CHAPTER 22 Facial Trauma
Soft Tissue Lacerations and Burns
Etiology
The most common causes of traumatic injuries to the face include motor vehicle accidents, interpersonal violence, activities of daily life, sports-related injuries, work-related injuries, and bites, both human and animal.1,2 Although generalized facial trauma, including bony trauma to the maxillofacial skeleton, is more common in men than women at approximately a 2 : 1 ratio, soft tissue facial trauma appears to have no distinct sex predilection and occurs in a wide range of ages, although the majority of injuries occur during the first 3 decades of life.3 Motor vehicle accidents are a common cause of facial injuries, affecting approximately 50% of survivors. The use of seatbelts alone, or in combination with airbags, has been shown to reduce the frequency and severity of facial injuries; however, airbags alone have not demonstrated the same benefit.4
Approach to Traumatic Injuries
History
The social context in which injuries take place is as important as the physical context. Injuries from interpersonal violence make up a large component of facial trauma. Assault and abuse victims may not volunteer the mechanism or the assailant without confidence that the health care system will protect them from immediate and future harm. Depending on their age and development, children may not be able to volunteer details of abuse, requiring a thorough history from parents or caregivers and witnesses in an effort to identify discrepancies. More than 50% of victims of child abuse demonstrate injuries to the face, although injuries to the face alone are not sufficient to suspect abuse.5 Abuse should be suspected when the described mechanism does not fit the injury pattern or when the child displays signs of abuse elsewhere.
Assurance of tetanus prophylaxis is imperative. Tetanus-prone wounds are typically deep lacerations, avulsions, or puncture wounds contaminated with soil, feces, saliva, or mineral debris. If the immunization status is unknown or if the patient has not completed the series of tetanus immunizations, tetanus immunoglobulin (TIG) and vaccine (tetanus toxoid) should be administered. All other patients who have completed a primary immunization series should receive toxoid unless they have had a booster or completed the series within the last 5 years.6
Physical Examination
Many soft tissue injuries to the face occur in the setting of underlying trauma to the maxillofacial skeleton, and a thorough examination must be performed with this in mind. Although the focus of this chapter is on injury to the soft tissues, an adequate evaluation of facial trauma includes an assessment to rule out fractures. A systematic approach is essential to prevent errors, both in diagnosis and management. Every practitioner caring for a trauma patient is obligated to follow ATLS protocol regardless of that caregiver’s role in treatment.7 An orderly approach using the ABCDE mnemonic with primary and secondary surveys assures that the most threatening conditions are dealt with first and that nothing is missed. A seemingly innocuous forehead laceration in the emergency department triaged quickly to the “facial trauma service” may mask occult intracranial or cervical spine injury depending on the mechanism—something that could be missed by simply focusing on fixing the laceration rather than treating the patient. Vigilance must be exercised in patients transferred from other institutions, and experienced surgeons recognize that an assessment from a transferring provider may not be an adequate substitute for their own careful examination.
The examination begins with careful investigation of problems with airway, breathing, and circulation—immediate or impending. Airway compromise is rarely associated with superficial soft tissue trauma alone; however, severe hemorrhage with collection of blood in the upper airway can rapidly compromise airway, breathing, and circulation, particularly in a combative or obtunded patient.8 The airway is secured by controlling hemorrhage with direct pressure or identification and ligation of the injured vessel. This must be performed with caution, however, to avoid injuring other important structures such as the facial nerve or parotid duct in attempts to quickly stop hemorrhage by clamping a bleeding vessel in the wound bed. Another injury requiring immediate intervention is that of corneal exposure from eyelid laceration or avulsion. Immediate corneal protection prevents potentially devastating ocular injury (Fig. 22-1).
Anesthesia
Complete assessment of wounds is often only possible after establishing adequate anesthesia. Additional patient discomfort during wound exploration and repair is unnecessary and creates an adverse environment for a technically successful repair. Comfortable working conditions for both the patient and the physician can generally be established with local anesthetics through topical application, infiltration, or nerve blocks of the trigeminal distribution. Lidocaine, with or without epinephrine in concentrations from 0.5% to 2%, is a commonly used agent for infiltration or regional block. Lidocaine is well tolerated by nearly all patients with minimal side effects and a safe dosing range.9 Widely quoted maximum doses for local anesthetics actually have little basis in human studies or evidence-based medicine and are largely extrapolated from animal data and case reports of toxicity.10 These theoretical guidelines suggest that toxicity from lidocaine, in the form of central nervous system disturbances (e.g., seizures or cardiac dysrhythmias), will develop with doses greater than 5 mg/kg of patient body weight or 7 mg/kg if epinephrine is added. Toxicity, however, is probably multifactorial, taking into account fluid status, age, site of injection, medical comorbidities, and other injuries.11 Even so, in the multiply injured patient requiring repair at separate sites by more than one practitioner, the aggregate dose of local anesthetic should be tracked and documented by all parties involved to avoid toxicity. In children, doses may be inadvertently high because of the patient’s smaller body mass.
Lidocaine alone has a modest vasodilatory effect on capillaries and can impair hemostasis during closure. The addition of epinephrine in a dilution of 1 : 100,000 to 200,000 encourages hemostasis and mitigates systemic absorption but requires caution in certain circumstances. Dense infiltration of macerated wound edges or long, tenuous flaps of avulsed skin with epinephrine may compromise otherwise salvageable tissue and should be avoided. The need for local infiltration can be markedly reduced or obviated by a well-performed regional block. Physicians involved in the treatment of soft tissue trauma should become facile with their use. Near-total anesthesia of the face for soft tissue work can be accomplished by selective blocks of the infraorbital, supraorbital/supratrochlear, zygomaticotemporal, zygomaticofacial, dorsal nasal, great auricular, and mental nerves.12 Appropriate use of these blocks decreases the overall dose of local anesthetic required and the pain associated with the injection of local agents. They are also helpful when infiltration of wound edges would distort important landmarks such as the vermillion border. Significantly, in a cooperative patient, establishment of good regional anesthesia may eliminate the need to perform a repair under general anesthesia in the operating room. Longer acting local agents such as bupivacaine may also be used for direct injection into the wound edge, or, more appropriately, for a long-acting block in select cases. Bupivacaine does have a narrower therapeutic window than lidocaine with potential for cardiotoxicity.13 Ropivacaine is another well-established long-acting local agent with a better dose-dependent toxicity profile than bupivacaine; however, higher cost may be a barrier to its use at many institutions.
The four chief causes of pain associated with injection are the temperature of the injectate, the acidity of the solution, the speed of injection, and the size of the needle. These factors are all easily addressed to minimize the discomfort of the patient. Warming the local agent to body temperature decreases the pain of injection.14 Similarly, buffering 1% lidocaine with 8.4% sodium bicarbonate solution in a ratio of 9 : 1 brings the pH of the solution up from 4 to a value around neutral. The only real tradeoff with buffering is the resultant diminished duration of effect, which can be as short as 30 minutes.9 Injecting slowly with small needles, 27 or preferably 30 gauge, also decreases pain. It is much easier to inject with a small needle when a small syringe is also used because there is a smaller discrepancy between the diameter of the syringe and the diameter of the needle. A calm, comforting demeanor, combined with appropriate technique, enables the surgeon to provide the patient with adequate anesthesia without any additional pain or anxiety. With children, it is best to take a graduated approach. Frequently, by the time the consultant is seeing the patient, the initial psychological trauma has abated and the child is fairly calm. One could first talk to the child about something other than the injury. Also, the clinician should explain everything he or she is going to do in advance. The patient’s anxiety only increases when awaiting a “surprise attack.” Next, the clinician should “examine” part of the patient’s body that was uninjured. This nonpainful touching can set the precedent that not everything is going to hurt. Next, the wound is gently examined. Gentle irrigation with warm saline is rarely painful and allows the wound to be cleaned and thoroughly examined. At this point, careful infiltration of local anesthesia with a small-bore needle is almost always possible. Most patients fall asleep during the wound closure. However, for some pediatric patients, the idea of the needle trumps all efforts to alleviate anxiety. Rather than restraining a child to anesthetize a wound through injection, the clinician should choose topical anesthesia or conscious sedation.
Topical anesthesia first gained popularity in the form of a solution of 0.5% tetracaine, 1 : 2000 adrenaline, and 11.8% cocaine, known as TAC anesthesia, after comparable efficacy and safety were demonstrated relative to injection with lidocaine.15–17 Based on the potential systemic toxicity and security concerns of the cocaine component of TAC, a variation on this technique, known as LAT (4% lidocaine, 1 : 2000 adrenaline, and 1% tetracaine), has been shown to be equally effective. It is also one-tenth the cost of TAC—a significant savings.18 Even though LAT and TAC have become agents of choice for anesthetizing simple lacerations in children and select adults, their role in more complex wounds has yet to be defined. In an uncomplicated laceration, it is relatively easy to uniformly administer a topical agent to all areas of the wound bed.19 Typically, an anesthetic solution is applied by saturated cotton tips or sponges and replaced every few minutes until anesthesia is obtained. This usually takes about 10 minutes. However, large, irregular wounds filled with clot or debris that would impair administration and require débridement are not candidates for this method. TAC should also be avoided near mucous membranes because of reports of systemic toxicity associated with high mucosal uptake of cocaine. It is important that adult patients understand that there is a possibility of testing positive for cocaine after TAC administration.20
Some children require sedation in addition to adequate local anesthesia. Conscious sedation or procedural sedation of children is a safe and effective way to diminish the potentially significant psychological distress associated with repair of soft tissue injuries.21 Administering sedation to children requires training, experience, skill, and appropriate institutional resources. In the emergency setting, this is best administered by trained nursing staff under the direction of a physician or other provider certified to perform procedural sedation in children. This allows the surgeon to focus on the patient’s injuries without the added responsibility of drug administration and monitoring. Despite its benefits, sedation does add to emergency department length of stay and cost of treatment, warranting judicious use when the child may tolerate repair with local anesthetic alone. This should not be used as an excuse, however, for withholding sedation for seemingly uncomplicated lacerations in children who are clearly distressed by the prospect of local anesthesia. Several agents have been demonstrated to be effective, including midazolam, ketamine, and fentanyl; these are often used in combination. The most common adverse effects are hypoxia and vomiting, which are usually minor and self-limited or resolve with minimal intervention.22
Cleaning
Carefully irrigating and cleaning wounds and surrounding skin is important not only for decreasing risk of infection but also to improve visualization of wound characteristics in preparation for repair. In the multiply injured, obtunded, or sedated patient, meticulous cleaning is even more important. It is not an uncommon scenario to encounter an unconscious patient in the trauma bay, positioned supine with an endotracheal tube and bite-block in the mouth, a nasogastric tube taped in place, a cervical collar around the neck, and dry, crusted blood, dirt, or debris concealing soft tissue injuries. With so many impediments to a thorough examination, cleaning the entire head and neck is critical to avoid missing injuries. This includes hair-bearing scalp and facial hair where many soft tissue injuries are easily hidden. Hair may need to be shaved or trimmed to adequately clean, assess, and repair injuries. Eyebrows may be trimmed conservatively or shaved if necessary, although it may take 6 months for them to fully regrow.23
In most cases, simple antimicrobial cleansers such as chlorhexidine are adequate. Saline alone does little to remove bloody crusts. Warm saline is slightly better. Warm saline with dilute peroxide is better still, although studies showing fibroblast and keratinocyte inhibition in vitro with peroxide and povidone-iodine have led to many authors voicing caution regarding their liberal use in open wounds.24 For most wounds, warm saline under moderate pressure will be adequate for irrigating debris and foreign material. Retained foreign bodies left unrecognized can develop into a significant problem and are a well-known cause of medicolegal action related to repair of traumatic injuries. Fortunately, the limited depth of soft tissue in the face relative to other areas of the body allows for most foreign material to be identified in the course of routine wound exploration.
Imaging is helpful in certain circumstances. Glass is a common foreign body associated with motor vehicle trauma and is easily detected with plain films. However, the utility of these studies is limited to wounds deeper than the immediate subcutaneous fat.25 Contrary to commonly held assumptions, a negative CT scan does not rule out a retained foreign body. The radiodensity of substances such as wood, plastic, and vegetative material are so low that imaging frequently misses them. Wood, however, is often visible on magnetic resonance imaging (MRI). There is an increasing body of literature in support of the use of ultrasound to detect the presence of radiolucent foreign bodies.26 Most foreign bodies in the head and neck, however, are discovered in the course of a detailed history, careful examination, and meticulous wound exploration. Loupe or microscope-assisted magnification is often helpful.27
This is most noticeable when debris is left embedded in dermis that has been denuded of epithelium. Judicious use of solvents such as acetone may even be necessary to help remove petroleum-based products. Time spent removing debris likely to cause permanent pigmentation will benefit both patient and physician in that delayed treatment of traumatic tattooing is difficult and often has disappointing results (Fig. 22-2).
Infection Control
There are no convincing data on the role of routine antibiotic administration for soft tissue injuries. Wounds treated within 8 hours and those created surgically are generally considered “clean,” indicating a presumed safety of primary closure. It is also generally accepted that in highly vascular areas such as the face, this margin of safety may be extended to 24 hours. Few data exist, however, regarding precise cutoff points to determine which wounds are too contaminated to safely close.28 The general principle of increasing bacterial counts as a function of time should be kept in mind. Even in wounds without a significant amount of exogenous bacteria, normal skin flora such as staphylococci and streptococci and mixed flora in wounds involving mucosa will proliferate. Heavily contaminated, partially devitalized, extensive, or deep wounds with oral contamination may benefit from at least a single dose of broad-spectrum antibiotics. Even animal bite injuries of the face may be adequately treated without routine antibiotic prophylaxis.29 Human bites are notoriously contaminated with various aerobic and anaerobic bacteria and recent studies support the use of antibiotic prophylaxis with broad-spectrum agents.30
Repair
The first step to performing a technically successful repair is preparation of the work environment. Excellent lighting, comfortable positioning for both the patient and physician, appropriate instruments for soft tissue work in the face, available support staff, and adequate anesthesia are all essential. The absence of any of these elements compromises the primary focus of the surgeon. If necessary, the patient may be transferred to an appropriate venue for repair such as the operating room or minor procedure room. Facial soft tissue work demands instrumentation such as fine tooth forceps, small needle holders, skin hooks, tissue scissors, suture scissors, and a scalpel handle with replaceable No. 15 and 11 blades (Fig. 22-3).
Loupe magnification is also often helpful in improving the precision of repair.
Epithelial closure is commonly performed with permanent monofilament sutures such as 6-0 or 7-0 nylon or polypropylene (Prolene). Absorbable suture with minimal tissue reactivity, such as fast absorbing gut, is also useful, especially in children or patients in whom suture removal may be difficult.31 A child who requires sedation for repair is unlikely to tolerate removal of permanent sutures. Similarly, adult patients who are unwilling, unable, or unlikely to follow up for suture removal are better served with absorbable sutures than permanent sutures left in too long or removed by inexperienced hands.
Tissue adhesives now have a proven role in wound closure with acceptable results compared to suture techniques in simple lacerations.32 Even though caution is appropriate in entirely sealing off a heavily contaminated wound such as a human or animal bite, there is no evidence that routine lacerations appropriately cleaned and irrigated have increased rates of infection with tissue adhesive than with suture. They can even be combined with fast absorbing gut on skin, preventing premature suture removal. There are limitations, however. Octyl cyanoacrylate combined with a subcutaneous 4-0 Vicryl closure has approximately the same tensile strength of percutaneous 5-0 nylon suture and cannot be relied upon to close a wound on tension without some widening of the scar.33 For tissue adhesives to be used effectively, epithelial edges must sit in good approximation before application to prevent glue from entering the wound, resulting in a wider scar or even wound breakdown.34 Eversion of the wound edges is more difficult with adhesives.
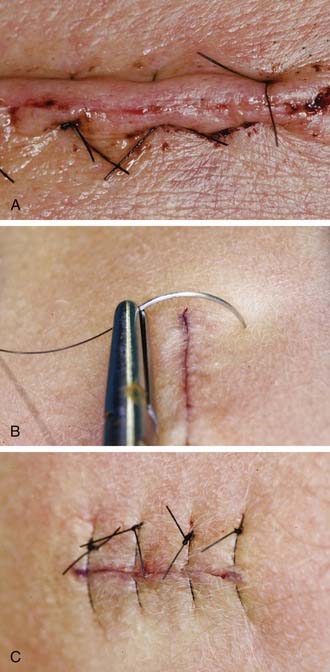
Eversion is critical to the favorable appearance of the final result. Because scars contract as they heal, a laceration that is flat when reapproximated will become inverted. An inverted scar, unless coincidentally located in a wrinkle, will create an obvious shadow and be easily noticed. The best technique for everting the edges of a wound is to use vertical mattress sutures. Properly placed, these sutures elevate the incision just enough to counteract scar contracture. The distal pass of the needle should be placed perpendicular to the surface of the skin and should be placed one half the chord-length of the needle from the incision. The chord-length is the distance from the tip of the needle to the swage. The proximal pass of the needle should only include enough of the epidermis to align the edges and reapproximate them. It is a common technical error to place the distal pass too close to the laceration and the proximal pass too far away. This has several negative effects. First, there is very little skin supporting the suture and, as the wound swells, the tension causes the suture to act as a seton, creating suture tracks. The second is that the epidermal edges will not be in apposition, which results in a gap that granulates and reepithelializes, creating a red, shiny scar (Fig. 22-4).
Types of Injuries
Abrasions
Abrasions are defined as a superficial soft tissue wound caused by contact with a hard, irregular surface, resulting in skin loss not extending to the subcutaneous layer. In the multiply injured patient, these wounds are often neglected and can ultimately result in significant color and contour irregularities. Even with appropriate initial treatment consisting of meticulous cleaning, débriding devitalized tissue, dirt, or debris, these wounds require ongoing care for optimal healing. Once clean, a moist environment conducive to reepithelialization can be achieved with a variety of media including antibiotic ointment, hydrogel, or hydrocolloid dressings.35 Because these wounds tend to weep and collect fibrinous debris, especially in the setting of increased interstitial fluid, ongoing gentle cleaning is essential. This allows a maximum degree of epithelialization with a minimum degree of fibrosis and scar. Pigmentation abnormalities are nearly universal; however, significant changes are usually temporary and based partially on the depth of injury. Abrasions deep to the papillary dermis cause a greater degree of scarring than more superficial injuries. As with any other scar, protection from sun exposure decreases the likelihood of postinflammatory hyperpigmentation.