Exfoliation Syndrome, Pigment Dispersion Syndrome, and the Associated Glaucomas
Mahmoud A. Khaimi
Gregory L. Skuta
Rebecca K. Morgan
Exfoliation Syndrome and Exfoliative Glaucoma: History and Nomenclature
In 1917, Lindberg described grayish or bluish flakes of material on the pupillary border in a large proportion of patients with chronic glaucoma.1 Vogt later hypothesized that this material represented degenerative changes of the lens capsule followed by secondary desquamation and proposed the term senile exfoliation of the lens capsule. He also recognized its association with open-angle glaucoma, proposing the term capsular glaucoma.2 Busacca argued that the exfoliative material represented deposition of material formed elsewhere in the eye rather than degenerative changes of the lens capsule.3 Dvorak-Theobald subsequently showed that exfoliative material differed histochemically from lens capsule and, to differentiate this condition from true exfoliation of the lens capsule secondary to infrared exposure, suggested the term pseudoexfoliation of the lens capsule.4 Subsequent electron microscopic studies by Ashton et al. and Bertelsen et al. indicate that the anterior lens capsule was directly affected in this disorder.5,6 Bertelsen et al. suggested that preequatorial lens epithelial cells produced the abnormal fibrillar substance and recommended the term fibrillopathia epitheliocapsularis.6 Eagle et al., who believe that the material represented abnormal basement membrane secretions, have called this condition basement membrane exfoliation syndrome.7
The terms exfoliation syndrome (XFS) and pseudoexfoliation syndrome are now most commonly used to designate this disorder and are used interchangeably in current literature. However, because recent ultrastructural studies indicate that the material on the lens capsule is derived, at least in part, from the lens, it is proposed that the disorder be called exfoliation syndrome.8,9,10
Epidemiology
Although XFS has been well described in patients of Scandinavian heritage, it also has been documented in numerous populations, including other Europeans,11 the Japanese,12 Australian aborigines,13 Navaho Indians,14 individuals of Mediterranean origin,15 natives of India16 and Pakistan,17 and the southern Bantu tribe of South Africa.18 It may be observed, but is relatively rare, among African Americans.19,20
Wide variations in the prevalence of XFS have been reported. These variations may result, at least in part, from differences in the definition of disease, populations studied, age and sex distributions, racial and ethnic factors, and examination techniques.11,21 In one study of 2,958 patients older than 60 years of age examined by a single investigator in three countries, Aasved reported a respective prevalence rate of exfoliation of 4.0% in England, 4.7% in Germany, and 6.3% in Norway.11 Among Australian aborigines older than 60 years of age, Taylor et al. noted a 16.3% prevalence rate of exfoliative changes.13 In the United States, a prevalence rate of 1.6% among patients older than 30 years of age and 3.2% for those older than 60 years of age was described in one study.22 In another, the prevalence rate was 0.7% for those aged 52 to 64, 2.6% for ages 65 to 74, and 5.0% for ages 75 to 85.21
The reported prevalence of increased intraocular pressures and glaucoma in XFS is variable, again depending on the populations evaluated. Kozart and Yanoff reported that of 100 consecutive patients in Philadelphia with XFS, glaucoma was present in 7% and ocular hypertension (intraocular pressure above 22 mm Hg without optic nerve cupping or visual field loss) was present in 15%.23 According to Henry et al., the cumulative probability of elevated intraocular pressures developing in XFS eyes previously with normal intraocular pressures was 5.3% over 5 years and 15.4% over 10 years.24 Hensen and Sellevold noted that glaucoma may develop in 7% to 20% of XFS eyes previously without glaucoma over 5 years and 9% to 24% of these eyes over 10 years.25 The lower figures referred to progression in women and the higher figures to progression in men. These investigators further noted that in bilateral XFS and unilateral glaucoma, the second eye developed glaucoma within 5 years in 21% to 26% of cases.
Among patients with open-angle glaucoma, the prevalence rate of XFS varies widely with the geographic location. In the United States, reported figures range from 1% to 12%.9,20,23,26 A prevalence rate of 26% to 75% has been noted in various Scandinavian countries.27,28,29 Figures from other areas include a 46.9% prevalence rate in eastern Turkey,30 44.5% in northwestern Spain,31 and 1.4% in a South African white population.32
XFS is predominantly a disorder of the elderly and affects both men and women. Although it has been described in patients as young as 17 years of age,33 it is rare among those younger than 40 years. The reported mean age of onset of this condition ranges from the late sixties to seventies, and the prevalence increases with increasing age.21,34 Although some studies show that exfoliation is more common among men,16,35 several large American and European series indicate that exfoliative changes without glaucoma are more common in women.18,19,34 However, among patients with exfoliative changes, the likelihood of the development of increased intraocular pressures and glaucoma appears to be greater in men.36,37,38
Genetic factors and differential genetic expressions currently are being investigated in order to better understand any hereditary patterns associated with XFS.39 It appears that XFS may be inherited as an autosomal dominant trait with late onset and incomplete penetrance.40 However, most cases of XFS do not appear to follow any clear Mendelian inheritance patterns.40,41,42 Preliminary linkage analysis has identified three gene loci, 2p16, 2q35-36, and 3q13-q21.40 Recently, genome-wide association studies on homogenous Icelandic and Swedish populations have associated XFS to three single nucleotide polymorphisms (SNPs) on chromosome 15q24.1.42a More specifically, Thorleifsson et al discovered a strong association between XFS and two nonsynonymous SNPs (rs1048661, R141L; rs3825942, G153D) in the lysl oxidase-like protein 1 gene (LOXL1). Furthermore, this association was confirmed when cohorts from other populations were analyzed.42b The LOXL1 gene is a member of the lysly oxidase gene family, which plays important roles in the biogenesis of connective tissue and elastogenesis. Aberrancies in the LOXL1 gene may contribute to the production of defective elastin and accumulation of fibrillar material in eyes with XFS. However, as many patients with the LOXL1 risk alleles do not manifest exfoliation, ongoing study of these associations and their implications will be vital to understanding the complex genetic basis of XFS.
An epidemiologic study by Ringvold et al. revealed a higher than expected prevalence of XFS among both spouses of married couples, which suggests an environmental influence on the distribution of the disorder.43 However, in a more recent epidemiologic study, no relevant impact of climate on the occurrence of XFS was found.44 Ringvold et al. also considered an infectious etiology, such as a slow virus, in the pathogenesis of XFS.10,43 Additionally, Küchle and Naumann reported the occurrence of exfoliation in three eyes of two young patients 4 to 6 years after penetrating keratoplasty, which raises the possibility that XFS is a transmissible disease (from donor buttons to recipients).45
Clinical Features
Lens
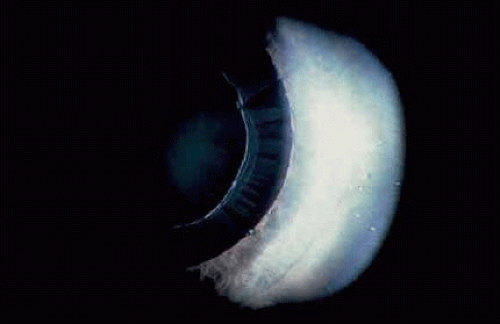
Deposition of exfoliative material on the anterior lens surface is the most commonly recognized feature of XFS and usually is best appreciated after pupillary dilation.46 A bull’s eye pattern is generally seen in which a translucent central zone and a granular peripheral zone of deposition are separated by an intermediate clear zone (Fig. 1). The translucent central zone of exfoliative material varies in diameter and may exhibit curled edges. In approximately 20% of patients with exfoliation, the central zone may be absent.38 The intermediate clear zone presumably results from lens contact with movement of the iris. The granular peripheral zone, which may be subtle but invariably is present in XFS, generally exhibits a well-delineated inner border and often shows numerous radial striations (Fig. 2). Occasionally, a bridge of exfoliative material may cross the clear zone to join the central zone and the granular peripheral zone.38,47
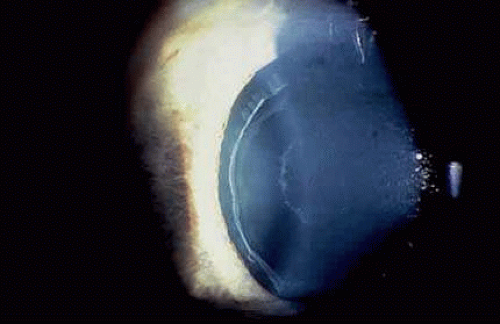 FIGURE 1. Typical bull’s eye pattern of exfoliation on lens surface showing separation of central and peripheral zones of deposition by intermediate clear zone. |
Some patients with XFS exhibit phacodonesis and subluxation of the lens, apparently resulting from degenerative changes in the zonular fibers.48,49,50 (Fig. 3) Spontaneous dislocation of the lens into the vitreous has been reported.51 In 1970, Bartholomew described 22 spontaneously displaced lenses in 19 patients with the disorder.48 Sixteen of the lenses were subluxated inferiorly. In these eyes, he visualized superior zonular fibers that were coated with exfoliative material and further noted that the zonular breaks generally were present at the ciliary body attachments and not at the lens, which led him to hypothesize that the main degenerative process occurred at the insertion of the zonular fibers to the basement membrane of the ciliary body epithelium. By electron microscopic examination, Schlötzer-Schrehardt and Naumann noted disruption of zonular fiber structure at the ciliary body insertion sites in eyes with XFS, but also observed abnormalities at the attachments to the anterior lens capsule.49
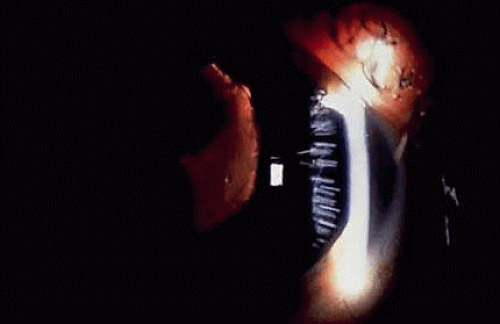 FIGURE 3. Subluxated lens in an eye with XFS. (Courtesy of Dr. Ronald Gross, Cullen Eye Institute, Houston, TX) |
Bartholomew also described phacodonesis in XFS and believed that this represented a probable sign of incipient lens displacement.52 Upon electron microscopic studies, Futa and Furuyoshi demonstrated marked degenerative changes in the lens zonules of XFS eyes with phacodonesis compared with normal zonular structure in those with no phacodonesis.50 Clinically, iridodonesis in association with phacodonesis may not necessarily be observed because of iris rigidity as a consequence of infiltration by exfoliative material or, perhaps, prolonged miotic therapy.48
Iris and Pupil
Second to the lens deposition described earlier, exfoliative material is most prominent at the pupillary border (Fig. 4) and should suggest the diagnosis of exfoliation even before the pupil is dilated.27 In addition, defects of the pigmented pupillary ruff are commonly seen. Aasved reported pupillary defects in 6.1% of eyes without XFS and in 74% of eyes with XFS.53 He further noted that in patients with unilateral XFS, pupillary ruff defects were twice as common in the affected eyes when compared with the fellow eyes. Iris transillumination defects in a moth-eaten pattern often are observed. Although these generally are limited to the region of the sphincter (Fig. 5), some patients also have diffuse midperipheral defects.54 Of additional note, exfoliative material has been demonstrated on the posterior surface of the iris by light and scanning electron microscopy.55
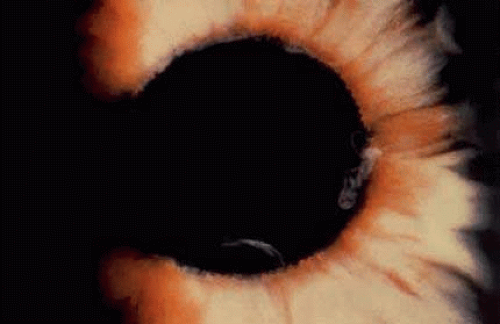 FIGURE 4. Accumulation of white exfoliative material at pupillary border. (Van Buskirk EM: Clinical Atlas of Glaucoma. Philadelphia: WB Saunders, 53, 1986) |
Iris fluorescein angiographic studies in eyes with exfoliation disclose iris hypoperfusion, fewer radial iris vessels, and loss of the normal pattern of these vessels.56 Microneovascularization of the iris and associated fluorescein leakage also have been observed.57 These findings may result from tissue hypoxia caused by abnormal extracellular matrix formation or vascular abnormalities.58,59 Whether tissue hypoperfusion contributes to the development of these abnormalities or is a secondary effect of the XFS is not known. In support of the former are studies that show an increased frequency of XFS in eyes of patients with a history of transient ischemic attacks60,61 and an increased prevalence in patients with a history of vascular disease.62 Nauman et al. observed that spontaneous intrastromal iris hemorrhages without iris neovascularization occur more commonly after mydriasis and suggest advanced iris vascular damage.55
The iris hypoxia in this disorder may lead to atrophy of the iris pigment epithelium, which results in particulate pigment deposition on the anterior iris surface seen in some eyes with exfoliation.59 Prince and Ritch have noted that the pigment often is found in a whorl-like pattern on the sphincter and is most commonly found over the inferior portion of the sphincter, although it also may be diffusely scattered over the peripheral iris surface.46
Iris vasculopathy also has been noted to lead to the chronic breakdown of the blood–aqueous barrier, which manifests clinically as cell and flare and creates a “pseudouveitis” appearance.63 After cataract surgery, trabeculectomy, and laser trabeculoplasty exfoliative eyes have been found to demonstrate a greater inflammatory response than eyes without XFS, which is presumably secondary to blood–aqueous barrier dysfunction.64,65
Cornea
Slit-lamp examination of the cornea may reveal flakes or clumps of exfoliative material deposited on the endothelium46 (Fig. 6). Upon ultrastructural examination, Schlötzer-Schrehardt et al. noted incorporation of the material into Descemet’s membrane, which led them to believe that degenerated endothelial cells could be a source of the deposits.67 Pigment on the endothelium also may be observed. It usually is diffuse and unevenly distributed, but rarely forms a Krukenberg spindle. Decreased endothelial cell counts and morphologic abnormalities of endothelial cells in eyes with exfoliation, as well as uninvolved fellow eyes of apparent unilateral cases, also have been reported.68,69,70 These findings have led Schlötzer-Schrehardt and Naumann to differentiate XFS-associated keratopathy from Fuchs endothelial dystrophy. Mainly, they note that XFS keratopathy is characterized by a diffusely thickened Descemet’s membrane with irregular nonguttate-like excrescences with melanin deposited in and on the corneal endothelium. These eyes are at increased risk of early corneal decompensation as a result of moderate rises in IOP seen after mydriasis or minor intraoperative trauma.40
Conjunctiva
Clinically, the conjunctiva does not appear to be involved in XFS. However, conjunctival biopsy specimens reveal the presence of exfoliative material,71,72,73,74 and fluorescein angiographic studies show loss of the normal limbal vascular patterns, congestion of the anterior ciliary vessels, and possible evidence of neovascularzation.75
Angle and Anterior Chamber
XFS and pigment dispersion syndrome (PDS) are the two most common causes of increased pigmentation of the trabecular meshwork. The increased trabecular meshwork pigmentation in XFS tends to be less distinct and more patchy than the dense homogeneous deposition of trabecular pigment in PDS46 (Fig. 7). (It has been suggested that the degree of angle pigmentation in XFS is correlated with the severity of the glaucoma.26,76) However, Spaeth et al. more recently have noted that the degree of angle pigmentation in XFS may not be correlated with the severity of glaucomatous disc damage, which suggests that pigment dispersion is not the single decisive factor in chronic intraocular pressure elevation.9,77,122
Pigment also may be deposited on or anterior to Schwalbe’s line (Sampaolesi line). Occasionally, flakes of exfoliative material may be present in the anterior chamber angle (see Fig. 7). Although the anterior chamber angle usually is open in XFS, acute and chronic angle closure and occludable angles may be seen.9,76,77,78,79
Pupillary dilation in XFS may result in marked pigment dispersion into the anterior chamber. This may be accompanied by a substantial increase in the intraocular pressure46 that presumably results from decreased aqueous outflow caused by the dispersed pigment. Although pigment dispersion after dilation may occur in patients without XFS, Krause et al. have shown that the pigment released after dilation is substantially greater in XFS than in normal persons.80
The dispersed iris pigment on the anterior iris surface, in the angle, and in the anterior chamber after dilation arises from the iris pigment epithelium.81 As mentioned previously, iris hypoxia may result in pigment epithelial atrophy and subsequent pigment dispersion,59 but iris contact with a rough anterior lens surface also contributes to this phenomenon.
Ciliary Body and Zonules
Exfoliative material also may be seen on the ciliary processes and zonules (Fig. 8). Using a modified method of gonioscopy known as cycloscopy, Mizuno and Muroi documented exfoliative material on the zonules and ciliary processes in all 31 eyes with clinical evidence of exfoliation.12 They further noted that in patients with clinically unilateral exfoliation, more than half (17 of 31) of the fellow eyes demonstrated exfoliative material on the ciliary processes and zonules, thus establishing subclinical evidence of exfoliation in clinically “uninvolved” eyes.
Histopathology
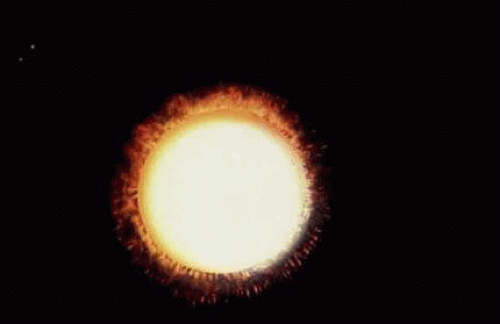
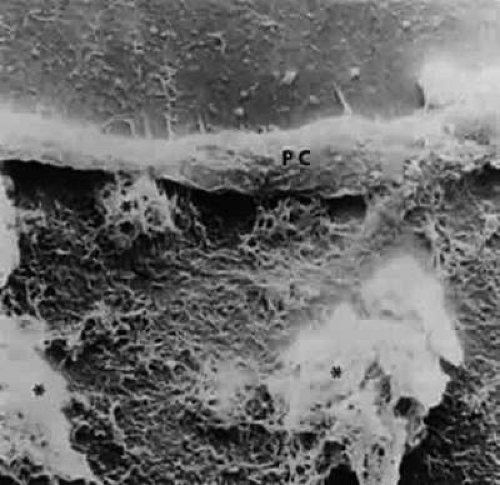
Accumulation of exfoliative material may be detected histopathologically throughout the anterior segment to include the lens, iris, trabecular structures, conjunctiva, ciliary body, and zonules. The deposition of fibrillar eosinophilic material on the anterior lens capsule is the classic histopathologic feature of XFS (Fig. 9). Ultrastructural studies also have indicated some degree of actual exfoliative changes or peeling of the anterior lens capsule82 (Figs. 10 and 11). In addition, Ashton et al. described a degenerative band containing exfoliative material within the inner half of the lens capsule.5 Bertelsen et al. independently noted projection of coarse fibrils from the lens surface into the deep portion of the lens capsule to form an amorphous layer of the lens capsule between the lens epithelium and normal lens capsule.6 Thus, studies indicate that exfoliative material accumulates on the anterior lens surface but also that the lens capsule itself may be involved, and that the underlying epithelial layer may at least partially contribute to the production of the exfoliative material.
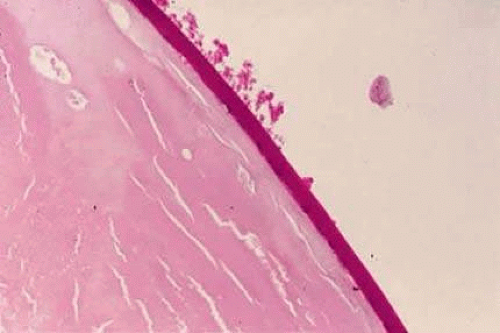 FIGURE 9. Deposition of fibrillar eosinophilic material on anterior lens capsule in XFS (PAS, 250×). (Courtesy of Dr. Marilyn C. Kincaid and Armed Forces Institute of Pathology, Washington, DC) |
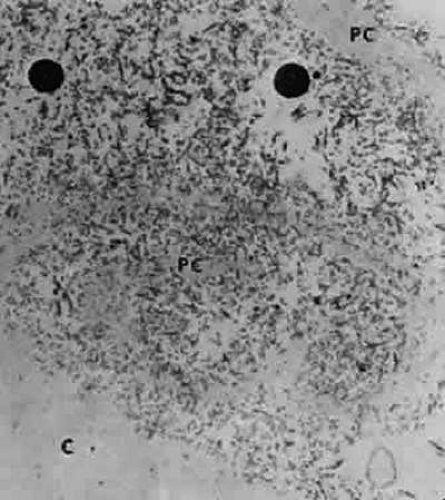
A ground glass-appearing precapsular layer sometimes is observed on the anterior lens capsule of elderly patients. Ultrastructural studies show this layer to have a fibrillar structure similar to exfoliative material, which indicates that this may be a precursor to the XFS.83,84
Exfoliative material also may be observed histopathologically on the pupillary border,8 on the anterior iris surface,85 within the anterior iris stroma, around iris blood vessels,86,87,88 and on the posterior surface of the iris.3,4 The iris has been implicated as a source of the material,81,89 and essentially all iris cell types, including epithelial cells, fibrocytes, melanocytes, vascular endothelial cells, pericytes, and smooth muscle cells, may be involved in the production of exfoliative material.59 Exfoliative deposits also have been described on the zonules and ciliary processes (Fig. 12) and within the basement membrane of the nonpigmented ciliary epithelium.4,90 Observations by Mizuno and Muroi have suggested that exfoliative material may accumulate on these structures before deposition elsewhere in the eye.12
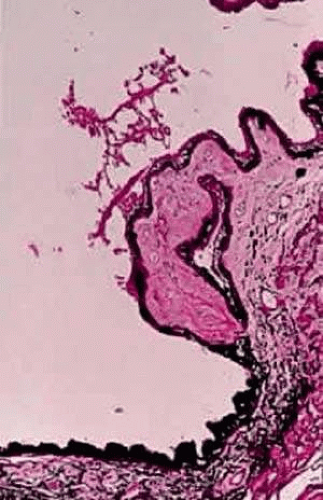 FIGURE 12. Light micrograph of exfoliative material overlying ciliary body process (PAS, 100×). (Courtesy of Dr. Marilyn C. Kincaid and Armed Forces Institute of Pathology, Washington, DC) |
Exfoliative material and pigment have been described in the intertrabecular spaces, trabecular endothelium, juxtacanalicular tissue, and Schlemm’s canal.3,4,8,91,92,93 An association between the extent of trabecular involvement by exfoliative material and intraocular pressure has been noted with greater involvement producing higher intraocular pressures.94 Although most exfoliative material is carried to the trabeculum by aqueous, the material also may be produced by the trabecular endothelial cells.95,96
Exfoliative material generally is not found in the vitreous or posterior to the hyaloid face. However, it has been described on the hyaloid face after intracapsular cataract extraction.47,97
Exfoliative material also may be seen in extrabulbar tissues. As previously noted, exfoliative fibers have been seen in biopsy specimens of conjunctival tissue from eyes with XFS and also from fellow eyes that appeared to be clinically unaffected.71,72 Eagle and colleagues described similar material in the walls of the short posterior ciliary arteries in the orbit.7 These authors suggested that exfoliative material is an abnormal basement membrane synthesized at multiple sites by aging cells. Histopathologic studies also have revealed the material in orbital septa, extraocular muscles, vortex veins, and central retinal vessels.73,74
In 1992, Schlötzer-Schrehardt et al.,98 followed by Streeten et al.,99 reported electron microscopic findings of exfoliative fibers in more remote extraocular tissues. They demonstrated the material in lung, heart, liver, gallbladder, skin, kidney, and cerebral meninges of exfoliative patients. It was observed to be within the interstitial fibrovascular connective tissue in close proximity to elastic fibers, collagen fibers, fibroblasts, and vessel walls. This suggests that XFS is a systemic disorder involving generalized abnormal connective tissue metabolism. As noted previously, exfoliation may have an increased prevalence among individuals with systemic vascular conditions.60,61,62 However, no systemic clinical manifestations resulting from the presence of extraocular exfoliative material have been demonstrated.
Nature of Exfoliative Material
Exfoliative material consists of an irregular meshwork of fibers composed of fibrillar subunits.82,100 Masses of these fibers correspond to the material seen clinically (see Fig. 10). The individual fibrils, which measure 6 to 8 nm in diameter and exhibit cross-banding at 10- to 12-nm intervals, are hypothesized to consist of macromolecules with a protein backbone and polysaccharide side chains.101,102,103 In contrast to collagen, the amino acid content of exfoliative material lacks hydroxyproline.104 Ringvold and Husby noted histochemical, immunologic, and ultrastructural features that led them to classify exfoliative material as an amyloid-like substance.105 Repo et al. described Congo red-positive staining for amyloid in the vessel walls of 7 of 13 iris specimens from exfoliation patients and believe that these findings support the theory that XFS is associated with amyloid.66 Immunohistochemical studies by other investigators have shown heparin sulfate and chondroitin sulfate proteoglycans, laminin, entactin/nidogen, fibronectin, and amyloid P protein to be components of exfoliation material.106,107 Schlötzer-Schrehardt et al. have suggested that the material may be an expression of a disordered extracellular matrix synthesis.106
As previously noted, Eagle et al. regarded exfoliative material as abnormal basement membrane material.7 In support of this assumption, other studies have indicated that it may be a basement membrane proteoglycan.106,108 Streeten et al. reported that, like zonular fibers, exfoliative material demonstrated staining characteristics similar to oxytalan, the microfibrillar component of elastic fibers.109 These investigators also have shown an immunologic relation to elastic microfibrils and elastin.103,110 The association of exfoliative material with elastosis in conjunctival biopsy specimens from XFS patients offers some support for the hypothesis that exfoliation represents a type of elastosis.111 In this elastosis, basement membrane-secreting cells appear to produce an abnormal protein-mucosubstance complex with elastic microfibrillar characteristics. Recent discoveries regarding the LOXL1 gene appear to support the concept of defective elastogenesis.
Differential Diagnosis
PDS and true exfoliation of the lens capsule are included in the differential diagnosis of XFS. In contrast to the elderly population affected by XFS, PDS and, more specifically, pigmentary glaucoma tend to occur bilaterally in the eyes of young myopic patients.104 Peripheral radial iris transillumination defects are seen rather than the peripupillary atrophy of XFS. In addition, Krukenberg spindle generally is seen in pigmentary glaucoma, and the trabecular pigmentation in pigmentary glaucoma tends to be more dense and homogeneous than the patchy trabecular hyperpigmentation in XFS. The characteristic appearance of exfoliative material on the anterior lens capsule is not present in pigmentary glaucoma. However, XFS may occur in patients with PDS.113
In true exfoliation of the lens capsule secondary to intense heat,114 inflammation,115 trauma,115,116 or irradiation,115 the lens capsule is rolled up in characteristic clear, thin sheets. This condition, which also may be called capsular delamination,117 is only infrequently associated with glaucoma. Histopathologically, a prominent split in the anterior lens capsule is seen without associated deposition of exfoliative material.
Laterality
Clinically evident exfoliative changes initially are unilateral in a large percentage of patients with XFS, although these changes frequently become bilateral over time. In their series of 100 consecutive patients, Kozart and Yanoff described 76 patients with unilateral pseudoexfoliation and 24 with bilateral changes.23 In patients who initially presented with unilateral exfoliation, Hansen and Sellevold noted the development of exfoliation in the fellow eyes in 31% of women and 40% of men over 5 years.25 Aasved described similar progression in 43% of patients over 6 to 7 years.118 Henry et al. reported a 5-year probability of 17% for developing XFS in the fellow eyes of initially unilateral patients.24 Patients with unilateral exfoliation tend to be younger than patients with bilateral exfoliation.37,38,47
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree