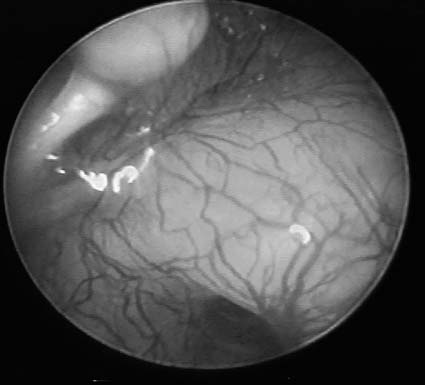
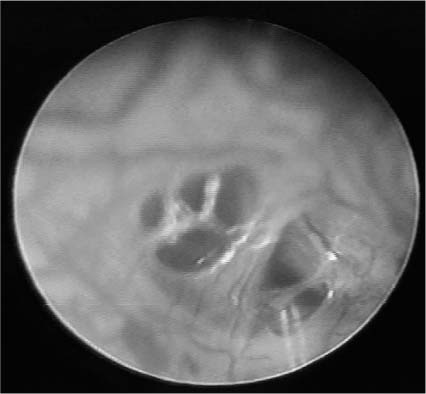
Chapter 21 Endoscopy has created new opportunities for minimally invasive techniques in middle ear and temporal bone surgery. Otologic surgery was revolutionized with the advent of the surgical microscope, but microscopes are limited to a direct line of sight visualization. Endoscopes bring the surgeon’s eyes into the depths of the operating field, being designed with wide-angle lenses that produce panoramic views extending into recesses hidden from the microscope. Endoscopes offer the potential for reducing open surgical exposure, reducing operating time, improving cholesteatoma eradication, and minimizing surgically induced artifacts during middle ear exploration for perilymphatic fistulas. Rigid Hopkins rod and fiberoptic endoscopes can be used in otologic surgery, but generally rigid rod lenses are preferred because of their superior resolution. Fiberoptic endoscopes employ thousands of individual light fibers, with each one creating a single pixel of the resultant image. The cladding and cement between fibers creates a “chicken-wire fence” appearance when images are sharply focused.1 Endoscopic images have an inherent spherical distortion or “fish-eye view,” and lack the three-dimensionality offered by the binocular operating microscope. Endoscopic magnification increases steeply as objects are brought into proximity with the lens and can approach the powers achieved with the operating microscope. Endoscopic surgeons learn to compensate for the variable magnification and two-dimensional images by watching how a structure and its surroundings are altered as the endoscope is moved in and out of proximity to it. The three-dimensionality of an image is re-created by its changes with endoscope motion. Transtympanic endoscopy utilizes instruments of 1.9 mm in diameter or less. Operating room exposures permit the use of 2.7- to 4.0-mm diameters that yield larger images with improved lighting clarity. Endoscopes have 0-, 30-, 45-, and 70-degree view angles. Illumination is by a halogen or xenon fiberoptic light source generally providing between 150 and 300 W. Images may be viewed directly through an endoscope lens, or more commonly, a charge-coupled device (CCD) camera is attached to the endoscope lens to deliver the images onto a monitor. Endoscopes are useful in the office for inspecting areas of the ear that are inaccessible to the operating microscope and for photodocumentation. The panoramic views achieved with a 2.7- or 4-mm endoscope are excellent for otologic photography. Endoscopes are useful to inspect the tympanic membrane or medial external auditory canal when the microscopic view is limited by canal stenosis or other obstructions. Defects or recesses in the external canal and the depths of mastoid cavities may be easily visualized. Tympanic membrane retraction pockets may be inspected to determine their depths and the presence or absence of cholesteatoma debris. Endoscopes may be passed through an existing perforation or myringotomy in the tympanic membrane to perform a limited middle ear exploration. The procedure may be done in the office or operating room. In the office, the patient is placed in the supine position in an exam chair. The ear is inspected through a speculum using an operating microscope. The tympanic membrane is anesthetized with topical phenol solution (United States Pharmacopeia) applied by dipping a 20-gauge (3-french) suction tip into the solution and dragging the bead of solution that adheres to the suction across the tympanic membrane over the incision site. An immediate blanching of the tympanic membrane is noted. Phenol is the preferred anesthetic because of its rapid onset of action and local cautery that produces a dry and bloodless field. A radially oriented myringotomy is made from the annulus to the malleus, overlying the site of anticipated pathology. An opening is created sufficiently large to atraumatically admit the endoscope and minimize the chance for inadvertent tearing of the tympanic membrane. A drop of defogging solution is applied to the tip of the endoscope and the excess blotted away by touching a cotton sponge to the side of the lens. It is important to avoid direct contact with the lens as it often smears the solution and blurs the image. A 0-degree endoscope is often used for the initial inspection of the middle ear because it yields a wide overall view of the middle ear. Close-up inspections in the area of suspected pathology are done with a 30-degree endoscope. It takes some practice to atraumatically maneuver an angled endoscope through a myringotomy because of its off-centered view. Endoscopic images may be viewed directly through the lens or with use of a CCD camera delivering the image to a video monitor. Surgeons with little endoscopic experience find it easier to look directly into the endoscope eyepiece. Although the image appears very small to the eye, it yields an adequate examination and it is simpler to maintain control of the endoscope within the ear. The use of a CCD camera increases the difficulty of use by introducing potential disorientation from rotation of the camera on the eyepiece, operating while looking at a remote video monitor away from the surgical field, and maneuvering the increased weight of the endoscope system. Experienced endoscopists, however, usually prefer video monitor images that appear considerably larger to the eye and offer a better appreciation of detail in the surgical field. A small ear speculum is placed deep into the external canal to help protect against inadvertent pain or bleeding from contact of the canal skin with the endoscope shaft. The speculum and endoscope shaft are held in the surgeon’s nondominant hand, and the endoscope tip is guided atraumatically through the myringotomy using fine fingertip movements. The camera and eyepiece are held in the dominant hand, supporting the weight and assisting in guiding the endoscope. The endoscope may be rotated to a small degree in situ, but it is generally safer to make large rotations of the view angle into the appropriate direction prior to insertion into the middle ear to minimize the potential for tympanic membrane trauma. Once the endoscope lens has fully passed through the tympanic membrane, a wide view of the middle ear can be realized (Fig. 21–1). Close-up and angled views, especially around overhangs, are best done with a 30-degree endoscope (Figs. 21–2 and 21–3). It is important to repeatedly ensure that the camera is properly oriented to avoid inappropriate movements in the middle ear due to disorientation. Patients may experience caloric-effect vertigo from the heat of a 300-W light source if it is in situ for more than 45 seconds. Withdrawal of the endo-scope relieves the vertigo, so the examination may continue by removing the endoscope periodically or by reducing the intensity of the light source. Vertigo has not occurred using a 150-W light source. There have not been any reported cases of thermal injury, but elevations of temperatures to 508C have been produced in dry temporal bones exposed for 2 minutes.2 FIGURE 21–1 Transtympanic endoscopic view of middle ear with 1.9-mm, 0-degree angled Hopkins rod endoscope. FIGURE 21–2 Transtympanic endoscopic view of superior mesotympanum with 1.9-mm, 30-degree angled Hopkins rod endoscope. At the conclusion of the exam, the myringotomy is inspected under the microscope to determine that the margins show no significant trauma and are nearly in approximation. Wide gaps or inadvertent tears may be repaired with adhesive Steri-Strips, Gelfilm, or cigarette paper. Tympanic membrane injuries are generally avoided by making the initial myringotomy sufficiently long to pass the endoscope easily. Water precautions and avoidance of nose-blowing are recommended for 2 weeks after the procedure.1 FIGURE 21–3 Transtympanic endoscopic view of round window niche with 1.9-mm, 30-degree angled Hopkins rod endoscope. The author has performed 114 transtympanic endoscopic procedures in the office to date without any complications. There have been no cases of persistent hearing loss, vertigo, infection, or persistent perforation. Surgical exploration has previously been the “gold standard” for establishing the diagnosis of perilymphatic fistula. However, the criterion for determining the presence or absence of a fistula, the accumulation of fluid in either the round or oval window niches, has been demonstrated to be inaccurate because of the inability to distinguish between artifacts such as tissue transudates or injected anesthetics versus perilymph accumulating in the dependent window niches.3 These artifacts can be reduced by a minimally invasive endoscopic exploration through a phenol cauterized myringotomy. The middle ear is visualized in as undisturbed a state as possible. A diagnostic endoscopic perilymphatic fistula exploration can be performed in the office. It may also be done in the operating room, especially if an open repair is anticipated after the diagnostic exam. A myringotomy is made radially halfway between the shadow of the round window niche and the distal end of the incus’s long process, which are usually visible through the tympanic membrane. It has been demonstrated that endoscopic and microscopic explorations have comparable resolution for the detection of a leaking fistula.4
ENDOSCOPIC MIDDLE EAR AND MASTOID SURGERY
EQUIPMENT
ENDOSCOPY OF THE EXTERNAL AUDITORY CANAL AND TYMPANIC MEMBRANE
OTOLOGIC MIDDLE EAR ENDOSCOPIC SURGERY
TRANSTYMPANIC ENDOSCOPY
PERILYMPHATIC FISTULA EXPLORATION
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree