular locations. Age-related cataracts form earlier than in nondiabetics.
—Hypocalcemia: Small, white, iridescent cortical changes, usually seen in the presence of tetany.
—Wilson disease: Red–brown pigment deposition in the cortex beneath the anterior capsule (a “sunflower” cataract). See 13.9, Wilson Disease.
—Myotonic dystrophy: Multicolored opacities, “Christmas-tree cataract,” behind the anterior capsule.
—Others: Down syndrome, Neurofibromatosis Type 2 (posterior subcapsular cataract), etc.
Types
1. Nuclear: Yellow or brown discoloration of the central lens. Typically blurs distance vision more than near (myopic shift).
2. Posterior subcapsular: Plaque-like opacity near the posterior aspect of the lens. Best seen in retroillumination against the red reflex. Glare and difficulty reading are common complaints. Associated with ocular inflammation, steroid use, diabetes, trauma, or radiation. Classically occurs in patients <50 years of age.
3. Cortical: Radial or spoke-like opacities in the periphery that expand to involve the anterior and posterior lens and can cause glare. Often asymptomatic until central changes develop.
NOTE: A mature cataract is defined as lenticular changes sufficiently dense to totally obscure the view of the posterior lens and posterior segment of the eye. No iris shadow is seen on oblique illumination at the pupillary margin. Rarely, the cortex may liquefy and the nucleus becomes free-floating within the capsule, this is known as a hypermature or Morgagnian cataract. If the liquefied cortex leaks through the intact capsule, wrinkling of the lens capsule may be seen and phacolytic glaucoma may develop. See 9.12.1, Phacolytic Glaucoma.
Work-Up
Determine the etiology, whether the cataract is responsible for the decreased vision, and whether surgical removal would improve vision.
1. History: Medications? [e.g., tamsulosin or any medications used for urinary retention (alpha-1 blockers) strongly associated with intraoperative floppy iris syndrome] Systemic diseases? Trauma? Ocular disease or poor vision before the cataract?
2. Complete ocular examination, including distance and near vision, pupillary examination, and refraction. A dilated slit-lamp examination using both direct and retroillumination techniques is required to view the cataract properly. Fundus examination, concentrating on the macula, is essential in ruling out other causes of decreased vision.
3. For preoperative planning, note the degree of pupil dilation, density of the cataract, and presence or absence of pseudoexfoliation syndrome, phacodonesis (quivering of the lens indicating zonular damage or weakness), or cornea guttata.
4. B-scan ultrasonography (US) if the fundus is obscured to rule out detectable posterior segment disease.
5. The potential acuity meter (PAM) or laser interferometry can be used to estimate the visual potential when cataract extraction is considered in an eye with posterior segment disease.
NOTE: Laser interferometry and PAM often overestimate the eye’s visual potential in the presence of macular holes or macular pigment epithelial detachments. Interferometry also overestimates results in cases of amblyopia. Near vision is often the most accurate manner of evaluating macular function if the cataract is not too dense. Nonetheless, both laser interferometry and PAM are useful clinical tools.
6. Keratometry readings and an A-scan US measurement of axial length are required for determining the power of the desired intraocular lens (IOL). Corneal pachymetry or endothelial cell count is occasionally helpful if cornea guttata are present.
Treatment
1. Cataract surgery may be performed for the following reasons:
—To improve visual function in patients with symptomatic visual disability.
—As surgical therapy for ocular disease (e.g., lens-related glaucoma or uveitis).
—To facilitate management of ocular disease (e.g., to allow a view of the fundus to monitor or treat diabetic retinopathy or glaucoma).
2. Correct any refractive error if the patient declines cataract surgery.
3. A trial of mydriasis (e.g., scopolamine 0.25% q.d.) may be used successfully in some patients who desire nonsurgical treatment. The benefits of this therapy are only temporary. Most useful for posterior subcapsular cataracts.
Follow-Up
Unless there is a secondary complication from the cataract (e.g., glaucoma), a cataract itself does not require urgent action. Patients who decline surgical removal are reexamined annually, sooner if symptoms worsen.
If congenital, see 8.8, Congenital Cataract.
13.2 PREGNANCY
ANTERIOR SEGMENT CHANGES
Transient loss of accommodation and increased corneal thickness/edema and curvature. Refractive change likely results from a shift in fluid or hormonal status and will likely normalize after delivery. Defer prescribing new glasses until several weeks postpartum.
PREECLAMPSIA/ECLAMPSIA
A worldwide leading cause of maternal/fetal/neonatal morbidity and mortality. Occurs in 2% to 5% of pregnancies but may approach 10% in developing countries. Occurs after 20 weeks of gestation; most commonly in primigravids.
Symptoms
Headaches, blurred vision, photopsias, diplopia, and scotomas.
Signs
Systemic
 Preeclampsia or pregnancy-induced hypertension: Hypertension and proteinuria in previously normotensive women. Other signs include peripheral edema, liver failure, renal failure, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet counts).
Preeclampsia or pregnancy-induced hypertension: Hypertension and proteinuria in previously normotensive women. Other signs include peripheral edema, liver failure, renal failure, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet counts).
 Eclampsia: Preeclampsia with seizures.
Eclampsia: Preeclampsia with seizures.
Ocular. Focal retinal arteriolar spasm and narrowing, peripapillary or focal areas of retinal edema, retinal hemorrhages, exudates, nerve fiber layer infarcts, vitreous hemorrhage secondary to neovascularization, serous retinal detachments in 1% of preeclamptic and 10% of eclamptic patients, acute nonarteritic ischemic optic neuropathy, and bilateral occipital lobe infarcts (preeclampsia–eclampsia hypertensive posterior encephalopathy syndrome, or PEHPES). Differential diagnosis of PEHPES includes posterior circulation stroke, infectious cerebritis, coagulation disorder causing intracranial venous thrombosis, intracranial hemorrhage, occult tumor with secondary bleed, migraines, atypical seizure, or demyelination.
Natural History
1. Magnetic resonance imaging (MRI) abnormalities resolve 1 to 2 weeks after blood pressure control, at which time complete neurologic recovery can be expected.
2. Serous retinal detachments; often bilateral and bullous; resolve postpartum with residual pigment epithelial changes (see Figure 13.2.1).
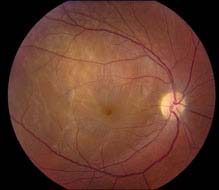
FIGURE 13.2.1. Serous macular detachment in a patient with preeclampsia.
3. Retinal vascular changes also normalize postpartum.
Work-Up
1. Complete neuro-ophthalmologic and fundus examinations. Poor vision with brisk pupils without an RAPD suggests occipital lesions.
2. MRI findings in PEHPES include bilateral occipital lobe lesions involving subcortical white matter with possible extension into the gray–white junction, cortical surface, external capsule, and basal ganglia. MRI abnormalities are identical in obstetric and nonobstetric hypertensive encephalopathy.
3. With typical presentation, further invasive studies are discouraged.
4. Systemic work-up, including blood pressure monitoring and urinalysis, in conjunction with an OB/GYN specialist.
Treatment
1. Control blood pressure and electrolyte imbalances.
2. Prompt delivery ideal.
OCCLUSIVE VASCULAR DISORDERS
Pregnancy represents a hypercoagulable state possibly resulting in the development of retinal artery and vein occlusions, disseminated intravascular coagulopathy (DIC), and thrombotic thrombocytopenia purpura. Ocular DIC is characterized by widespread small-vessel thrombosis, particularly in the choroid, associated with hemorrhage, tissue necrosis, and serous retinal detachments.
MENINGIOMA OF PREGNANCY
Meningiomas may have a very aggressive growth pattern during pregnancy that is difficult to manage. They may regress postpartum but may reoccur during subsequent pregnancies.
NOTE: All pregnant women complaining of a headache should have their blood pressure, visual fields, and fundus checked (particularly looking for papilledema). MRI/MRV or lumbar puncture is often required if a hemorrhage or cortical venous thrombosis is suspected.
OTHER CONDITIONS INFLUENCED BY PREGNANCY
Multiple conditions can be impacted by pregnancy. See 3.19, Purtscher Retinopathy; 10.10, Cavernous Sinus and Associated Syndromes (Multiple Ocular Motor Nerve Palsies); 10.16, Idiopathic Intracranial Hypertension/Pseudotumor Cerebri; 10.27, Migraine; 11.12, Diabetic Retinopathy; and 11.15, Central Serous Chorioretinopathy. Medications deserve special attention during pregnancy.
13.3 LYME DISEASE
Symptoms
Decreased vision, double vision, pain, photophobia, facial weakness. Also may have headache, malaise, fatigue, fever, chills, palpitations, or muscle or joint pains. A history of a tick bite within the previous few months may be elicited.
Signs
Ocular. Optic neuritis; vitritis; iritis; stromal keratitis; choroiditis; exudative retinal detachment; third, fourth, or sixth cranial nerve palsy; bilateral optic nerve swelling; conjunctivitis; episcleritis; exposure keratopathy; other rare abnormalities, including idiopathic orbital inflammatory syndrome. See specific sections.
Critical Systemic. One or more flat, erythematous or “bull’s-eye” skin lesions, which enlarge in all directions (erythema migrans); unilateral or bilateral facial nerve palsies; polyarticular migratory arthritis. May not be present at the time the ocular signs develop. A high serum antibody titer against Borrelia burgdorferi, is often, but not always present.
Other Systemic. Meningitis, peripheral radiculoneuropathy, synovitis, joint effusions, cardiac abnormalities, or a low false-positive FTA-ABS titer.
Differential Diagnosis
 Syphilis: High-positive FTA-ABS titer may produce a low false-positive antibody titer against B. burgdorferi. See 12.12, Syphilis.
Syphilis: High-positive FTA-ABS titer may produce a low false-positive antibody titer against B. burgdorferi. See 12.12, Syphilis.
 Others: Rickettsial infections, acute rheumatic fever, juvenile idiopathic arthritis, sarcoidosis, tuberculosis, herpes virus infections, etc.
Others: Rickettsial infections, acute rheumatic fever, juvenile idiopathic arthritis, sarcoidosis, tuberculosis, herpes virus infections, etc.
Work-Up
1. History: Does patient live in endemic area? Prior tick bite, skin rash, facial nerve palsy, joint or muscle pains, flulike illness? Meningeal symptoms? Prior positive Lyme titer?
2. Complete systemic, neurologic, and ocular examinations.
3. Two-step diagnosis with a screening assay and confirmatory Western blot for B. burgdorferi.
4. Serum RPR and FTA-ABS. Consider serum ACE, chest x-ray, and PPD.
5. Consider lumbar puncture when meningitis is suspected or neurologic signs or symptoms are present.
Treatment
Early Lyme Disease (Including Lyme-Related Uveitis, Keratitis, or Facial Nerve Palsy):
1. Doxycycline 100 mg p.o. b.i.d. for 10 to 21 days.
2. In children, pregnant women, and those who cannot take doxycycline, substitute amoxicillin 500 mg p.o. t.i.d., cefuroxime axetil 500 mg p.o. b.i.d., clarithromycin 500 mg p.o. b.i.d., or azithromycin 500 mg p.o. q.d.
Patients with Neuro-ophthalmic Signs or Recurrent or Resistant Infection:
1. Ceftriaxone 2 g intravenously q.d. for 2 to 3 weeks.
2. Alternatively, penicillin G, 20 million units intravenously q.d. for 2 to 3 weeks.
Follow-Up
Every 1 to 3 days until improvement is demonstrated, and then weekly until resolved.
13.4 CONVERGENCE INSUFFICIENCY
Symptoms
Eye discomfort or blurred vision from reading or near work. Most common in young adults, but may be seen in older people.
Signs
Critical. An exophoria at near in the presence of poor near-fusional convergence amplitudes, a low accommodative convergence/accommodation (AC/A) ratio, and a remote near point of convergence.
Differential Diagnosis
 Uncorrected refractive error: Hyperopia or over-minused myopia.
Uncorrected refractive error: Hyperopia or over-minused myopia.
 Accommodative insufficiency (AI): Often in prepresbyopia age range from uncorrected low hyperopia or over-minused myopia. While reading, a 4-diopter base-in prism placed in front of the eye blurs the print in AI, but improves clarity in CI. Rarely, adolescents may develop transient paresis of accommodation, requiring reading glasses or bifocals. This idiopathic condition resolves in several years. Patients with AI may benefit from reading glasses with base-in prism.
Accommodative insufficiency (AI): Often in prepresbyopia age range from uncorrected low hyperopia or over-minused myopia. While reading, a 4-diopter base-in prism placed in front of the eye blurs the print in AI, but improves clarity in CI. Rarely, adolescents may develop transient paresis of accommodation, requiring reading glasses or bifocals. This idiopathic condition resolves in several years. Patients with AI may benefit from reading glasses with base-in prism.
 Convergence paralysis: Acute onset of exotropia and diplopia on near fixation only; normal adduction and accommodation. Usually results from a lesion in the corpora quadrigemina or the third cranial nerve nucleus, and may be associated with Parinaud syndrome.
Convergence paralysis: Acute onset of exotropia and diplopia on near fixation only; normal adduction and accommodation. Usually results from a lesion in the corpora quadrigemina or the third cranial nerve nucleus, and may be associated with Parinaud syndrome.
NOTE: A diagnosis of convergence paralysis should prompt neuroimaging to rule out an intracranial lesion.
Etiology
 Fatigue or illness.
Fatigue or illness.
 Drugs (parasympatholytics).
Drugs (parasympatholytics).
 Uveitis.
Uveitis.
 Adie tonic pupil.
Adie tonic pupil.
 Glasses inducing a base-out prism effect.
Glasses inducing a base-out prism effect.
 Post-exanthematous encephalitis.
Post-exanthematous encephalitis.
 Traumatic injury.
Traumatic injury.
 Idiopathic.
Idiopathic.
Work-Up
1. Manifest (without cycloplegia) refraction.
2. Determine the near point of convergence: Ask patient to focus on an accommodative target (e.g., a pencil eraser) and to state when double vision develops as you bring the target toward them; a normal near point of convergence is <8 cm.
3. Check for exodeviations or esodeviations at distance and near using the cover tests (see Appendix 3, Cover/Uncover and Alternate Cover Tests) or the Maddox rod test.
4. Measure the patient’s fusional ability at near. Have patient focus on an accommodative target at their reading distance. With a prism bar, slowly increase the amount of base-out prism in front of one eye until patient notes double vision (the break point), and then slowly reduce the amount of base-out prism until a single image is again noted (the recovery point). A low break point (10 to 15 prism diopters), a low recovery point, or both, are consistent with CI.
5. Place a 4-diopter base-in prism in front of one eye while patient is reading. Determine whether the print becomes clearer or more blurred to rule out AI.
6. Perform cycloplegic refraction after the previous tests.
NOTE: These tests are performed with the patient’s spectacle correction in place (if glasses are worn for near work).
Treatment
1. Correct any refractive error. Slightly undercorrect hyperopia, and fully correct myopia.
2. Near-point exercises (e.g., pencil push-ups): The patient focuses on a pencil eraser while slowly moving it from arm’s length toward the face. Concentrate on maintaining one image of the eraser, repeating the maneuver when diplopia manifests. Try to bring the pencil in closer each time while maintaining single vision. Repeat the exercise 15 times, 5 times per day.
3. Near-point exercises with base-out prisms (for patients whose near point of convergence is satisfactory or for those who have mastered pencil push-ups without a prism): The patient performs pencil push-ups as described previously, while holding a 6-diopter base-out prism in front of one eye.
4. Encourage good lighting and relaxation time between periods of close work.
5. For older patients, or those whose condition shows no improvement despite near-point exercises, reading glasses with base-in prism can be useful.
Follow-Up
Nonurgent. Patients are reexamined in 1 month.
13.5 ACCOMMODATIVE SPASM
Symptoms
Bilateral blurred distance vision, fluctuating vision, blurred vision when shifting gaze from near to far, headache, and eye strain while reading. Often seen in teenagers under stress. Symptoms may occur after prolonged and intense periods of near work.
Signs
Critical. Cycloplegic refraction reveals substantially less myopia (or more hyperopia) than was originally found when the refraction was performed without cycloplegia (manifest refraction). Manifest myopia may be as high as 10 diopters. Spasm of the near reflex is associated with excess accommodation, excess convergence, and miosis.
Other. Abnormally close near point of focus, miosis, and a normal amplitude of accommodation that may appear low.
Etiology
 Inability to relax the ciliary muscles. Involuntary and associated with stressful situations or functional neuroses.
Inability to relax the ciliary muscles. Involuntary and associated with stressful situations or functional neuroses.
 Fatigue.
Fatigue.
 Prolonged reading may precipitate episodes.
Prolonged reading may precipitate episodes.
Differential Diagnosis
 Uncorrected hyperopia: Increased plus accepted during manifest refraction.
Uncorrected hyperopia: Increased plus accepted during manifest refraction.
 Other causes of pseudomyopia: Hyperglycemia, medication induced (e.g., sulfa drugs and anticholinesterase medications), anterior displacement of the lens-iris diaphragm.
Other causes of pseudomyopia: Hyperglycemia, medication induced (e.g., sulfa drugs and anticholinesterase medications), anterior displacement of the lens-iris diaphragm.
 Manifestation of iridocyclitis.
Manifestation of iridocyclitis.
Work-Up
1. Complete ophthalmic examination. The manifest refraction may be highly variable, but it is important to determine the least amount of minus power or the most amount of plus power that provides clear distance vision.
2. Cycloplegic refraction.
Treatment
1. True refractive errors should be corrected. If a significant amount of esophoria at near is present, additional plus power (e.g., +2.50 diopters) in reading glasses or bifocal form may be helpful.
2. Counseling patient and parents to provide a more relaxed atmosphere and avoid stressful situations.
3. Cycloplegics have been used to break the spasm, but are rarely needed except in resistant cases.
Follow-Up
Reevaluate in several weeks.
13.6 STEVENS–JOHNSON SYNDROME (ERYTHEMA MULTIFORME MAJOR)
Symptoms
Acute onset of fever, rash, red eyes, malaise, arthralgias, and respiratory tract symptoms.
Signs
Systemic. Classic “target” skin lesions (maculopapules with a red center and a white surrounding area on an erythematous base) concentrated on hands and feet; ulcerative stomatitis; and hemorrhagic lip crusting. Mortality rate is 10% to 33%.
Ocular
 Acute phase: Mucopurulent or pseudomembranous conjunctivitis, episcleritis, and iritis.
Acute phase: Mucopurulent or pseudomembranous conjunctivitis, episcleritis, and iritis.
 Late complications: Conjunctival scarring and symblepharon; trichiasis; eyelid deformities; tear deficiency; corneal neovascularization, ulcer, perforation, or scarring.
Late complications: Conjunctival scarring and symblepharon; trichiasis; eyelid deformities; tear deficiency; corneal neovascularization, ulcer, perforation, or scarring.
Etiology
Precipitated by many agents, including:
 Drugs: Sulfonamides, barbiturates, chlorpropamide, thiazide diuretics, phenytoin, salicylates, allopurinol, chlormezanone, corticosteroids, isoniazid, tetracycline, codeine, aminopenicillins, chemotherapeutic agents, and others.
Drugs: Sulfonamides, barbiturates, chlorpropamide, thiazide diuretics, phenytoin, salicylates, allopurinol, chlormezanone, corticosteroids, isoniazid, tetracycline, codeine, aminopenicillins, chemotherapeutic agents, and others.
 Infectious agents: Most commonly Mycoplasma pneumoniae, herpes simplex virus, and adenovirus.
Infectious agents: Most commonly Mycoplasma pneumoniae, herpes simplex virus, and adenovirus.
 Allergy and autoimmune diseases.
Allergy and autoimmune diseases.
 Genetics: HLA B-12 may confer increased risk.
Genetics: HLA B-12 may confer increased risk.
 Radiation therapy.
Radiation therapy.
 Malignancy.
Malignancy.
Types
1. Erythema multiforme minor: Only skin involvement.
2. Erythema multiforme major (Stevens–Johnson syndrome): Immune complex deposition in dermis with subepithelial vesiculobullous reaction of skin and mucous membranes.
3. Toxic epidermal necrolysis: Most severe form with extensive vesiculobullous eruptions and epidermal sloughing. More common in children and immunosuppressed patients.
Work-Up
1. History: Attempt to determine the precipitating factor.
2. Slit-lamp examination, including eyelid eversion with examination of the fornices.
3. Conjunctival or corneal cultures if infection is suspected. See Appendix 8, Corneal Culture Procedure.
4. Consult Internal Medicine for a systemic work-up.
5. Skin biopsy may aid in the diagnosis.
Treatment
1. Hospitalization, often requiring burn unit if available.
2. Remove (e.g., drug) or treat (e.g., infection) the inciting factor.
3. Supportive care is the mainstay of therapy.
4. Co-management with Dermatology and Internal Medicine.
Ocular:
a. Tear deficiency: Aggressive lubrication with preservative-free artificial tears, gels, and ointments. Topical cyclosporine 0.05%, punctal occlusion, moisture chambers, or tarsorrhaphy.
b. Iritis: Topical steroid drops (e.g., prednisolone acetate 1% four to eight times per day) and cycloplegic (e.g., atropine 1% t.i.d.).
c. Infections: Treat as outlined in 4.11, Bacterial Keratitis.
d. Controversial treatments:
—Topical steroids for ocular surface inflammation.
—Daily pseudomembrane peel and symblepharon lysis with glass rod or moistened cotton swab.
—Systemic or topical vitamin A.
—Intravenous immunoglobulin.
Systemic: Manage by burn unit protocol, including hydration, wound care, and system antibiotics. Medical and dermatological consultation recommended.
Follow-Up
1. During hospitalization: Follow daily, with infection and IOP surveillance.
2. Outpatient: Weekly follow-ups initially, watching for long-term ocular complications.
—Topical steroids and antibiotics are maintained for 48 hours after resolution and are then tapered.
—If there is severe conjunctival scarring, artificial tears and lubricating ointment may need to be maintained indefinitely.
3. Possible late surgical interventions.
—Trichiasis: Repeated epilation, electrolysis, cryotherapy, or surgical repair.
—Entropion repair with buccal mucosal grafts.
—Penetrating keratoplasty: Poor prognosis even when combined with limbal stem cell or amniotic membrane transplantation because of underlying deficiencies, such as dry eyes and limbal stem cell abnormality.
—Permanent keratoprosthesis.
13.7 VITAMIN A DEFICIENCY
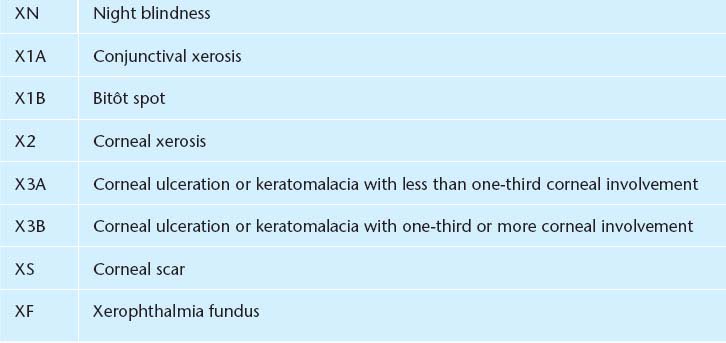
See Table 13.7.1.
TABLE 13.7.1 World Health Organization Classification of Vitamin A Deficiency
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


