Fig. 1
Emergency Airway Management Algorithm for Difficult-Critical Airways. Note the differences and similarities between neonatal emergency algorithms and pediatric algorithms. (a) Neonatal algorithm (courtesy of The Neonatal Airway Program–CHOP). (b) algorithm, (adapted from Wheeler and Shanley, et al. eds. Resuscitaiton and Stabilization of the Critically Ill Child. Springer, 2009
Implementation of Strategy: Mobilizing the Airway Team
While unnerving, dealing with a critical airway in a small neonate can be managed with five easy steps. When possible, anticipation, identification, preparation, mobilization, and execution should be the immediate steps that are set forth by the neonatal care team during an airway emergency (Fig. 2).
Fig. 2
“Pyramid of Action.” Useful for quick thinking on step-by-step decision tree
Anticipation
It is never a good idea to extubate or manipulate an unstable airway without alerting another skilled airway person. In the neonatal unit, emergency department, or in transport of an infant with a critical airway, alert another physician, anesthetist, or advanced practitioner. Making nurses and respiratory therapists aware of the plan to manipulate the endotracheal tube should be included in the first step of the process as well, so the entire care team can anticipate the clinical course.
Identification
All caretakers should be made aware of the airway status of the neonatal patient. Furthermore, diagnoses and comorbidities need to be carefully evaluated for issues that would confound an airway emergency. Becoming familiar with the numerous and varied diagnoses causing acute airway obstruction (refer to Fig. 11 of chapter “Challenges of the Neonatal Airway”), is a good starting point. Additionally, measures should be taken so that patients with a history of a difficult or critical airway are readily available and recognized as such.
Preparation
A solid airway emergency plan includes equipment that is both ready for use and well known to those who will use it. A simple tackle box with laryngoscopes, multiple sized endotracheal tubes, stylettes, laryngeal mask airways, oral and nasal airways, and facemasks is all one needs to have at the bedside. Another option in a busy airway center is a dedicated mobile cart that has all the necessary equipment in labeled drawers. Additionally, more specialized ENT equipment, such as halogen light sources with fiberoptic bronchoscopes, specialized laryngoscopes, videolaryngoscopy and even a large display monitor should be available in large center neonatal-infant ICUs with large airway pathology volume [19, 27, 28].
Mobilization
Recruitment of the airway team in an instant is essential to any successful airway emergency process. Specialized reliable paging systems should be able to quickly alert trained personnel (physicians, respiratory therapists, nurses, clerks) for quick activation and mobilization of the team.
Execution
With a well-organized team, equipment available at the bedside, and roles clearly established, the final step in the process is addressing the critical airway. The exact techniques for establishing an airway are going to be specific for the individual patient. As attempts are made to rectify the obstruction, the team will work up the hierarchy of equipment and personnel available until the problem is resolved.
Education/Simulation Drills
Integral to being prepared is education and simulation. Education has to be global, widespread, and include all caregivers. An essential component of this education is frequent updates about equipment, new personnel, and newly established algorithms. There also must be an insurance of competency for all members of the team. The way to validate this competency is via simulated clinical scenarios. This is a relatively novel approach to training and should be utilized frequently, especially for procedures that do not occur often. Simulation should include key team members and key scenarios such as unplanned extubation, difficult airway conditions, critical airway conditions, and unplanned delivery of an infant with a critical airway.
Software and mannequins that allow for simulated reality are integral support components for training. These technologies allow for immediate feedback during procedures via changes in vital signs, respiratory distress symptoms, etc. These simulations should occur on a regular basis, at least once a week, and in a variety of different environments where these emergencies may occur. Debriefing and feedback should be a regular part of concluding simulated training and education sessions [62].
Activating Airway Emergency Response Team (Fig. 3)
Fig. 3
“Algorithm of Action.” Useful for actionable steps to mobilize team members
Necessary Equipment for Airway Emergency Preparedness in the Neonate and Infant
Noninvasive Equipment
Bag Mask Ventilation
Bag mask ventilation is the cornerstone of neonatal resuscitation and is always attempted first. As mentioned previously in one study in premature infants, it can be difficult to adequately seal the facemask during bag mask ventilation thereby underestimating the delivered tidal volume [13].
Oral Airway/Nasal Trumpet/Endotracheal Tube
Oral airways, nasal trumpets and nasal endotracheal tubes are often overlooked as a quick method to bypass tongue-based obstruction. These tools can provide a nasopharyngeal airway that can be used for hand ventilation and suctioning during emergencies (Figs. 4 and 5).
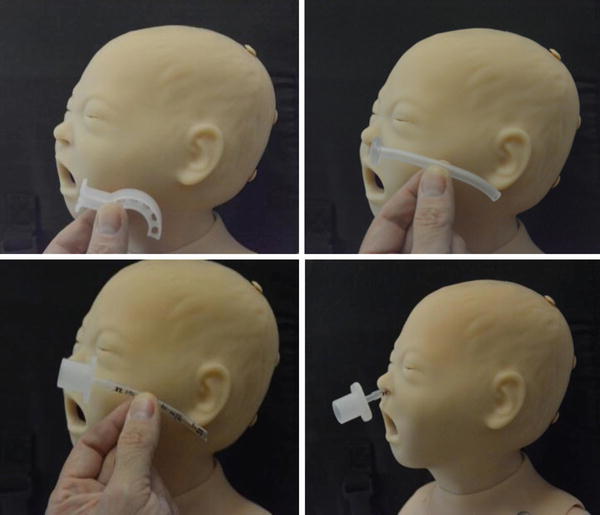
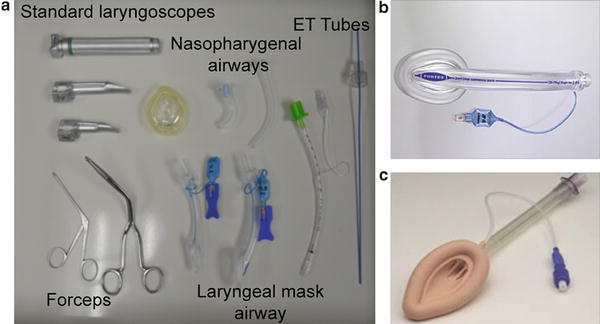
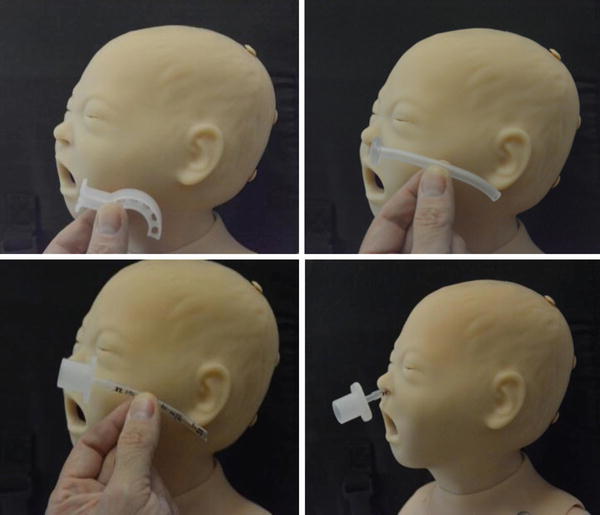
Fig. 4
Nasal Pharyngeal Airways. Guide to insertion, placement depth and stabilization of NP airways in life threatening oral obstruction. Note the nasal ETT is useful due to ease of bagging with connector
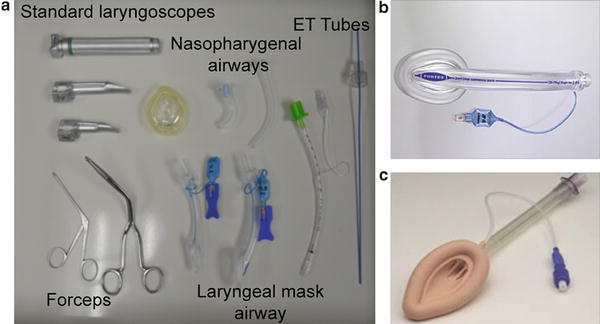
Fig. 5
Picture of essential intubation equipment-laryngoscopes, masks, LMAs, intubating nasal forceps
Laryngeal Mask Airway (LMA)
Also often overlooked are laryngeal mask airways. The LMA is a simple, easy to place device that can provide immediate access to the airway. Recently, LMA has been added to the tool set for noninvasive neonatal resuscitation. In a study evaluating newborns requiring positive pressure ventilation, the LMA was successfully inserted on the first attempt and provided an airway with no complications recorded [39]. Intubating through an LMA is also possible when the proper equipment is mobilized beforehand. A bronchoscope spring-loaded with an endotracheal tube can be threaded through the LMA to intubate the trachea [27, 39, 56] (Figs. 6 and 7a–e).

Fig. 6
Springloading a bronchoscope-LMA with an ETT. A useful skill to allow rapid intubation over a bronchoscope during intubation of critical airway

Fig. 7
AirwayCart and equipment: (a) airway cart, (b) Olympus Monitor-video recorder, (c) bronchoscopes, (d) special laryngoscopes—high intensity light source, (e) Tracheostomy equipment
Having a well-equipped, sturdy, and mobile cart containing all the necessary equipment is a top priority in an effective response to an airway emergency. The cart should have 6–7 drawers that are clearly labeled with basic airway equipment. Scopes, tubes, and masks should be kept in the upper drawers for easiest access. Larger equipment (fiber optic equipment and light sources, tracheostomy surgical trays) should be kept in the bottom drawers. Basic emergency equipment should also be kept in a medium-sized box kept atop the cart for rapid deployment to remote areas.
Direct/Indirect Laryngoscopy Equipment
Fiber Optic
Fiber optic laryngoscopy is frequently used for neonatal airway emergencies, particularly in sizes 2.2 and 2.8. Due to the size of the neonatal airway and limitations on the endotracheal tube, these are the only scopes that can be used. These scopes are equipped with xenon gas light source to provide optimal visualization of structures. As mentioned previously these, can be spring-loaded and used through an LMA. Furthermore, visualization with these scopes ranges from the nares to the carina, making them incredibly versatile. These are often specially handled and sterilized through very stringent procedures.
Fiber Optic Monitor/Light Source
Necessarily supporting fiber optic scopes is a cart combining both the Xenon source and a large HD flat-screen monitor with recording capabilities. This cart is mobile as to allow for rapid access to the bedside.
Direct
Traditional Neonatal Laryngoscope
The most commonly used laryngoscopes. These come in sizes 00 to 1-blade and should be available in all emergency airway carts.
Specialized Neonatal Laryngoscopes
More sophisticated scopes should be available for higher-level airway personnel (i.e., ENT and Anesthesia). These scopes require a portable halogen light source for illumination of the airway [61].
Indirect
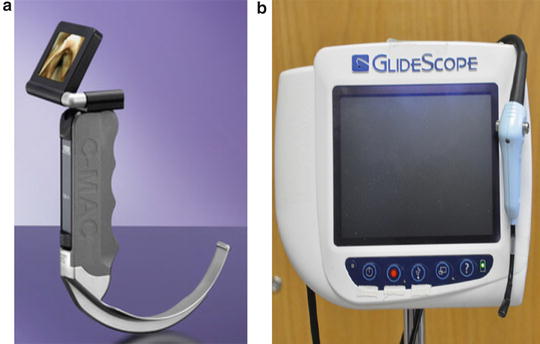
Indirect video laryngoscopy has gained immense popularity for use in airway emergencies in neonatal units due to adoption of appropriate sizes for the smallest of infants. There are a few products on the market that can be used in neonates. The learning curve for these technologies is a bit steeper than some the traditional techniques. Practice and frequent use are the mainstays for efficacy (Fig. 8a, b).