Fundus Autofluorescence of Intraocular Tumors: Choroidal Nevus and Melanoma
Daniel Lavinsky
Rubens Belfort Mattos Neto
Eduardo V. Navajas
Rubens Belfort Mattos Jr.
Choroidal melanoma is the most frequent primary intraocular tumor and the second most frequent malignant melanoma of the body (1). Although it is a malignancy of the melanocytic cells of the choroid, it directly affects the retinal pigment epithelium (RPE). This secondary epitheliopathy appears as areas of atrophy, drusen, lipofuscin accumulation, and localized detachment of the RPE (2).
Large tumors are not difficult to diagnose as malignant, but the differential diagnosis and management of small choroidal melanomas remains controversial. Documented growth of a recently diagnosed small choroidal melanocytic lesion is considered a hallmark for the diagnosis of choroidal melanomas, and quantitative (tumor size) and qualitative factors, such as symptoms, drusen, subretinal fluid, RPE changes, juxtapapillary location, and orange pigmentation, may be predictive of tumor growth in patients with these melanocytic lesions (3).
Secondary epitheliopathy and particularly orange pigmentation overlying the lesion have been described as a major risk factors for progression to melanoma (2,4, 5, 6). Orange pigment, indicative of lipofuscin accumulation within the RPE, overlying small choroidal melanocytic lesions has been found to be significantly correlated with the risk of subsequent growth (3,7).
Recently, several groups have investigated the role of fundus autofluorescence (AF) in the diagnosis and prognosis of choroidal lesions (8, 9, 10, 11, 12). It is accepted that the AF signal in the fundus comes predominantly from lipofuscin in the RPE (see also Chapter 3). Thus, AF imaging may provide important information regarding patients with choroidal tumors.
BASIC PRINCIPLES
In 1976, Shields et al. (13) demonstrated that lipofuscin accumulates in RPE cells and macrophages of malignant choroidal tumors from incomplete degradation and digestion of photoreceptor outer segments. It is usually seen as orange pigment over the lesion; however, depending on whether the tumor is melanotic or amelanotic, the color may vary from orange to brown or red-brown, respectively.
Lipofuscin is a mixture of proteins, lipids, and small chromophores, and its accumulation in the RPE results from impaired or overwhelmed lysosomal digestive activity (see Chapters 1 and 2). Evidence demonstrates that lipid peroxidation-derived protein modifications are able to induce lysosomal dysfunction and lipofuscinogenesis in the RPE, and suggests that such lipid peroxidation-induced lysosomal dysfunction
considerably contributes to cell damage and subsequent retinal degeneration (14). The exact mechanism by which choroidal melanoma induces lipofuscinogenesis remains to be elucidated.
considerably contributes to cell damage and subsequent retinal degeneration (14). The exact mechanism by which choroidal melanoma induces lipofuscinogenesis remains to be elucidated.
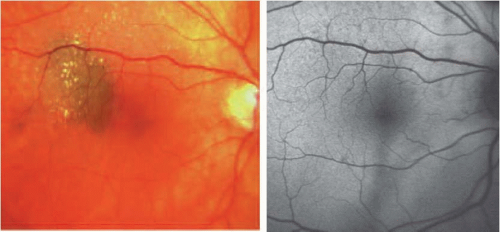
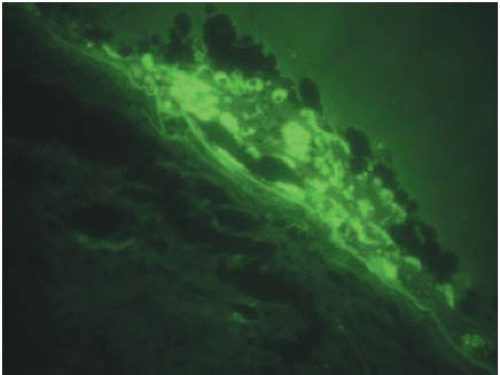 FIGURE 15.1. Autofluorescent deposits within the RPE and macrophages overlying the choroidal melanoma seen by fluorescence microscopy. |
In one histopathologic study (15), retina overlying choroidal melanoma showed areas of degeneration of outer retinal layers with a reduction in the number of nuclei of photoreceptors. Sheets of proliferated RPE cells and clusters of pigment-laden macrophages were present under the degenerated neurosensory retina, corresponding in position to the orange pigment observed in the macroscopic view of the tumor. On electron microscopy, most of the pigment granules appeared round to oval and demonstrated moderate homogeneous density with irregularly indented outlines, similar to typical lipofuscin granules normally observed throughout the retina to a lesser extent, and different from melanin granules.
Histochemical analysis indicates that orange pigment in macrophages and RPE cells of tumors stains positive for PAS, Sudan black B, and Long Ziehl-Nielsen (8); reduces silver salts with the Fontana-Masson method; bleaches partially with potassium permanganate; and is acid-fast and oil red O positive in paraffin sections. It also exhibits a golden-yellow AF when examined with ultraviolet light or a fluorescence microscope, suggesting that this pigment is in fact lipofuscin (Fig. 15.1) (15). Lohmann and colleagues (16) studied the endogenous fluorescence of ocular malignant melanomas and found that lipofuscin granules were cleaved off and broken into small remnants in the melanoma.
CLINICAL CHARACTERIZATION AND FUNDUS AUTOFLUORESCENCE FEATURES
Choroidal Nevus
A choroidal nevus can be classified clinically according to the Collaborative Ocular Melanoma Study (COMS). Benign lesions are usually less than 1 mm in height and 5 mm in basal diameter according to ultrasound measurements, and have no risk factors for growth, such as specific symptoms, orange pigmentation, subretinal fluid,
juxtapapillary location, and “hot spots” on angiography. Nevi may be brown to gray in color and their appearance may vary from homogeneous, small, flat, and well delineated to more heterogeneous with secondary changes overlying the nevus, such as drusen and pigment mottling.
juxtapapillary location, and “hot spots” on angiography. Nevi may be brown to gray in color and their appearance may vary from homogeneous, small, flat, and well delineated to more heterogeneous with secondary changes overlying the nevus, such as drusen and pigment mottling.
AF in choroidal nevus may show a normal pattern of background fundus AF, with no areas of increased or decreased AF signal, indicating a lack of RPE involvement (Fig. 15.2). Most nevi will demonstrate this pattern (8). In a minority of cases, nevi may also reveal areas with mild decreased or increased AF signal (11). The size of these lesions does not appear to influence the AF pattern, since large lesions may show normal background AF and small lesions with some RPE chronic degeneration may have a faint increased or decreased AF signal.
Drusen, often overlying nevus, when large or coalescent, may appear as areas of localized increased AF. However, the increased AF signal under these circumstances may not be a sign of lipofuscin accumulation in the RPE, such as occurs in choroidal melanoma; rather, it may result from the accumulation of different fluorophores inside these large drusen of drusenoid detachments, or relate to the presence of detached RPE cells within the latter.
Pirondini et al. (11) observed drusen in 56% of nevi, the majority of which demonstrated no changes in the distribution of AF or a traced increased AF signal. Less commonly, a reduced AF signal was also detected. Another clinical feature of nevus, although seen less commonly than drusen, is overlying RPE atrophy, which is easily identified as areas of low AF signal on AF images.
Choroidal Melanoma
Choroidal melanoma may appear as a pigmented lesion with orange pigment in a reticular or confluent pattern throughout its surface. Other features present in this lesion are subretinal fluid, superficial fibrosis with RPE metaplasia, and adjacent retinal detachment.
In the majority of cases, fundus AF correlates with the presence of orange pigmentation within choroidal melanoma. Gunduz et al. (9) found a complete
correlation between an increased AF signal and orange pigment in 61.5% of tumors, a partial correlation in 23.1%, and no correlation in only 15.4%.
correlation between an increased AF signal and orange pigment in 61.5% of tumors, a partial correlation in 23.1%, and no correlation in only 15.4%.
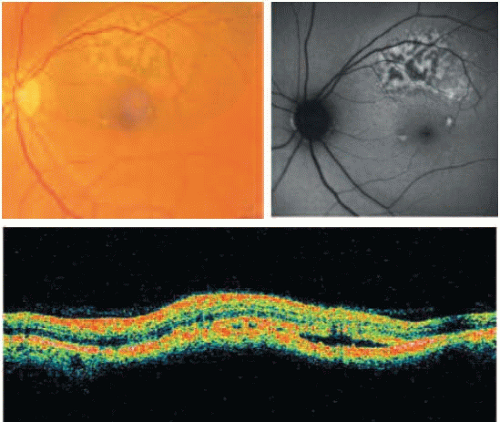 FIGURE 15.3. Correlation between orange pigmentation and subretinal fluid on AF images and OCT (horizontal scan) in a choroidal melanoma.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|