OVERVIEW
- The presence of a foreign body is a common occurrence in ENT practice
- Foreign bodies may be organic or inorganic. The former tend to be hydrophilic and therefore will expand over time and should be dealt with promptly
- Sharp objects also require urgent removal, especially if present in the aero-digestive tract
- Miniature batteries wherever lodged or placed—ear, nose or throat MUST be removed immediately, otherwise corrosive injury will follow and this may result in serious complications
- Food bolus without bone may be treated conservatively for 24–48 h with a muscle relaxant, prokinetic agent and analgesia
- Sharp foreign bodies in the throat, tend to lodge in the tonsils, posterior tongue base, valleculae or piriform fossae and may require a general anaesthetic for removal
- Uncooperative children usually require a general anaesthesia for removal of a foreign body within the ear, nose or throat
- Chest X-ray can be normal with an aerodigestive foreign body, so if in doubt it is safer to perform direct endoscopic examination
Introduction
The presence of a foreign body in the ear, nose or aerodigestive tract is a common occurrence in ENT practice. It can be a serious and challenging condition associated with considerable morbidity and mortality. Reports from The National Safety Council of America show that foreign bodies in the aerodigestive tract are the most common cause of accidental death in children under 6 years old.
Aural foreign bodies
Aural foreign bodies may present as incidental findings on otoscopy, or with otalgia, otorrhoea and hearing loss. They are most frequent in children under 10 years. Generally, foreign bodies in the ear or elsewhere may be classified as organic (e.g. peanuts, insects) or inorganic (e.g. beads, pins). The former tend to set up an intense inflammatory hydrophilic reaction and therefore must be dealt with promptly. The latter may also require urgent treatment if sharp or a button battery because of the potential to cause significant tissue damage. There is usually no urgency to remove smooth blunt inorganic objects. Insects in the external auditory canal may be drowned instantly with either alcohol or olive oil.
Retrieval
Patients are best managed under the operating microscope in the ENT emergency clinic. Removal is achieved with the use of a Jobson Horne probe, wax hook, suction and/or microforceps. Success is usually accomplished with a raking action. Irrigation should be avoided as organic materials will expand. Blind instrumentation may cause trauma to the canal or tympanic membrane and may impale the foreign material through the eardrum.
Rarely, if a large object is lodged deep in the ear canal, medial to the bony isthmus, or associated with otitis externa, the inflammation may be so severe that the meatus becomes very narrow or closed. Here, a general anaesthetic and a small endaural incision may be required. A general anaesthetic may also be needed to remove aural foreign bodies in young children, who are unable to cooperate.
Nasal foreign bodies
Nasal foreign bodies may present acutely or even after many years. They are most commonly found among 2- to 3-year-old toddlers, impacted between the septum and inferior turbinate and often visible on anterior rhinoscopy.
Organic materials such as tissue paper, sponge or nuts, provoke a profuse inflammatory reaction from the nasal mucosa. Initially the discharge is mucoid but eventually it becomes mucopurulent, and sometimes bloodstained. Inflammation and infection of the sinuses may cause further complications.
Furthermore, a secondary inflammatory response of the nasal vestibular skin (vestibulitis) may develop as a result of the constant discharge. For these reasons, any foul-smelling unilateral nasal discharge in a child, with or without excoriation of the vestibular skin, must be assumed to be due to a foreign body until proven otherwise. This may require examination of both nasal cavities under general anaesthetic.
Retrieval
Foreign bodies, particularly inorganic items, are removed by grasping the object firmly with crocodile forceps or by passing a blunt hook distal to the foreign body and slowly drawing it forward. A microsuction catheter may be used to withdraw objects such as polystyrene beads. Care should be taken not to let the child swallow the object as it is delivered from the nasal cavity. One attempt at removal is usually possible before the child becomes uncooperative. The use of a general anaesthetic may be required.
A battery inserted into the nasal cavity requires urgent examination under general anaesthesia with a good light source, as leakage occurs within hours resulting in corrosive burns and destruction of the nasal septum and inferior turbinate. Corroded mucosa should be irrigated with normal saline and inflamed mucosa treated with Naseptin cream®.
Late presentation of a nasal foreign body
Occasionally, a small foreign body may lie unnoticed in the nose for many years. Such retained foreign bodies may eventually present with unilateral nasal congestion, epistaxis, discharge and occasionally with sinusitis in late adulthood. Nasal secretions, calcium and magnesium carbonates, and phosphates usually deposit around the foreign body forming a nasal concretion or rhinolith (Figure 22.1), which is demonstrable on CT scan as it is radio-opaque. A rhinolith must be extracted under a general anaesthesia to ensure complete removal and controlled irrigation of the nose.
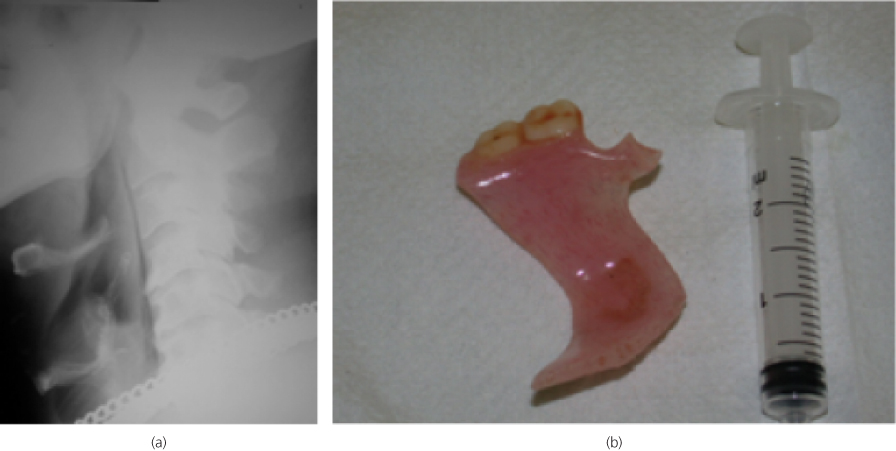
Orohypopharyngeal foreign bodies
Patients with orohypopharyngeal foreign bodies are usually adults, presenting acutely with pain and drooling. There is often a lateralising pricking sensation and significant odynophagia (pain on swallowing). Pharyngeal foreign bodies are commonly small bones which are not always radio-opaque. Fish bones may lodge in the tonsils, tongue base, valleculae or piriform fossae. Visualisation requires a good light, laryngeal mirror or a flexible nasendoscope. If no foreign body is visible and the patient is well and swallowing, with normal radiography, symptoms may be due to pharyngeal abrasion. The patient should be re-examined after 48 hours and if still symptomatic, should have a CT scan performed to look for a foreign body or signs of an abscess formation. Swallowed or inhaled dentures (especially partial) present special difficulties because their size and configuration compounds impaction and makes removal challenging. The presence of metallic material, such as a metal clasp, on the denture will render it radio-opaque on a plain film radiograph (soft tissue lateral neck is the film of choice) (Figure 22.2). However, most dentures are made from a radiolucent plastic (polymethylmethacrylate) and therefore can be missed easily on such a radiograph. This may delay diagnosis and subsequently lead to life threatening obstruction of aerodigestive tract or erosion of blood vessels. A CT scan would be the investigation of choice if the radiograph appears normal.
Figure 22.2 (a) Soft tissue lateral radiograph showing a partial denture foreign body (arrow); (b) retrieved partial denture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



