7
Evaluating Blunt Temporal Bone Trauma
Temporal bone trauma is commonly seen, with motor vehicle accidents, industrial accidents, and physical altercations representing 18 to 75% of patients with head injuries.1,2,3 Injuries resulting from such an insult can be far ranging and debilitating or even life threatening. Diagnosis may be obvious, but often the injuries are subtle. For those patients suffering from complications arising from blunt temporal bone trauma, the magnitude of the impact must be substantial, requiring 1875 lb of force to produce a fracture of the temporal bone.4
The clinician must be cognizant that blunt trauma introduced to the skull can affect not only the temporal bone but also structures within it, including the facial nerve, the middle ear, and the inner ear. Furthermore, because the temporal bone comprises the lateral skull base, cranial nerves V–XII and the great vessels of the neck must also be considered. These injuries fall into the realm of the otolaryngologist.
Often, findings related to insults to the temporal bone are overlooked in favor of other more obvious injuries. In addition, the symptoms of injuries stemming from temporal bone trauma can be protean, requiring a high level of clinical suspicion. Thus the otolaryngologist plays a vital role in the evaluation of the head injury patient. This chapter reviews the presentation, evaluation, and treatment of the patient suffering from an acute injury to the temporal bone.
■ Classification of Temporal Bone Fractures
Temporal bone fractures have traditionally been segregated into longitudinal versus transverse fractures, with longitudinal fractures representing 70 to 90%.5,6,7 Longitudinal fractures occur as a result of lateral impact on the temporal bone. The fracture line is described as paralleling the axis of the petrous bone, arising first at the squamous portion, involving the roof of the external auditory canal and tegmen tympani, coursing around the dense bone of the otic capsule, and involving either the carotid canal or jugular foramen (Fig. 7–1A,B). It is also often described as an otic capsule – sparing fracture. When associated with facial nerve dysfunction, facial paresis or paralysis is oftendelayed in onset occurring secondary to nerve edema, but one must not discount the possibility of a bone spicule wounding the facial nerve. Secondary to the axis of fracture, a conductive hearing loss resulting from ossicular discontinuity is also common. Uncommonly, a sensorineural hearing loss can result from a concussive injury to the cochlea.8 This is most commonly a high-frequency loss that resembles a noise-induced hearing loss configuration.
By contrast, transverse fractures are reported to constitute 20 to 30% of temporal fractures.5,6,7 The axis of the fracture line classically extends from the foramen magnum, traverses the petrous pyramid, and ends near the foramen lacerum anteriorly (Fig. 7–2A,B).As predicted by the axis of the fracture, the direction of the trauma is most often posterior to anterior, with the point of impact at the occiput. Because the force necessary to produce a transverse fracture is severe, other injuries are often present. The fracture line often traverses the internal auditory canal, and immediate facial nerve paralysis is seen in 50% of cases 9 resulting from a transection injury. Likewise, the cochlear and vestibular nerves as well as the otic capsule are immediately at risk, with total sensorineural hearing loss and vertigo commonly resulting.
■ Presentation and Evaluation
The otolaryngologist is often consulted for injuries related to temporal bone trauma in a delayed manner. More pressing injuries, such as those relating to the abdomen or the cerebrum, may have been evaluated and treated first. In other circumstances, the otolaryn-gologist is part of the acute cranial injury team involved in the initial evaluation of the head trauma patient. Regardless of the time of initial evaluation, one must decipher the magnitude of force received by the skull, the striking object, the direction of the force, any loss of consciousness, initial facial nerve function following the injury, and the status of the other cranial nerves. Any preexistent conditions must also be elucidated.
In the acute setting, matters of the airway, breathing, circulation, and cervical spine must first be addressed as well as other life-threatening circumstances. A neurosurgical evaluation is mandatory. Initial otolaryngological evaluation should include a full cranial nerve and complete otolaryngological examination. Attention should be given to any other areas of fracture within the craniofacial skeleton, including the squamous portion of the temporal bone. An ear examination should note the presence of any external auditory canal bony defects, tympanic membrane perforation, hemotympanum, or clear drainage arising from either the middle ear or the external auditory canal itself. Special attention should be given to the status of the facial nerve. Furthermore, the presence and direction of nystagmus should be determined because this would indicate vestibular injury. An evaluation of gait, when possible, is valuable. The determination of pure-tone thresholds is also necessary but can be obtained when the patient is stable. If an audiogram in a sound booth is not possible, at least a bedside audiogram is recommended. The results should be confirmed with a tuning fork exam. Diagnostic testing must include high-resolution computed tomography (CT) of the temporal bone in thin cuts in the axial plane. Coronal cuts are also preferred. If indicated, CT with the addition of contrast, magnetic resonance imaging (MRI), or angiography (MRA) may be obtained, especially if there is concern regarding injury to the brain parenchyma or vascular structures. Table 7–1 displays the most common sequelae following temporal bone injuries, and Table 7–2 considers the management of these conditions that can accompany temporal bone fractures. Subsequent examination should ascertain the presence or absence of these conditions.
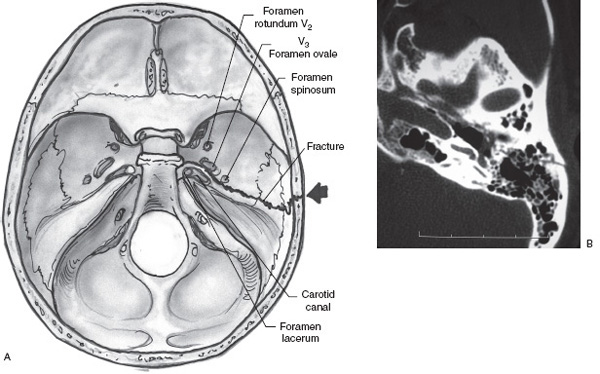
FIGURE 7–1 (A) An axial cut of temporal bone showing a longitudinal fracture.(B) Computed tomography in a patient with a longitudinal temporal bone fracture, with the fracture line traveling anterior to the cochlea.
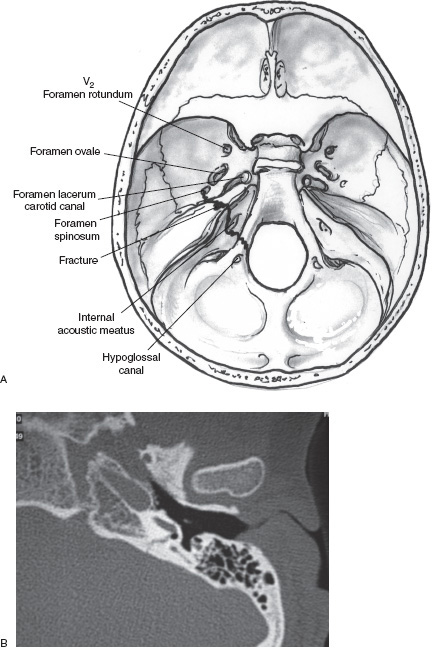
FIGURE 7–2 (A) An axial cut of temporal bone showing a transverse fracture. (B) Computed tomography in a patient with transverse temporal bone fracture, with the fracture line involving the cochlea.
Cerebrospinal Fluid Leak
The otolaryngologist must maintain a high level of suspicion for any leakage of cerebrospinal fluid (CSF) from either the external ear or the eustachian tube. As previously reported, 15 to 58% of temporal bone fractures are associated with a CSF leak manifesting either as clear otorrhea or clear rhinorrhea.10,11,12 It can manifest immediately following the traumatic event or in a delayed manner, once mucosal edema around the eustachian tube or middle ear has abated. This leak results either from a dural tear at the middle or posterior fossa surface or through an otic capsule fracture. When a tympanic membrane perforation is present or there is a fracture and dural tear along the superior portion of the external auditory canal, egress of clear fluid through the external auditory canal is observed. By contrast, when the fracture and dural tear occur medial to an intact tympanic membrane, egress of CSF through the eustachian tube to the nasopharynx manifested as rhinorrhea is observed.
Sequelae of Temporal Bone Fractures | Percentage Occurrence |
|---|---|
Hearing loss10 | 82.0 |
Vertigo30 | 24.0 |
Cerebrospinal fistula | 14.9 |
Facial nerve paralysis | 7.0 |
Meningitis | 1.6 |
(Data from Brodie H, Thompson T. Management of complications from 820 temporal bone fractures. Am J Otol 1997;18:188–97.)
Initial otolaryngological examination should include an otologic exam. The external auditory canal is often filled with blood, clots, and debris. Cleaning within the external auditory canal must be done in a careful and sterile manner. Extensive suctioning should be avoided. Any clear fluid in the external auditory canal should be evaluated either for the presence of B2 transferrin, if adequate volume permits, or for glucose levels, utilizing a urine dipstick. A glucometer used to measure finger-stick glucose levels can also be used. The presence of either or both B2 transferrin and glucose levels approximating those of the serum should be interpreted as being consistent with CSF. To elucidate the source of the CSF leak, a high-resolution temporal bone CT can be helpful to delineate areas of tegmen tympani or tegmen mastoideum dehiscence. A CT cisternogram or nuclear studies are rarely necessary.
Problem | Prevention/Treatment |
|---|---|
Cerebrospinal fluid leak | Maintain high level of suspicion Assess for aural and nasal discharge Collect fluid with B2 transferrin or glucose level assessment Once diagnosed, treat conservatively with bed rest and head of bed elevation Consider lumbar drain if it does not cease after 4–5 days Consider surgical closure if it does not cease after 4–5 days with lumbar drain |
Facial nerve paresis | Determine facial nerve status immediately following injury With partial function, observe as satisfactory outcome is likely |
Facial nerve paralysis | Determine facial nerve status immediately following injury Computed tomography (CT) to determine fracture line and its relationship to the course of the facial nerve If transection of facial nerve likely, consider immediate surgical exploration for repair Obtain electroneuronography (ENoG) to assess level of facial nerve degeneration Following 14 days, obtain electromyograms (EMGs) to assess for any signs of regenerating fibers If no signs of recovery in one ENoG and consecutive EMGs over several weeks, consider surgical decompression of the facial nerve Surgical decompression must always include the meatal foramen at the lateral internal auditory canal, the narrowest portion of the bony covered facial nerve |
Vertigo | Observe patient in regard to the presence of nystagmus and its direction Determine based on nystagmus its likelihood of being an insult to the peripheral end-organ or central vestibular system |
Perilymphatic fistula | Assess for exacerbation of vertigo with position and Valsalva maneuver Assess for association of balance symptoms with a stepwise, fluctuating hearing loss Consider electrocochleography, which would show an elevated summating potential/action potential ratio Consider CT of temporal bone to assess for a pneumolabyrinth Conservative therapy warranted initially with bed rest Continued vertigo and deterioration of hearing warrants surgical exploration and repair |
Labyrinthine concussion | Nonfluctuating patients with mild vertigo versus imbalance Conservative observation with possible vestibular therapy |
Vestibular nerve injury | Accompanies facial nerve injury Observe with consideration of transtympanic gentamicin versus vestibular nerve section if symptoms persist beyond 1 year |
Delayed endolymphatic hydrops | Conservative medical management initially Surgical intervention when recalcitrant |
Benign paroxysmal positional vertigo | Canalith repositioning maneuver Brandt-Daroff exercises Posterior semicircular canal occlusion |
Hearing loss | |
Conductive hearing loss |



