(1)
Narayana Hridayalaya Multispeciality, Bangalore, India
The flap reconstruction is an integral part of head–neck cancer surgery. The reconstruction has evolved greatly in the last few decades and that has enabled oncosurgeons to resect more advanced and complex tumors. The PMMC flap has been used as a mainstay of reconstruction for decades. The microvascular reconstruction has evolved lately and is becoming the standard of care for head and neck reconstruction. The algorithm for reconstruction of various subsites is already discussed in individual chapters. This chapter essentially focuses on flap raising technique, and only those flaps that are used frequently in our practice are described.
The following flaps are described in this chapter:
1.
Pectralis major myocutaneous flap
2.
Temporalis flap
3.
Infrahyoid flap
4.
Forehead flap
5.
Anterolateral thigh flap
6.
Fibula flap
7.
Rectus abdominis flap
8.
Radial forearm flap
The Pectoralis Major Myocutaneous Flap
This flap has been the mainstay for head–neck reconstruction for a very long time and continues to be an important component even today. It is very simple to raise and is a very safe flap. It is based on pectoral branch of thoraio-acromial artery.
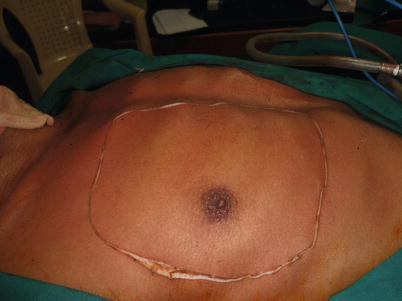



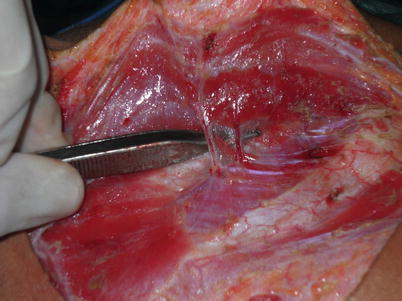

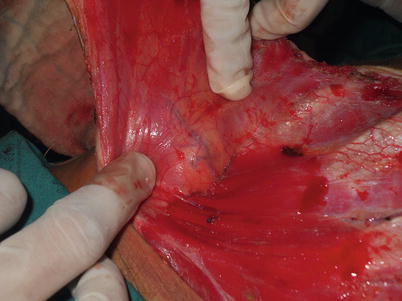

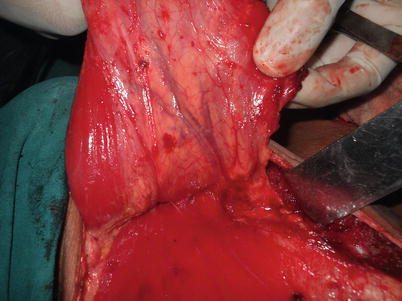

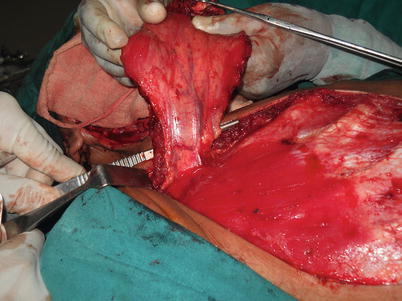




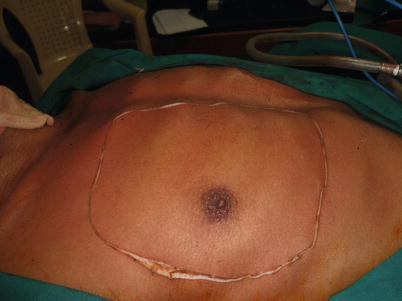
Fig. 16.1
The surface marking for large skin paddle. This is the area from where one can take skin paddle of varying sizes. The area below and medial to the nipple is preferred for small- to medium-sized defects. This donor site needs skin grafting but majority of other defects can be closed primarily. One needs to be extra careful while raising the flap in female and try to preserve as much breast tissue as possible while taking sufficient care not to harm the blood supply to skin paddle

Fig. 16.2
Identifying the lateral border of pectoralis major muscle is the first step in this procedure. This gives complete orientation about further dissection

Fig. 16.3
The flap is raised separate from pectoralis minor muscle

Fig. 16.4
The small perforator vessels are seen at deep surface of the muscle
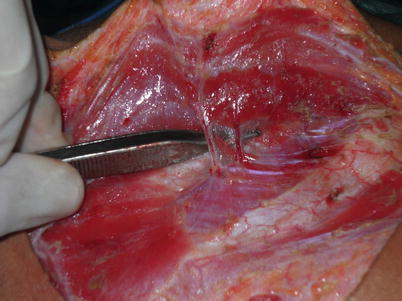
Fig. 16.5
It is important to secure these perforators to avoid postoperative hematoma

Fig. 16.6
The muscle is raised separate from the rib and pectoralis minor muscle. Try and leave periosteum over the rib for better graft uptake
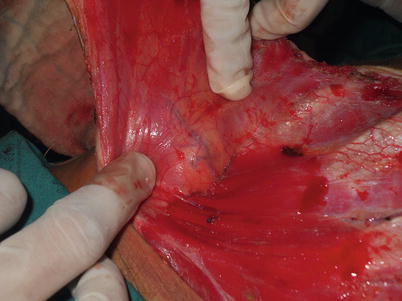
Fig. 16.7
The pedicle is seen as flap is raised further. Be careful in preserving the deep fascia over pedicle to avoid accidental injury. Further dissection is always carried with pedicle in view

Fig. 16.8
The skin flap above is raised to tunnel the flap into the neck
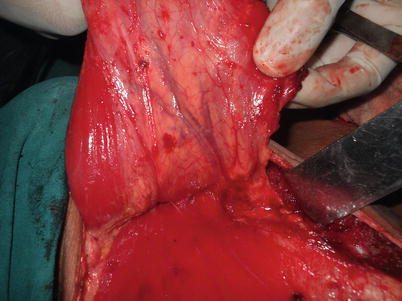
Fig. 16.9
The flap is completely raised. One can reduce the base of the flap to bare minimum. This increases the reach and allows one to rotate the flap without any pressure on the pedicle

Fig. 16.10
The lateral muscle fibers are divided to increase the reach of the flap
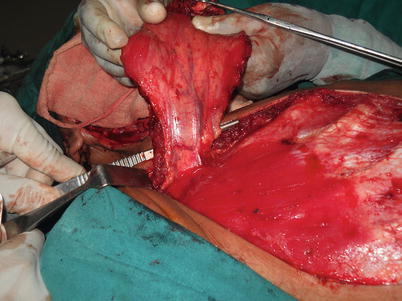
Fig. 16.11
The flap is completely raised. The base is kept bare minimum just to support the pedicle

Fig. 16.12
The tunnel is complete and adequate in size. One must make the tunnel large enough for safe and tension free passage of the muscle. When there is any doubt regarding the tension over the pedicle, one has to promptly increase the size of the tunnel or put releasing incisions over the skin

Fig. 16.13
The flap has been tunneled into the neck. It is important to avoid any twist of the pedicle particularly when the skin is required for defect of the neck. Most of the flaps are lost due to venous congestion because of the twist or pressure over the pedicle and every attempt should be made to avoid these problems

Fig. 16.14
The flap has covered the defect with ease and is tension free one must remove neck extension before raising the flap. One can remove the neck extension to increase the reach while suturing the flap. The PMMC can reconstruct majority of defects of the oral cavity and larynx–pharynx. This flap is very versatile and can be used as muscle only or large bi-paddle myocutaneous flap

Figs. 16.15 and 16.16
The cosmetic outcome is quite acceptable in majority of patients with proper flap orientation
Possibilities for PMMC Flap Reconstruction
Buccal mucosa–alveolus reconstruction: lining or for bi-paddled reconstruction
Tongue–FOM reconstruction: for hemiglossectomy, total and extended glossectomy as a single flap or in combination with other flaps
Oropharynx reconstruction: muscle only for small defects and composite flap for complex defects
Larynx–pharynx reconstruction: as patch or tube reconstruction after laryngectomy and pharyngectomy. For salvage laryngectomy
Neck–parotid reconstruction: for large skin cover after composite resection involving the skin
Salvage surgery: reconstruction of choice for majority of salvage surgery
Resource constrained setup: reconstruction of choice for majority of defects
Limitations
Reach not enough for maxilla and skull base defects
Difficult to cover defects above the zygoma
Flaps drags down in some cases due to its weight
Temporalis Muscle Flap
The temporalis flap is a simple and safe flap for reconstruction of maxillary defects.


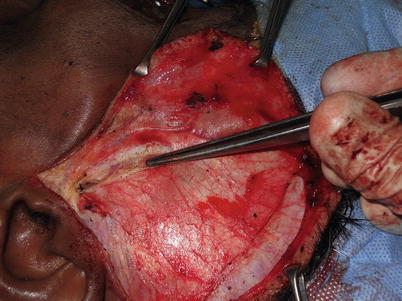


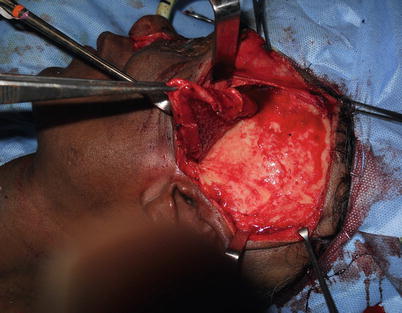
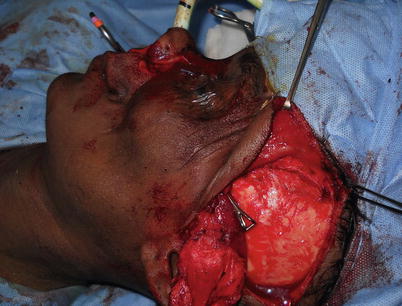
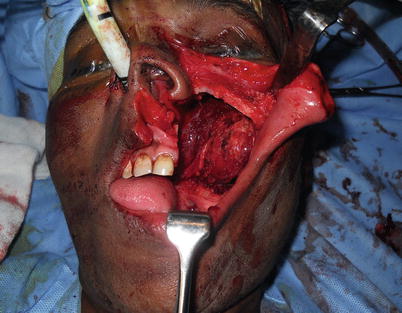


Fig. 16.17
The skin is marked to raise the flap

Fig. 16.18
The skin flap is raised over temporalis fascia. Care is taken not to go too anterior to avoid injury to the facial nerve
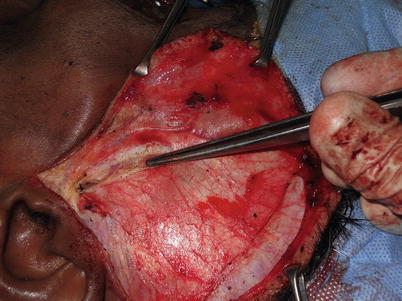
Fig. 16.19
The superficial layer of temporalis fascia is divided and fat plane is exposed for anterior dissection. This process automatically prevents injury to frontal branch of facial nerve as it runs above the superficial layer of temporalis fascia

Fig. 16.20
The zygoma is exposed and temporalis muscle is freed from below

Fig. 16.21
The muscle is separated from the skull. It is important to include more muscle in the posterior part and also to include the fascia beyond muscle to increase its reach. It is advisable to use periosteum elevator instead of cautery to avoid injury to deep branches of maxillary artery particularly in the lower half
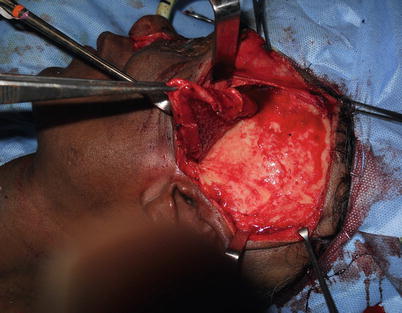
Fig. 16.22
The muscle is freed all around
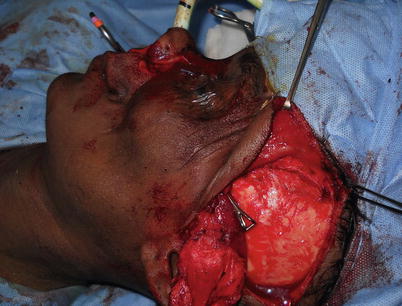
Fig. 16.23
The forceps is tunneled below the zygoma to bring the muscle into the maxillary cavity. This flap is useful when upper alveolus with maxillary tuberosity is removed. There is adequate space for flap rotation without any struggle and tension in such situation
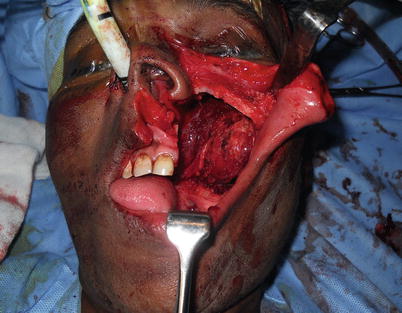
Fig. 16.24
The flap is in the cavity and can be sutured to complete the procedure. It is important to secure the medial insertion over the palate. We prefer to have holes in the palate and use nonabsorbable sutures in this region to have added strength. We also avoid placing suture on the buccal aspect to avoid tension on palatal aspect

Fig. 16.25
The photograph shows healed-healthy flap in few days
Possibilities for Temporalis Reconstruction
Infrastructure maxillectomy defects
Orbital floor reconstruction with temporalis and coronoid process
Lateral skull base defects
Orbit reconstruction
Limitations
Patients develop trismus in postoperative period after oral cavity reconstruction.
Cosmetic dip over the temple can be profound in some cases.
Infrahyoid Flap
This is a local flap that we use quite often to reconstruct small defects of the oral cavity. We prefer this flap over submental and nasolabial flap because of its better oncological safety over submental flap and better cosmesis over nasolabial flap. This flap is reliable if care is taken not to damage the venous drainage.
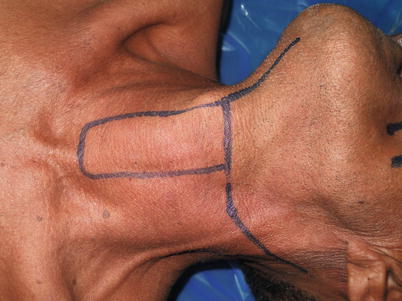



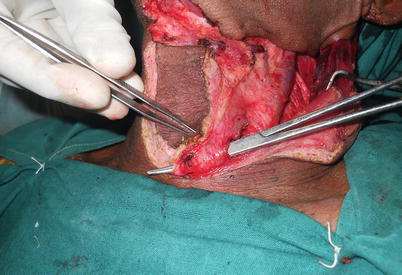




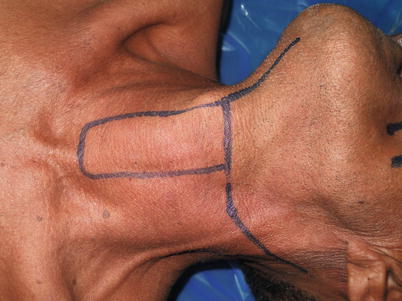
Fig. 16.26
The flap is marked over the neck. The skin width can be about 3–4 cm and the length can be from hyoid to clavicle. It is better for thin and long individuals compared to patients with short neck

Fig. 16.27
The neck dissection is complete. It is important to avoid dissecting the area medial to IJV near the superior thyroid veins

Fig. 16.28
The anterior jugular vein is ligated to expose the strap muscles

Fig. 16.29
The omohyoid muscle is divided to expose IJV
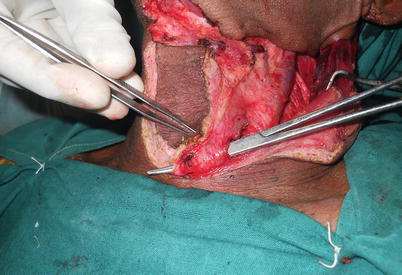
Fig. 16.30
The strap muscles are divided in the lower end
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


