Endocrine Disease and the Eye
H. C. Chen
Eva M. Kohner
DISORDERS OF THE THYROID GLAND
The thyroid gland is situated anterior to and on either side of the upper part of the trachea and the thyroid cartilage. Its principal function is the secretion of thyroxine (T4) and triiodothyronine (T3). Both hormones increase cellular metabolism and have widespread physiologic action, including enhancing the adrenergic state; of the two, T3 possesses a greater level of activity.
The synthesis of thyroid hormones is dependent on the availability of dietary iodine, which is incorporated by the thyroid gland into individual tyrosyl residues of a complex molecule called thyroglobulin. These individual residues merge to form T3 and T4, which are cleaved from the parent thyroglobulin molecule for release into the blood stream. Thyroid hormones are transported in the blood stream bound principally to thyroxine-binding globulin. Only a very small percentage (less than 0.5%) circulate “free” or unbound, and it is this fraction that is responsible for the physiologic action.
The function of the thyroid gland is controlled by the anterior pituitary gland via the secretion of thyroid-stimulating hormone (TSH), which is itself influenced by the release of thyrotropin-releasing hormone by the hypothalamus; TSH release by the anterior pituitary is partly controlled by the thyroid hormones through a negative feedback mechanism.
HYPERTHYROIDISM
Hyperthyroidism or thyrotoxicosis is characterized by the overproduction of thyroid hormones. A small proportion of patients have only elevated T3 levels, but the majority possess high levels of both T3 and T4. Thyrotoxicosis may be classified broadly into two groups: (1) where the thyroid gland is either diffusely hypertrophic and hyperplastic (Graves’ disease); or (2) where single or multiple hyperactive nodules exist in the gland.
Graves’ disease is a condition that predominantly affects females and, although it may occur at any age, has a peak incidence in the third and fourth decades. In almost all patients with this autoimmune disease, immunoglobulins are directed against the TSH receptors on the thyroid cellular membrane. As with other autoimmune conditions, there is a strong familial tendency for Graves’ disease: it has been associated with the HLA antigens B8 and DR3 in whites and with Bw35 in Asians.
It usually presents insidiously, although rapid and dramatic presentations are not uncommon; the exact precipitating mechanism is unknown. Systemic symptoms include weight loss, increased sweating and heat intolerance, palpitation, fatigue, and diarrhea. Examination of a patient with Graves’ disease may reveal a goiter, a fine tremor, palmar erythema, finger clubbing, vitiligo, alopecia, pretibial myxedema, and a multitude of cardiovascular signs (e.g., tachycardia, atrial fibrillation, bounding peripheral pulses).
Ocular Involvement
Ocular involvement is an almost integral part of the clinical presentation of Graves’ disease; however, the systemic and eye manifestations are generally considered to run independent courses. Although most of the systemic features of Graves’ disease can be attributed to the increased activity of thyroid hormones, the ocular involvement is less obviously linked to this. Graves’ ophthalmopathy, preferably termed thyroid-associated ophthalmopathy (TAO), may occur in the absence of overt systemic signs of hyperthyroidism (approximately 10% of cases; more subtle analysis often reveals evidence of systemic thyroid disease in most of these cases), or even after the systemic disease has been treated adequately. TAO is the most common cause of proptosis in adults; the term exophthalmos is used exclusively to describe the proptosis of TAO and will be used henceforth in this section.
Compared with Graves’ disease, hyperthyroidism due to “toxic” thyroid nodules is less common and generally occurs in older patients. Ocular involvement is not a common feature of this condition.
Presentation
Patients with TAO may present with a wide range of symptoms. Both eyes are usually affected, often to differing degrees, or the involvement may be unilateral. Although the condition may be selflimiting, it often has a tendency to produce episodes of acute activity lasting several months interspersed by relative quiescence, but the progression in severity from any one acute episode is not likely to regress as a result of fibrotic changes. The natural tendency of the disease process is to eventually “burn out” within 2 to 3 years.
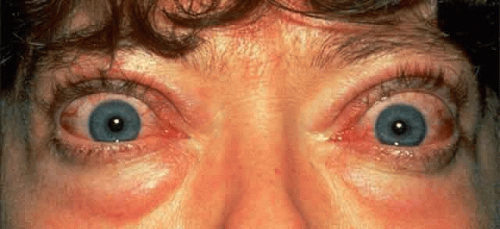
Lid puffiness and irritable, watery eyes are common symptoms; complaints include a feeling of “grittiness” in the eyes and profuse tearing despite the absence of apparent irritants. Affected eyes may feel gritty for several reasons: (1) lid retraction and exophthalmos may cause problems with corneal lubrication, and superior limbic keratitis is a well-recognized association; (2) thickened conjunctival folds may obstruct the drainage of tears into the lower lid punctum, evidenced by a fullness of the conjunctiva at the medial canthus; and (3) conjunctival hyperemia commonly accompanies inflammation of the extraocular muscles. The injection is usually most marked over the insertions of the extraocular muscles (Fig. 1).
Cosmetic problems associated with protruding eyes are also common; this protrusion is usually asymmetric and is due to a combination of upper lid retraction and exophthalmos. Lid retraction is among the earliest and most common signs causing exposure of the superior sclera and widening of the palpebral fissure. It is one feature of TAO that can be partly attributed to the systemic effects of hyperthyroidism; increased stimulation of the smooth muscle retractors in both the upper and lower lids can result from heightened adrenergic activity. Upper lid retraction also results from a tightened inferior rectus due to inflammation and fibrosis, and this tightening leads to compensatory overactivity of the superior rectus/levator palpebrae complex. Similar inflammatory and fibrotic involvement of the levator palpebrae muscle will add further to upper lid retraction.1 This wide-eyed staring appearance is often accentuated by the presence of exophthalmos (see Fig. 1).
When mild, the signs and symptoms of exophthalmos may be limited to a feeling of grittiness, conjunctival injection, and chemosis; however, severe corneal exposure, which is often complicated by a poor Bell’s phenomenon because of restrictive myopathy, can lead to pannus formation and ulceration, corneal scarring and infection, and visual impairment. Because exophthalmos is secondary to increased retro-orbital mass, it can be associated with optic nerve compression, although significant nerve compression may be present in its absence.
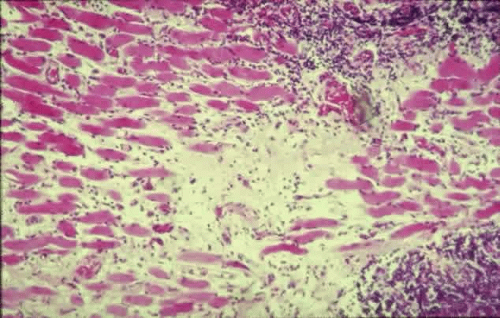
The principal visual symptoms are diplopia and reduced visual acuity. According to Fells,2 patients with thyroid-associated diplopia see vertically separated images upon waking in the morning, which improve within minutes but recur later during periods of fatigue or alcohol intoxication. Defective ocular motility in TAO is due to inflammatory engorgement of the extraocular muscles: the inferior and medial recti more commonly and the lateral and superior recti less commonly. The restriction in function may initially be reversible, but is eventually permanent due to cicatricial, fibrotic elements (Fig. 2). Since the inferior rectus muscle is the most commonly affected, upgaze can often lead to elevated intraocular pressure.
Optic nerve compression (compressive neuropathy) is one of the serious complications of TAO and leads to reduced visual acuity. Its prevalence has been reported at approximately 10% in a prospective study of 101 patients attending a combined thyroid-eye clinic during a 5-year period3; this figure may be artificially high because of the specialized nature of this clinic. It is more likely that less than 5% of patients with Graves’ disease will develop sight-threatening compressive neuropathy. Optic nerve involvement is generally accepted to be due to compression at the orbital apex by enlarged extraocular muscles.4 These patients are likely to be older and male; they commonly exhibit limitations of extraocular movements with significant vertical deviation.5,6 Other causes of reduced visual acuity are corneal exposure and desiccation, with their attendant complications, and chorioretinal striae involving the macula, due to an increased retro-orbital mass.
In an attempt to clarify the nomenclature pertaining to thyroid-related eye disease, Werner classified the eye changes into seven categories, based on an original classification by the American Thyroid Association7; Werner’s classification is presented in Table 1. Although useful as a means of classifying the severity of involvement, its usage is limited because it lacks a means of measuring the rate of progression or treatment-induced regression of clinical activity. The signs of TAO can be subdivided into those pertaining to the lids, conjunctiva and cornea, globe, extraocular muscles, and fundus. These signs are summarized in Table 2.
TABLE 1. Werner’s Classification of Thyroid-Associated Ophthalmopathy* | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 2. Signs of Thyrotoxicosis | |
|---|---|
|
Pathogenesis
Present understanding of the pathogenesis of TAO remains unclear; however, as with the thyroid component, autoimmune mechanisms have been implicated. The association between the ocular disorder and a hyperactive thyroid gland may be the result of a linkage between the two conditions and a primary autoimmune disorder manifested through a variety of circulating autoantibodies acting on two different end-organs sharing a hypothetical autoantigen. Currently it is unclear what this autoantigen is, but several candidates have been proposed, including a 64-kilodalton (kd) protein found in thyroid and eye-muscle plasma membranes8,9 and the TSHreceptor protein.10,11 Antibodies directed against a 64-kd protein expressed by extraocular muscle has been reported to be present in 33% of patients with TAO and in 75% of patients with severe eye disease.12 There may also be other antigens expressed in the orbit similar to both thyroglobin and antigens expressed on thyroid microsomal cells, since antibodies directed against them have been identified in the orbit.13
The stimulatory strength of these respective antibodies vary among patients. In cases predominantly involving the eye, the antibodies directed against the thyroid may be weak. In cases where these antibodies prevent the normal binding of TSH, there may be an association between hypothyroidism and TAO. It has also been suggested that a common autoantigen exists (e.g., the 64-kd antigen) that is responsible for the milder eye disease seen in the majority of patients with Graves’ disease; in patients with severe disease, other eye-muscle-specific antigens have been proposed.14 It has been demonstrated that IgG from patients with TAO stimulated the growth of extraocular myoblasts, compared with sera from controls and patients with Graves’ disease who had no ocular involvement. The effect was relatively specific to these cells, whereas the effect on skeletal myoblasts was less marked.15
The inflammatory infiltration of the extraocular muscles consists principally of activated T-cells together with smaller numbers of B-cells, macrophages, and mast cells.16 The infiltration is mainly interstitial and is accompanied by increased fibroblastic activity induced by cytokines derived from the immune cells, leading to deposition of glycosaminoglycans and collagen as well as edema. The eventual outcome is fat cell infiltration and fibrosis (Fig. 3). The muscle fibers appear normal, with the exception of subsarcolemmal deposits of lipid and glycogen, and there is an absence of muscle-cell destruction.
It is unclear which cell type expresses the offending antigen, but current understanding favors the fibroblast. According to Weetman,17 the histologic picture reveals a pathologic process directed principally against the retrobulbar fibroblast, rather than muscle cells, but this may be just a manifestation of the presence of large numbers of immune cells attracted there by a nonfibroblastic source. Antibodies against the TSH-receptor have been shown to stimulate collagen synthesis by fibroblasts18; retrobulbar fibroblasts have also been demonstrated to possess TSH-receptor-encoding RNA.19 However, an immune process directed against muscle cells is suggested by the finding of higher levels of eye-muscle-binding antibody in patients with TAO, whereas levels of antifibroblast antibody were unremarkable.20
Also unclear is why the extraocular muscles are selectively involved in TAO while other skeletal muscles in the body are spared. Schmidt and associates21 reported that hyperthyroidism alters the immunocompetent cell population in extraocular muscles, but not skeletal muscles. Another possible explanation is that extraocular muscles also possess more spindles and connective tissue and have a greater blood supply than skeletal muscles.
Most of the infiltrative pathology seen in TAO traditionally has been attributed to the retro-orbital deposition of glycosaminoglyans, with associated edema and inflammatory cell infiltration of the muscles. More recently, Hudson and colleagues22 proposed that, in some cases, the exophthalmos may be due to passive orbital venous congestion from a partial obstruction of the superior ophthalmic vein. They based this view on the observation that exophthalmos is sometimes present with little enlargement of the extraocular muscles, with the exception of the superior rectus muscle together with congestion of the superior ophthalmic vein with which it is closely linked. The obstruction could be purely compressive, or there may be an element of contiguous inflammation from the adjacent muscle.
Orbital fat content is not thought to play a significant role in compressive optic neuropathy. Feldon and co-workers23 demonstrated that patients with optic nerve compression had greater extraocular muscle volumes than those without optic nerve involvement, whereas both groups had similar fat content; orbital fat volume was found to decrease with increasing muscle size.
Diagnosis
Diagnosis of TAO is based on clinical findings, sometimes in the absence of hyperthyroidism. Symptoms and signs indicating active inflammation (e.g., pain, conjunctival injection, edema) are particularly important because they influence the management strategy.24 The degree of exophthalmos should be assessed with an exophthalmometer (a protrusion of 20 mm or more is suspicious), and the intraocular pressure should be measured with the patient in the primary position and with attempted upgaze. Photography is a useful method of recording clinical status.
Clinical investigations may reveal elevated plasma T3 and T4 levels (the free thyroxine index can be determined after correction for plasma protein binding) and in most cases decreased plasma TSH. Antibodies that may be detected include those directed against TSH-receptor, thyroglobulin, and thyroid membranes.
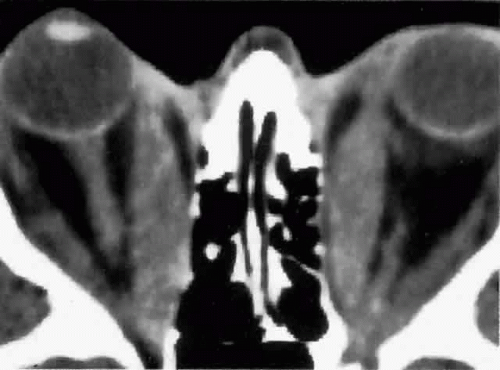
Computed tomography (CT), most revealing in the coronal plane, and ultrasonography are useful methods for assessing extraocular muscle thickness (Fig. 4). Magnetic resonance imaging (MRI) has been advocated as a means of differentiating between extraocular muscles that are actively inflamed and those that are fibrosed25,26,27; both muscular problems can restrict ocular movement, but the former is amenable to immunosuppressive intervention. The T2 relaxation time of MRI is directly proportional to the water content of the tissue scanned: since inflamed tissues are edematous, they should have longer T2 times. MRI is also thought to be better than CT in providing views of the orbital apex and may therefore be better for evaluating optic nerve compression.2
Extraocular muscle volume is inversely proportional to ocular motility, especially for horizontal movements. Therefore, the peak velocity of saccadic eye movement, measured with reflective infrared oculography, has been proposed as another means of assessing clinical severity.28,29,30 The degree of optic nerve compression has been found to increase as peak velocity decreases, particularly with larger angles of eye movement.29
Patients with optic nerve compression present with reduced visual acuity, which may be clinically substantiated by the presence of an afferent pupillary defect and visual field loss. More sophisticated means of detecting early compressive pathology include the pattern electroretinogram, cortical visual evoked potentials, and color contrast sensitivity along the tritan axis.31 Depending on the degree of severity, fundal examination may reveal varying degrees of venous congestion, swollen optic discs, and chorioretinal striae (usually horizontal). It is important to note that 40% to 50% of patients with optic nerve compression may have a normal fundal appearance.5,32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree