Enucleation, Evisceration, and Exenteration Techniques
Mark Alford*
*The author has no financial interest in any of the products discussed in this manuscript.
The removal of an eye or the orbital contents is one of the most serious and difficult decisions a patient and physician must consider. The patient facing the loss of an eye has often recently been through multiple ophthalmic surgeries, experienced severe ocular trauma, or been diagnosed with a potentially life-threatening disease. Patients facing the removal of an eye are often feeling depressed and overwhelmed.
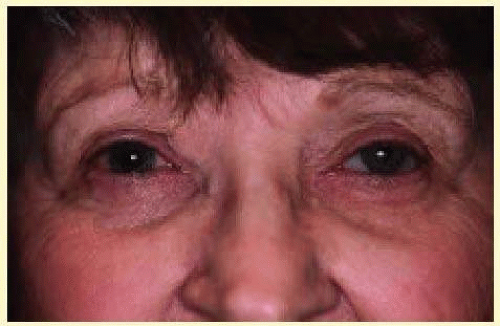
Enucleation is removal of the entire globe, including the cornea, sclera, and a portion of the optic nerve (Fig. 82.1). Evisceration surgery involves removal of the contents of the globe while leaving the sclera and optic nerve in place. The cornea can be retained in some evisceration cases. Exenteration is the removal of the globe, as well as the complete or partial removal of the soft tissues of the orbit. The ultimate goals of these surgeries are to safely and effectively remove the diseased eye or orbital contents using advanced surgical techniques, eliminate the severe underlying ocular pathology, and provide excellent long-term cosmesis. In addition to the surgical procedure, the ophthalmologist often must coordinate the patient’s ancillary care such as radiation therapy, systemic workup, and prosthetic evaluations. Although every surgeon who performs enucleations, eviscerations, or exenterations must provide emotional support to the patients, certain patients will need psychologic referrals and contact with support groups.
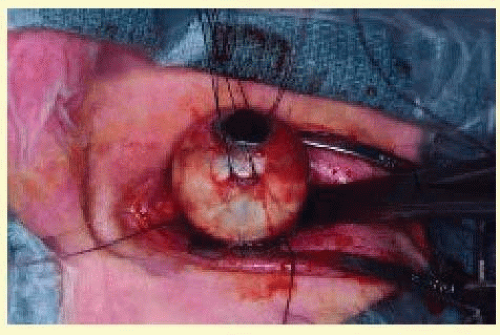 FIG. 82.1 The globe is removed from the socket using silk traction sutures. The optic nerve is clamped with a large hemostat. |
The objective of this chapter is to provide the reader with a general understanding of underlying principles and surgical techniques to manage this challenging group of patients. The indications and contraindications for enucleation, evisceration, and exenteration are discussed. Surgical techniques and an explanation of the various implant materials are reviewed. The chapter also provides guidance in managing the anophthalmic patient postoperatively.
HISTORICAL PERSPECTIVE
Dating back thousands of years, there is evidence that the Egyptians and Sumerians were making artificial eyes and performing enucleations. It was not until the 1500s that enucleations were reported in the medical literature. Noyes1 first reported evisceration of the ocular contents in 1874. In 1885, Mules2 was the first physician to report the use of an orbital implant, a glass sphere, after an evisceration. Advances in surgical techniques, anesthesia, implant materials, and prosthetics over the past decade have greatly improved surgical outcomes and patient satisfaction. In addition, the ability to deal with the long-term complications of the anophthalmic socket such as enophthalmos, ptosis, contraction, exposure, extrusion, and lower lid laxity have improved significantly. Today, most patients can confidently return to their daily activities with good cosmetic results following the removal of an eye.
ALTERNATIVES TO REMOVAL OF THE EYE
Not all blind, painful disfigured globes require removal. In many cases, patients are relieved to try an alternative treatment to surgery while adjusting to the loss of vision. The use of topical steroids, cycloplegics, antiglaucoma medications, and oral analgesics can provide relief for varying periods. The use of retrobulbar alcohol injections has been used in the past in selected patients. It has been my experience that alcohol injections are painful, provide temporary relief, and make future enucleation surgery more difficult because of the postinjection scarring of the orbit. In a debilitated patient that is a very poor surgical risk, it is a reasonable choice for temporary pain control. The only permanent solution is removal of the eye, which is often safer and more effective than alternative treatments.
Patients with blind, disfigured eyes without pain can be managed effectively with a custom made, shell conformer (Figs. 82.2 and 82.3). Conformers provide excellent cosmesis and good motility for many patients. A custom fit by a skilled ocularist is essential for a good appearance and comfort. Corneal sensitivity and globe phthisis may limit the patient’s ability to tolerate the shell or for the ocularist to create a cosmetically acceptable appearance. Although the appearance is improved with a shell conformer, the eye must continue to be followed for problems. Because the risk of uveal melanomas in phthisical eye is reported to be as high as 12%, routine ocular ultrasound should be performed in atrophic eyes.3
The likelihood of sympathetic ophthalmia should also be discussed with any patient deciding against removal and electing to keep a traumatized or phthisical eye. Sympathetic ophthalmia is a rare, bilateral granulomatous panuveitis that occurs after injury to one eye. The exact incidence is unknown, but reports have shown it to be as common as 0.28% to 1.9% following penetrating trauma.4 The incidence is less following intraocular surgery. The cause of sympathetic ophthalmia is unknown, but evidence suggests sympathetic ophthalmia represents an autoimmune inflammatory response to retinal melanocytes mediated by T-cells.5,6 It is believed that enucleation within 2 weeks of the initial injury prevents the onset of sympathetic ophthalmia. Treatment consists of systemic anti-inflammatory agents including corticosteroids and immunomodulators. The role of enucleation after the diagnosis of sympathetic ophthalmia remains controversial.7,8
Enucleation during childhood has been reported to cause orbital growth retardation.9 Promoting bony growth remains a challenge to the oculoplastic surgeon. Traditional treatments include progressive conformers, orbital implant exchange, orbital expanders, dermis fat grafts, and craniofacial surgery. However, Fountain and coworkers10 have shown that children who undergo enucleation leading to acquired anophthalmia at an early age maintain normal orbital and periorbital soft tissue growth when large static spherical implants are placed at the time of surgery. Implant exchange and enlarging conformers were not found to be necessary.
ENUCLEATION AND EVISCERATION
Indications for Enucleation
Recommending enucleation is one of the most difficult therapeutic decisions in ophthalmic surgery. The most common indications for enucleation are treatment of intraocular malignancies, relief of pain in blind eyes; removal of severely traumatized, deformed, or phthisical eyes without visual potential; and prevention of sympathetic ophthalmia.
Choroidal melanoma is the most common primary intraocular malignancy in adults. Treatment of choroidal melanoma must be individualized to each patient on the basis of tumor size, tumor location, metastatic spread, and patient preference. For many years, enucleation was the definitive treatment for intraocular melanomas. Over the past 36 years, an increasing proportion of patients have been treated with radiation alone with a decreasing number of patients treated with radioactive plaque therapy and enucleation. Despite changing trends in treatment, the 5-year survival rate of approximately 81.6% has remained unchanged.11 The Collaborative Ocular Melanoma Study (COMS) has investigated the role of enucleation versus I-125 radioactive plaque therapy in medium-sized tumors and found similar survival rates. The COMS12 also studied enucleation alone versus pre-enucleation external beam radiation in eyes with large melanomas, finding no difference in outcomes.
The Zimmerman theory postulated that enucleation might induce metastatic spread of the disease because of an increase in the intraocular pressure during surgery. This theory was based on the findings in 1,146 patients with uveal melanomas that metastatic disease was found in only 1% of patients preoperatively but increased to 8% during the second year of follow-up.13 From information obtained in the COMS, there is evidence that enucleation does not induce metastasis. Although this topic remains controversial, most surgeons advocate gentle handling of the tissues, as well as avoidance of opening the globe during enucleation surgery to decrease the theoretical increased risk of tumor spread during enucleation surgery.
Retinoblastoma is the most common intraocular malignancy of children. Although other means of treatment exist such as chemotherapy, cryotherapy, radiation, and photocoagulation, most eyes affected by retinoblastoma are enucleated. Enucleation of the affected eye has resulted in survival rates as high as 90%.14
In a review of 24,444 enucleation cases over a 55-year period, Spraul and Grossniklaus15 found trauma to account for 40.9% of cases, whereas tumors were the cause of enucleation in 24.2% of cases. Brackup and colleagues16 found that 34% of patients with open globe injuries eventually required enucleation for pain control in a university referral practice. Custer17 reviewed 58 cases of enucleation for blind, painful eyes and found that 45% of patients had sustained prior trauma. In the same study, 202 cases of enucleation during a 15-year period were reviewed; intraocular malignancy accounted for 54% of cases, blind painful eyes accounted for 33%, and disfigured phthisical eyes for 6% of cases.17 Margo18 found that blind, painful eyes accounted for 43% of cases and was the most common indication for enucleation in a study of enucleations in a community hospital practice.
The issue of primary enucleation must sometimes be addressed by any ophthalmologist who cares for ocular trauma patients. In most cases, surgeons initially try to salvage even severely traumatized eyes. Assessment of visual acuity and obtaining proper informed consent may be impossible. There is also some advantage in allowing the patient and the patient’s family to realize that the eye is no longer functional and to come to terms emotionally with the loss of vision. Primary enucleation is appropriate in certain circumstances. In patients who have experienced explosive, thermal, or gunshot injuries to the eye, there is typically no appreciable ocular tissue left to repair and primary enucleation may be indicated. In other patients large corneoscleral lacerations extending posterior to the ora serrata where no light perception (NLP) vision is documented and prolapsed uveal and retinal tissue is verified by frozen section, primary enucleation is a viable option. Of course, complete examination to evaluate the status of the other eye should be completed before surgery and detailed informed consent by the patient or patient’s guardian must be obtained. They must be made well aware of the condition and realize that no chance of vision will be possible in the future and that the eye will be removed.
Typically associated with penetrating ocular trauma or surgery, sympathetic ophthalmia is a rare, granulomatous panuveitis affecting both the injured and the uninjured eye. Characteristically, there is a diffuse lymphocytic infiltration of the uveal tract with nonnecrotizing granulomas. The precise cause and incidence is unknown. Most studies quote incidence rates between 0.001% and 1.9% in traumatized eyes.19 Although the condition is rare, enucleation is the only known prophylaxis for sympathetic ophthalmia.19 Based on the previous information, enucleation has been recommended within 2 weeks of the injury to prevent sympathetic ophthalmia. However, current thoughts on the subject are under debate.
Levine and coworkers4 undertook a chart review and survey of the members of the American Society of Ophthalmic Plastic and Reconstructive Surgery, Uveitis Society, and Eastern Ophthalmic Pathology Society in an effort to evaluate the relationship between evisceration and sympathetic ophthalmia. First, of the 51 patients who underwent evisceration at their institution, none was found to have clinical evidence of sympathetic ophthalmia. The survey portion of the study found no documented cases of sympathetic ophthalmia among the respondents following evisceration. Less than five cases of sympathetic ophthalmia were recalled but not documented by the surveyed physicians. From this information, the authors concluded that sympathetic ophthalmia is a rare disease and is infrequently associated with evisceration. Levine and coworkers concluded that evisceration is safe and effective procedure. It should be considered in cases in which direct examination or ultrasound excludes intraocular tumor, when there is adequate scleral volume, and when the pathologic specimen is not important.4
The Enucleation Procedure
The most devastating surgical complication in ophthalmology would be the removal of the incorrect eye. It is absolutely essential that the eye to be removed is appropriately identified before surgery. Reviewing the patient’s chart and obtaining informed consent personally are the first steps on the day of surgery. After the patient is asleep in the operating room, verifying the correct eye by another chart review, as well as direct examination of the patient, is essential. In patients with intraocular tumors in which the eye typically appears normal externally, a dilated examination is extremely helpful. I like to dilate only the operative eye and identify the tumor just before draping the patient. Marking the cornea of the operative eye with a surgical marking pen also provides another safety check. Finally, a shield should be placed over the nonoperative eye, and the patient should be prepped and draped by the operating surgeon. These measures, although time consuming, are important in preventing a disastrous situation.
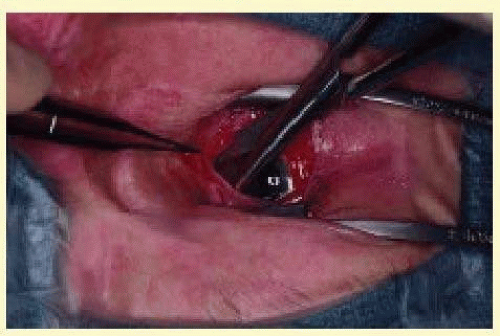
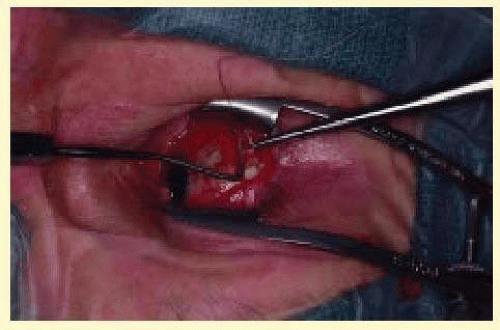
Enucleation is best performed under general anesthesia. After the patient is asleep and has been prepped and draped by the surgeon, a retrobulbar injection of 3 cc of a 50/50 mixture of 1% lidocaine and 0.5% bupivacaine with 1:100,000 units of epinephrine is performed. An eyelid speculum is placed, and a 360° limbal peritomy is performed with blunt-tipped Westcott scissors and small toothed forceps. Using blunt-tipped Steven’s tenotomy scissors, the four quadrants between the recti muscles are cleared (Fig. 82.4). This is performed by grasping the edge of conjunctiva and Tenon’s capsule, advancing the scissors posteriorly along the sclera to just past the equator, and spreading the tissue by opening the scissors. Next, all four recti muscles are identified, tagged with a double-armed 5-0 Vicryl suture in a locking fashion, and cut free from the globe. Each rectus muscle is identified and isolated on a muscle hook and excess facial attachments are bluntly removed from the muscle’s surface with a cotton-tipped swab. One end of a double-armed 5-0 Vicryl is then passed through the midportion of the muscle belly approximately 1 mm from its insertion toward the edge of the muscle (Fig. 82.5). The suture is then passed through the underside of the muscle approximately 1 mm from the muscle edge and pulled through so as to lock the suture. The other end of the suture is passed similarly by starting the pass where the first end started and exiting at the opposite muscle edge. The sutures are then clamped or taped to the drapes. After all four recti muscles have been removed from the globe, the superior oblique muscle tendon is cut with Westcott scissors. Next, the inferior oblique muscle is isolated with a muscle hook in the inferior medial quadrant, cauterized across its belly, and cut (Fig. 82.6). A 4-0 silk suture is then placed in a running fashion through the remaining muscle tissue of the medial and lateral recti muscles to be used as traction sutures. While applying gentle upward traction, a large hemostat is advanced toward the optic nerve, posterior to the globe, starting at the lateral canthus. With the hemostat closed, the optic nerve is identified. With the clamp superior to the nerve, gentle inferior movement of the clamp will cause the eye to rotate superiorly. The opposite will be observed with the hemostat inferior to the nerve. With the position of the optic nerve accurately identified, the clamp is opened, retracted slightly, advanced over the nerve, displaced a few millimeters posteriorly, and closed. Again, gentle movement of the clamp should verify that the nerve is securely clamped. With the nerve still clamped, enucleation scissors are then advanced into the orbit, anterior to the clamp, and the optic nerve is transected (Fig. 82.7). The globe is elevated with the traction sutures while any remaining tissue adherent to the globe is cut with scissors. The socket is immediately packed with two gauze sponges. During this time the orbital implant can be wrapped with an appropriate wrapping material and prepared for implantation. The globe is grossly examined and sent to the pathology laboratory for examination. The packing is removed, the cut edge of the optic nerve is isolated, and bipolar cautery is applied. The clamp is carefully released under direct visualization to ensure that no significant hemorrhage is present. The socket is then examined for any sign of pathologic process. A small rent in posterior Tenon’s capsule corresponding to the opening for the optic nerve can be repaired at this time using a single 5-0 Vicryl suture. Repair of this defect in Tenon’s capsule prevents unintentional posterior migration of the orbital implant.
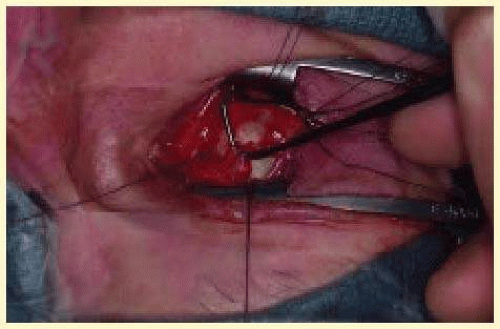 FIG. 82.6 The inferior oblique muscle is isolated on a muscle hook before cauterization and transection. |
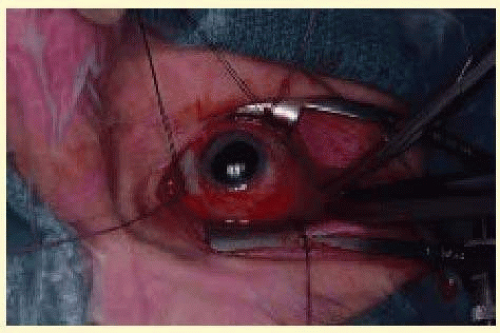 FIG. 82.7 After the optic nerve is clamped, curved enucleation scissors are used to cut the optic nerve just anterior to the clamp. |
In certain instances, it is appropriate to place the implant posterior to Tenon’s capsule, directly into the orbital fat. In these cases, placing blunt-tipped scissors into the defect and spreading easily enlarges the rent in posterior Tenon’s capsule allowing for placement of the implant directly into the muscle cone.
To provide for the best possible prosthetic appearance and motility, an implant with attached extraocular muscles should be placed within Tenon’s capsule. The largest implant that comfortably fits into the socket should be used to decrease the risk of a superior sulcus deformity. Most adults can accommodate a 20- or 22-mm implant without difficulty. Wrapping an implant provides approximately an additional 2 mm of diameter. (The average ocular diameter is 24 mm.) In general, the recti muscles are attached to the implant directly or to the various materials used to wrap orbital implants in a location slightly anterior to their normal anatomic position. When using a wrapped implant, cut four windows in the sclera measuring 2 by 5 mm corresponding to the positions of the extraocular muscle attachments. Each extraocular muscle is then advanced through its respective window and sutured to the sclera and implant (Fig. 82.8).
 FIG. 82.8 A scleral-wrapped orbital implant. Windows to allow for attachment of the extraocular muscles are visible. |
A complete discussion on the wide variety of orbital implants and wrapping materials is found in the section on implant and wrapping materials. A careful layered closure is mandatory to decrease the risk of implant exposure. Tenon’s capsule is closed first with multiple interrupted 5-0 Vicryl sutures. Care should be taken not to incorporate any conjunctiva into the deep closure. This may allow for cyst formation, implant exposure, or extrusion. The conjunctiva is then closed with a running suture of 7-0 Vicryl (Fig. 82.9). Antibiotic ointment and a conformer are then placed between the eyelids, and the socket is pressure patched for 4 to 7 days. Some surgeons place patients on prophylactic oral antibiotics for the first few days following surgery. After the patch is removed, the patient is asked to apply antibiotic ointment to the socket twice a day for the next 2 to 4 weeks. Continued wear of the conformer is used to prevent shortening of the conjunctival fornices. Consider placing a temporary suture tarsorrhaphy to prevent loss of the conformer. The tarsorrhaphy can be kept in place for up to 3 weeks. The patient is ready to see the ocularist 6 to 8 weeks after surgery for the prosthesis fitting. Patients should be encouraged to wear polycarbonate glasses to protect the remaining eye.
Indications for Evisceration
Evisceration is the removal of the ocular contents while leaving the sclera and optic nerve and, in some cases, the cornea intact. Evisceration offers several advantages over enucleation. Operating time is shorter, the operation is less technically challenging, and the procedure can be performed under retrobulbar anesthesia. There is less disruption to the orbital tissues, better motility, and a more cosmetically acceptable orbit when compared with enucleation. It is the preferred treatment for endophthalmitis because it allows for extirpation and drainage of the ocular contents without orbital invasion. In cases of endophthalmitis, orbital implantation has typically taken place as a secondary procedure. However, a recent study has found that primary implant placement is a viable technique.20 Evidence suggests that eviscerated eyes have better implant motility and few complications.21 Disadvantages include the theoretical risk of sympathetic ophthalmia and a less complete specimen for pathologic examination to detect intraocular malignancy or spread. Although controversy exists about the exact indications for evisceration and enucleation, evisceration should never be performed in cases of suspected intraocular tumor.
The Evisceration Procedure
The appropriate eye for removal must be established as described previously. Unlike enucleation, evisceration can be performed using a retrobulbar injection and intravenous sedation. Whether monitored anesthesia or general anesthesia is used, a retrobulbar injection of 3 cc of a 50/50 mixture of 1% lidocaine and 0.5% bupivacaine with 1:100,000 units of epinephrine is injected to control oozing and provide postoperative pain control. The patient is then prepped and draped by the surgeon. An eyelid speculum is placed and a 360° limbal peritomy is performed with blunt-tipped Westcott scissors and small toothed forceps. Using Steven’s scissors, the four quadrants between the recti muscles are cleared. This is performed by grasping the edge of conjunctiva and Tenon’s capsule, advancing the scissors posteriorly along the sclera to just past the equator and spreading the tissue by opening the scissors.
Approximately 1 to 2 mm posterior to the limbus, a small full-thickness scleral incision is made. Westcott scissors is then used to make a circumferential incision around the globe to remove the cornea. If the cornea is to be left in place, the incision is stopped just short of completion leaving a small scleral hinge. The intraocular contents are then separated from the sclera using an evisceration spoon or Freer periosteal elevator. Bleeding from the optic nerve or penetrating vessels can be controlled with gentle bipolar cautery. The pigment is meticulously removed using absolute alcohol on a cotton-tipped applicator. The scleral cavity is then copiously irrigated with antibiotic solution. Windows oriented in an anterior to posterior direction are cut in the sclera in the four quadrants between the recti muscles using scissors. The sclera can also be opened around the optic nerve.22 These scleral windows allow for vascular ingrowth if a porous implant is placed. Scissors are then used to make two cuts at the anterior opening of the sclera in an inferior-medial and superior-lateral direction to facilitate implant placement into the sclera. A sphere implant measuring from 14 to 18 mm is placed into the scleral cavity (Fig. 82.10). Redundant sclera is trimmed and the sclera is closed with multiple interrupted 5-0 braided nylon sutures. Tenon’s capsule is closed first with multiple interrupted 5-0 Vicryl sutures. The conjunctiva is then closed with a running suture of 7-0 Vicryl (Fig. 82.11). Antibiotic ointment and a conformer are then placed between the eyelids, and the socket is pressure patched for 4 to 7 days. Some surgeons place patients on prophylactic oral antibiotics for the first few days following surgery. After the patch is removed, the patient is asked to apply antibiotic ointment to the socket twice a day for the next 2 to 4 weeks. Continued wear of the conformer is essential to prevent shortening of the conjunctival fornices. The patient is ready to see the ocularist 6 to 8 weeks after surgery for the prosthesis fitting. As with any monocular patient, polycarbonate glasses should be worn routinely to protect the remaining eye.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree