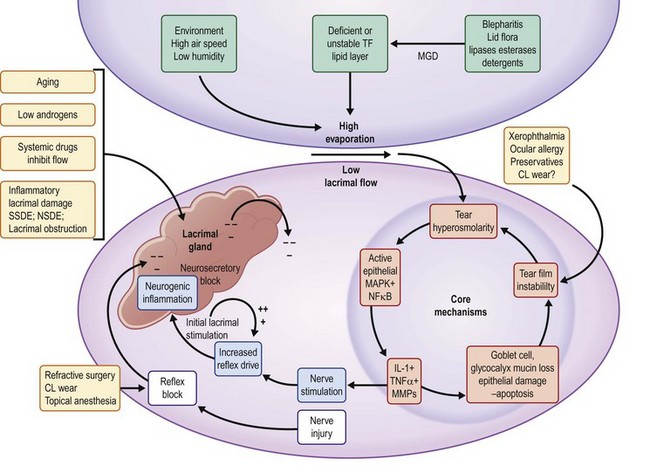
11 Epidemiology is that branch of medical study which concerns itself with the frequency, distribution, determinants and assessments associated with disease. In this chapter we shall cover major studies and results, concentrating on the most recent ones, which affect clinical understanding of dry eye disease (DED). For a comprehensive review of this field, including an assessment of symptom questionnaires, the reader is referred to the 2007 Report of the International Dry Eye Workshop (DEWS), chapter on the epidemiology of dry eye disease.1 As noted in the above referenced publication, there has been a significant increase in both interest in and studies of the prevalence and incidence of DED, particularly since the 1990s. At the first Tear Film and Ocular Surface Society international meeting in 1992, a call for a ‘consensus conference’ was made. This resulted in the National Eye Institute/Industry workshop report, which determined that there was a paucity of data concerning prevalence and incidence of DED. New methodologies in the field of epidemiology and statistical analysis have been employed to expand our knowledge in this regard. Clinicians have long recognized that complaints relating to DED are common in clinical practice. In an attempt to apply scientifically valid methodologies to this enquiry, an agreed definition is essential. The DEWS report, building on an earlier text, defined DED as ‘a multifactorial disease of tears and ocular surface that results in symptoms of discomfort, visual disturbance and tear instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface’.2 Armed with this widely agreed definition, many studies have been published. These studies address different population groups throughout the world. They agree that DED is a very common condition, increasing in frequency with advancing age. The estimates of prevalence (proportion of a population with the disease at a given time), range from about 5% to over 30%. These differences may be related to different population characteristics but primarily to differences in the characterization of subjects with disease. Various names have been attached to dry eye. These include keratoconjunctivitis sicca (KCS), dry eye syndrome, and dysfunctional tear syndrome (DTS). KCS is a traditional name implying dryness and inflammation of the ocular surface. Its use began to wane with the recognition that all cases of the condition do not demonstrate a lack of tears and with recognition of the role of inflammation in the pathogenesis of the disease process. Dry eye or dry eye syndrome became the predominant terms in use throughout the English-speaking world and even in non-English-speaking countries, in which the term is widely recognized. With publication of the Delphi report in 2006,3 a new term, dysfunctional tear syndrome, was proposed. The issue was put to a vote at the Tear Film and Ocular Surface Society meeting prior to publication of the DEWS report. A majority of the expert participants preferred the term ‘dry eye’ or ‘dry eye disease,’ citing its wide recognition, not only by clinicians and researchers but also by patients.4 The latter term emphasizes the increasingly well-characterized pathophysiological processes of a discrete disease. Both DED and DTS are currently in use. There are a number of risk factors for the development of DED (Fig. 11.1). Reference 1 lists these factors and stratifies them based on levels of evidence. The most obvious factors associated with DED are increasing age, female gender and hormonal changes. Connective tissue disease is associated with more severe forms of DED, e.g. Sjögren’s syndrome and graft-versus-host disease. Dry eye disease occurs with greater frequency in women, particularly in the menopausal and postmenopausal years. The preponderance of evidence has demonstrated that androgen insufficiency is a principal risk factor for both lacrimal gland involvement and meibomian gland dysfunction (MGD). The female : male ratio decreases with advancing age as large segments of males with MGD become affected. The distribution of subtypes of DED, based on glands primarily affected is discussed in the section on pathophysiology later. A recent recognition is the impact that DED has on visual function. A hallmark of DED is tear film instability.2 This is manifest in a rapid tear breakup time, during the inter-blink interval. This effect is not apparent in standard high-contrast visual acuity testing, in which the subject can blink and transiently re-form the tear film. However, within several seconds in dry eye patients, the tear film breaks up causing a significant loss of resolving power and a drop in acuity. A Japanese study has documented that inter-blink visual acuities of 20/60 and greater are common.5,6 Patients rarely recognize the connection between their visual problem and dry eye, usually complaining of decreased reading time, or ocular fatigue. This is probably caused by repeated blinking in an unconscious effort to clear vision. Other parameters of visual loss in DED, such as contrast sensitivity and Shack Hartmann aberrometry measurements may be also affected.7,8 These features of DED lead to the substantial degradation of quality of life measures in the disease. In one study, the equivalent burden of having moderate to severe dry eye was similar to that of moderate to severe angina.9 The literature states that dry eye is a symptom-driven disease.1 This implies that symptoms are a requisite component of the diagnosis. While symptoms certainly play a major role in the disease, recent studies have noted two seemingly paradoxical observations, i.e. that many patients with early/mild disease have symptoms greater than any objective findings, and that in a subset of patients with severe disease there is a paucity of symptoms. The latter is thought to be due to a decrease in sensory perception associated with inflammation; the former has been linked to a hyperalgesia, associated with early nerve ending response to injury. In a recent presentation of an observational study, only 60–70% of patients with DED were reported to have symptoms (as measured by the Ocular Surface Disease Index).10 The remaining 30–40% do not present with measurable symptoms. Reliance on symptoms alone for diagnosis would therefore, seem unwise. Although there are numerous risk factors for the development of dry eye disease, the final common expression of the pathophysiology includes tear film hyperosmolarity and instability. The concept of a functional lacrimal unit has been developed in which the secretory glands (lacrimal, meibomian and mucin-producing surface cells), the entire ocular surface, and the lids are linked by a neural network, which responds to external stimuli to maintain a stable tear film and underlying ocular surface, necessary for subserving clear vision.11 This unit has recently been enlarged to include the nasolacrimal duct, which has receptors that respond to volume changes. A key concept to understanding the development of DED is the breakdown in this unit leading to an unstable, concentrated (hyperosmolar) tear film. In Table 11.1, this concept is illustrated in a graphic, which the entry points or risk factors in the periphery lead to the core central mechanisms.2 As these mechanisms (e.g. lacrimal hyposecretion and/or meibomian gland dysfunction) come into play, there is a mutually reinforcing cycle of dysfunction leading to inflammation in the ocular surface and lacrimal glands. This vicious cycle concept has been developed by Baudouin12 and is illustrated in Figure 11.1.
Dry Eye Disease
Epidemiology and Pathophysiology
Introduction
Nomenclature
Risk Factors for Dry Eye Disease
Impact on Visual Function
Role of Symptoms in DED
Pathophysiology of Dry Eye Disease
Dry Eye Disease: Epidemiology and Pathophysiology