11 Penny A. Asbell and Ömür Ö. Uçakhan According to ICEE 2002 estimates (personal communication, July 2002), the years leading up to 2020 are expected to yield an enormous increase in the global contact lens market through two main influences: the rising number of people with myopia and presbyopia, and the demand from huge emerging markets such as China and India. By 2020, more than 2.5 billion people worldwide will be myopic, and owing to the decrease in mortality rates in almost all countries, the U.S. Census Bureau estimates that there will be more than 2.3 billion people over the age of 45. Despite the continuing growth of the contact lens market from previous years, with some 2.8 million new wearers entering the U.S. market each year, roughly as many existing wearers drop out. It has been estimated that approximately 5 to 10% of contact lens wearers stop wearing their lenses during any given year.1 The estimated number of permanent contact lens dropouts in the United States ranges from 10 to 16 million people.2 It has been estimated that 10% enter the market every year and 10% drop out. This is an alarming trend and does not include the temporary discontinuations that range from 30 to 50%, and as many as half of these people may drop out for 2 years or longer (Table 11-1).3 The major reasons for contact lens discontinuation have been consistent throughout several studies—dryness and dryness-related discomfort. Contact lenses have been described as “widely used on-eye prostheses.”4 Because they rest within the tear film, safety and performance of contact lenses are strictly dependent on the quality and quantity of the preocular tear film.4,5 On the other hand, the contact lenses themselves ultimately alter the integrity and stability of the tear film, which in turn affect the ocular surface as well as the contact lens itself.4–7 In 1995, a report from National Eye Institute/Industry workshops indicated that “contact lens-related dry eye” is a major subclassification of dry eye disease, the epidemiology and etiology of which are still elusive.4
Dry Eye and Contact Lenses
Key Points
♦ Contact Lens-Tear Film Relationship
|
♦ Epidemiology
Determination of prevalence of dry eye in contact lens wearers is hampered by the nonspecificity of the symptoms, the difficulty in applying few measurable physiological diagnostic tests, and the lack of correlation between dry eye symptoms and available clinical tests.1,8,9 Therefore, most data are based on the patients’ subjective reports of symptoms.10–12
Dry eye symptoms are more common in contact lens wearers than in the general population. Several studies have reported a significantly higher frequency of dry eye symptoms in contact lens wearers than nonwearers, indicating contact lens wear is a provocative condition for tear dysfunction.13–20 In studies in which the same subjects compared their symptoms with and without contact lenses, eye dryness was reported to be significantly more frequent and severe when wearing contact lenses than when not.8,9,21,22
In a large-scale study performed on 150 presbyopes, symptoms of dryness were reported in 28% of the subjects at baseline and in 68% of subjects after wearing contact lenses for 6 months.23 In this study, females seemed to report symptoms of dryness more frequently, but age did not seem to be a significant factor in reporting symptoms. The authors concluded that dry eye symptoms seemed to be influenced by contact lens wear rather than age or gender.
Furthermore, the problem is probably getting more prevalent, and eye care practitioners have started seeing more and more cases of dry eye in contact lens wearers than ever before. The reasons for this are manifold. First, middle-aged people are more likely to be contact lens wearers today than a generation ago, and baby boomers who have worn contact lenses all through their lives wish to stay with their lenses as their eyes age. Market statistics have indeed revealed that the average age of lens wearers is increasing, and although teens represented the largest group of new entrants to the vision-correction market at 36% in 2003, this was followed by emerging presbyopes. Patients older than 35 years will soon constitute the majority of wearers, and that would include women over 35, a demographic group that is particularly susceptible to dry eye. Second, certain medications known to cause dryness are commonly used today, including oral contraceptives, antihypertensives, tricyclic antidepressants, antihistamines, anticholinergics, ibuprofen, and scopolamine patches. Third, climate and environmental factors also play roles. A higher percentage of the U.S. population is moving to warmer, drier climates such as the Southwest. Environmental factors such as widespread essential usage of computers in the workplace, air-conditioning, central heating, and smoke probably aggravate contact lens-related dry eye (Table 11-2).20
|
As mentioned earlier, dry eye and dryness-related discomfort are the major causes of contact lens intolerance and discontinuation.3,5,18,24 Various surveys have been performed, and the prevalence of dry eye symptoms in contact lens wearers has been reported to range from 20 to 78%.8,9,12,18,20,25–28 Even among successful, full-time soft contact lens wearers, up to 38% were reported to have dryness.8
A survey of optometric practices in the United States showed that 18 to 30% of contact lens wearers had symptoms of dryness, 12 to 21% had sufficient symptoms to reduce their wearing time, and 6 to 9% could not continue wearing their contact lenses because of dryness symptoms.29
Data from other countries are not encouraging either. In the United Kingdom, some 2.1 million contact lens dropouts are reported, which represent 60% of contact lens wearers and is the reason for the decline in the total number of contact lens wearers in that country.30 Symptoms of ocular dryness were the most frequent reasons for abandoning contact lens use, accounting for about 13 to 22% of such cases.31
♦ Pathogenesis
According to the functional unit theory, contact lenses represent a major perturbation to the ocular surface because mechanical trauma, hypoxia, toxicity, or inflammation due to contact lens wear could cause corneal damage directly and lead to secondary lacrimal gland damage.32 Therefore, low-grade ocular surface insults secondary to contact lens use can lead to inflammation and may cause or exacerbate symptoms and signs of dry eye.4,32–34 Figure 11-1 summarizes the possible pathogenic mechanism of contact lens-induced dry eye.
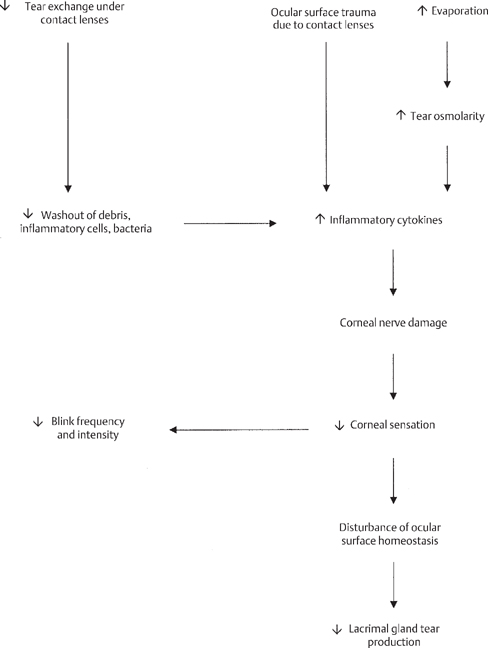
Figure 11-1 Possible pathogenic mechanism of contact lens-induced dry eye.
Tear exchange, especially under soft contact lenses, is known to be modest, and contact lenses decrease washout of debris, inflammatory cells, and bacteria away from the ocular surface by retarding the elimination of tear fluid underneath.35 Increased residence times of inflammatory cytokines or other mediators on the ocular surface would then cause corneal nerve damage, decreasing corneal sensation.13,36,37 Decreased corneal stimulation disturbs the normal homeostatic balance between reflex tear stimulation and the ocular surface, and interrupts the neural stimulation of the lacrimal gland, which in turn decreases tear production.1,32,38,39 Recent evidence on the induction of a contact lens-induced inflammatory state on the ocular surface includes demonstration of inflammatory cytokines in the tear film of contact lens wearers,40 complement deposition on the surface of contact lenses,41 mononuclear leukocyte recruitment in soft contact lens wearers,41 and expression of inflammatory markers HLA-DR and CD23 on conjunctival epithelial cells of contact lens wearers.42 Contact lenses are also known to cause a reduction in blink frequency and intensity through a decrease in corneal sensitivity.6,43
Finally, evaporation continues to present an important factor in contact lens-related dry eye. Increased tear osmolarity may cause the ocular surface epithelial cells to release inflammatory cytokines to initiate the abnormal signaling in the ocular surface-lacrimal gland functional unit.1
♦ Diagnosis
Symptoms
Symptom assessment is a key component in the clinical diagnosis of contact lens-related dry eye, as with dry eye disease in general, and the diagnosis is very much a symptom-based diagnosis.22,44 The symptoms of dry eye in contact lens wearers have not been fully established, however, because these patients usually have a mild to moderate degree of dry eye.8,22,44,45
Dryness is the most frequent symptom of dry eye in contact lens-wearing patients.8,9,15,45,46 The sensation of dryness is actually complex, and symptoms of ocular dryness are often poorly defined and variable. Table 11-3 shows a list of common ocular symptoms of contact lens-related dry eye. In several studies performed among contact lens wearers, besides dryness, frequently reported symptoms include scratchiness or irritation, grittiness, blurry or changeable vision, ocular fatigue, discomfort, and soreness.9,15,27,46 In a Japanese study, blurry vision was the most frequent symptom.27
|
Even successful full-time contact lens wearers seem to have many dryness symptoms when questioned. In one study, among 83 successful full-time contact lens wearers, dryness was reported as the most frequent symptom (37%), followed by blurry or changeable vision (33%), light sensitivity (26%), scratchiness (26%), discomfort (19%), and soreness (18%).8
Questionnaires are important screening and diagnostic instruments commonly used to detect dry eye in clinical practice and in large-scale epidemiological studies. The original McMonnies questionnaire assessing dry eye was later modified by Guillon et al20 to deal more specifically with contact lens wearers. The Contact Lens Dry Eye Questionnaire was developed to examine symptom distribution among contact lens wearers and focuses on ocular symptoms rather than the presumed risk factors for dry eye disease.8,9,20,28 All versions were reported to be fairly good and effective.8,9,28
In a study in which 502 soft contact lens wearers were evaluated by the Contact Lens Dry Eye Questionnaire, the researchers concluded that the question that best predicts dry eye symptoms without administration of a full questionnaire was that related to the incidence of ocular dryness. Other symptoms recommended to be questioned were scratchiness and burning.20
A shift toward increased severity of symptoms at the end of the contact lens-wearing time is frequently reported by contact lens wearers.8,9 Additionally, in contact lens wearers, several environmental conditions—such as video display terminal or computer use, air conditioning, atmospheric pollution, central heating, tobacco smoke, or vehicle exhaust fumes—may exacerbate symptoms of dryness.20,26,47–49 This problem was attributed to increased evaporation from the ocular surface. In computer visual syndrome, the increase in evaporation was reported to be secondary to factors such as decreased blink rate, warm air produced by the computer equipment, and a widening of the interpalpebral aperture because of raised viewing angle on the computer screen.26
Clinical Signs and Diagnostic Tests
In a situation similar to that in dry eye disease as a whole, no correlation has been yet established between typical subjective dry eye symptoms and objective clinical findings in patients with contact lens-related dry eye or in contact lens-wearing dry eye patients.8,9,50–52 This is probably due to the multifactorial nature of dryness in contact lens wearers.8,9,44,45,50–52 Although knowledge in the area of dry eye has grown over the past decade and efforts to outline a battery of diagnostic tests have been extended, the question of which diagnostic tests are most appropriate for research and clinical purposes remains controversial.22,44,45,53
Furthermore, tear tests that may be considered valid in diagnosis of dry eye may not be equally sensitive in prediction of dry eye problems in contact lens wearers as in the case of mild to moderate dry eye disease.34 It is not uncommon to find patients who have normal tear film breakup time (BUT) but who still complain of dryness when they wear contact lenses. Finally, although patient-reported symptoms are moderately repeatable from visit to visit, many of the procedures used clinically to diagnose and monitor dry eye disease are largely unrepeatable.53 Therefore, performing repeat measurements or examining the subject on more than one occasion has been recommended.53
Slit Lamp Examination
- ♦ A careful slit lamp examination—with and without contact lens—is important in diagnosis.
- ♦ The lids and lashes should be evaluated for the frequency and amplitude of blinks and the presence of blepharitis or meibomianitis. Lids should be everted and observed for the presence of tarsal papillae or staining.
- ♦ The height of the tear meniscus should be assessed.
- ♦ The quality of the tear film should be evaluated, and debris, mucus, and foam should be looked for in the preocular or prelens tear film.
- ♦ With the contact lens in place, surface cleanliness and wetting characteristics of the contact lens should be assessed, as well as the fitting characteristics.
Tear Film Breakup Time
After the contact lens is taken out, tear film stability can be measured with fluorescein tear film BUT (invasive) or non-invasively with the use of an interferometer or Tearscope Plus® (Keeler Instruments Inc., Broomall, PA). The Tearscope Plus® can be used to assess pre-lens tear film (pre-LTF) quality as well. Repeatability of fluorescein BUT was reported to be substantial and to increase when two-timed readings were averaged.53 The main problems with fluorescein BUT measurements are the invasive nature of the test and lack of control over the volume and concentration of fluorescein instilled.54,55 Accuracy and reproducibility of fluorescein BUT were reported to improve by using smaller volumes (1 to 2 μL) of fluorescein with either a laboratory micropipette or 1 μL fluorescein strips.56 With the Akorn Dry Eye Test, 97% of the BUT results were found to be within 3 seconds of each other.56,57
Ocular Surface Staining
Ocular surface staining should be evaluated with fluorescein, rose bengal, and lissamine green dyes. Common practice is fluorescein staining to evaluate corneal epithelial damage, together with either rose bengal or lissamine green staining to assess conjunctival epithelial status or mucin-deficient areas.58,59 In dry eye disease, interpalpebral superficial punctuate keratitis of varying intensity is frequently encountered.59 Conjunctival staining has been shown to be significantly more in soft contact lens wearers compared with nonwearers, and higher in patients with symptoms compared with those without.59
Assessment of Tear Volume
Tear volume can be assessed with Schirmer’s 1 and 2 tests, the phenol red test, or the self-prepared cotton thread test. Repeatability of Schirmer’s 1 and 2 tests has been shown to be more variable in mild to moderate dry eye disease,53 whereas another study reported that the sensitivity and specificity of the self-prepared cotton thread test were better than in the phenol red test for determining patients who will develop contact lens intolerance.34 As yet, however, none of these tests have been demonstrated to have accuracy as high as required to be used as a screening test.34 The tear meniscus height was reported to be a poor test for assessing tear volume because many variables other than tear volume might affect the height and shape of tear meniscus.60
Pre-Contact Lens Fitting Considerations
For a long time, dry eye has been considered a contraindication for contact lens fit. This is not exactly the case today, when different contact lens materials, multiple care solutions, and a variety of lubricant solutions are available. Not all patients need to be fitted with contact lenses either. To be able to weigh the advantages over the disadvantages and risks, diagnosis and, if possible, control of any tear film problem from the very beginning are critical.
Considering that contact lenses themselves disrupt the tear film, a dry eye sufferer from the beginning will surely experience acceleration of the onset of problems. Any potential contact lens wearer should be questioned about skin diseases, such as acne rosacea, and any systemic disease that may affect lacrimal output, such as rheumatoid arthritis or collagen vascular disease. Questioning should include any systemic drug use. Women should be questioned about regularity of menstrual cycles, menopause, and use of hormone replacement therapy or oral contraceptives. Patients should be asked about the presence of any of the common symptoms of dry eye, including feeling of dryness, scratchiness or irritation, grittiness, blurry or changeable vision, discomfort, light sensitivity, and burning, stinging, and soreness. If one or more of these problems are present, any change in symptoms during the day or with environmental alterations, prolonged reading, computer use, and TV watching should be investigated.
Blinking amplitude and frequency should be evaluated. Assessment of tear quantity and stability before fitting contact lenses is also crucial. Results of slit lamp examination, ocular surface staining, tear film BUT, and any tear volume assessment test described earlier—in combination with symptoms—would disclose patients who may become intolerant of contact lens wear. Patients with partial blinking characteristics are at risk, as are those with poor lid hygiene and obvious meibomian gland disease.
On the other hand, initially successful contact lens wearers with a healthy tear film may experience contact lens intolerance and contact lens-related dry eye in time, especially after 1 to 3 years of successful wear.15,41 Therefore, all patients fitted with contact lenses should be evaluated at regular intervals to identify early symptoms or signs of tear film or ocular surface problems that can lead to intolerance and contact lens dropout. Patients should be questioned about an increase in the severity of symptoms when they wear their contact lenses, as the day progresses, and with prolonged near work, computer use, or exposure to air conditioning, atmospheric pollution, central heating, tobacco smoke, or vehicle exhaust fumes (Table 11-4).26,61
|
♦ Differential Diagnosis
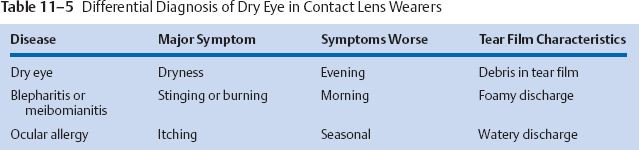
Table 11-5 shows the most common diseases that should be considered in the differential diagnosis of dry eye disease in contact lens wearers. Patients with chronic blepharitis (usually accompanied by meibomianitis) may also complain of dry eye symptoms. In these patients, a burning, stinging sensation may be more prominent than dryness, and the symptoms are usually worse in the morning. A close relationship has been reported between dry eye disease and all forms of blepharitis.1,62,63 Patients with one disease frequently suffer from the other also, and these subjects often have a vicious cycle of disease, with blepharitis, meibomian gland disease, and dry eye perpetuating each other.63 The chronic inflammation of blepharitis irritates the eye surface and inhibits tear production. The reduced tear flow does not wash inflammatory products away from lid margin, so they accumulate and create inflammation.
In staphylococcal and mixed staphylococcal-seborrheic blepharitis, Staphylococcus aureus has been isolated; in chronic blepharitis, coagulase-negative staphylococci, Propionibacterium acnes, Corynebacterium species, and S. aureus have been isolated.63 These bacteria can hydrolyze tear film lipid layer cholesterol esters and wax esters with their lipolytic exoenzymes. The disruption of the tear film lipid layer in blepharitis and meibomianitis often causes
increased evaporation and osmolarity that creates negative feedback on the ocular surface-lacrimal gland functional unit and leads to aqueous deficiency.64 On the other hand, decreased flushing action of tears and decreased washout of inflammatory mediators from the tear film in aqueous deficiency may aggravate inflammation and exacerbate symptoms and signs of blepharitis and meibomian gland disease.1
Rosacea is associated with both obstructive and seborrheic meibomian gland disease.63 Any patient with malar flushing of the cheeks and vascular changes in their facial skin should be considered to have rosacea. In these patients, the normal flora produces lipolytic enzymes that break down lipid molecules into individual components. The main components of meibomian gland secretions are cholesterol ester, wax ester, and triglyceride. Based on the analysis of an individual’s meibum, the associated clinical picture can be predicted.63
Diagnostic signs are variable but can include irregular, thickened, or hyperemic eyelid margins, a cloudy or inspissated secretion from meibomian glands on expression, irregular glandular dilatation, mild to moderate papillary hypertrophy, ocular surface staining most prominent in the inferior quadrants rather than interpalpebrally, chalazia, and foamy discharge into the tear film.63,65
Another condition that may coexist with or activate dry eye disease is ocular allergy.66,67 Whereas many patients with dry eye report eye itching, many contact lens patients have seasonal allergies and complain of ocular itching. In general, the accompanying symptoms and signs aid us in the differential diagnosis of dry eye versus allergy in contact lens patients. Itching is more prominent in ocular allergies and is often accompanied by a conjunctival papillary reaction, injection, and, possibly, chemosis and watery discharge. On the other hand, dry eye is usually a diagnosis of exclusion, and a papillary reaction and chemosis are generally absent.
The worst scenario is that the two conditions coexist in one patient. Whereas any sort of allergic inflammation, including giant papillary conjunctivitis, can create negative feedback on the ocular surface-lacrimal gland functional unit and decrease aqueous tear flow, aqueous deficiency can also lead to aggravation of allergic inflammation by delaying washout of vasoactive and inflammatory mediators.
The symptoms of giant papillary conjunctivitis are similar to both seasonal ocular allergy and solution sensitivity. Upper tarsal conjunctiva should be carefully examined in patients complaining of itching, mucous discharge, and recent contact lens intolerance, and any change in solution or chronic use of one solution should be questioned (Table 11-5).
Lid wiper epitheliopathy was recently described by Korb et al.68 It is characterized by staining with fluorescein, rose bengal, or both of that portion of marginal conjunctival epithelium that wipes the ocular surface. Eighty percent of contact lens wearers reporting symptoms indicative of dry eye within the first 4 hours of wearing their best-fit soft contact lenses displayed staining of the lid wiper as compared with 13% of contact lens wearers without symptoms. The authors proposed that a diagnosis of lid wiper epitheliopathy may explain the conundrum of patients with symptoms but no other clinically objective findings.
♦ Effects of Contact Lens Wear on the Tear Film and Ocular Surface
Although research on pathophysiological processes is continuing, an unstable tear film is known to be a common denominator among several conditions causing dry eye symptoms, ocular irritation, and contact lens intolerance.22
The true thickness of the preocular tear film remains controversial, with widely different published results.6,69–72 It is presumed to be less than 10 μm, however, and is reported to decrease to 4.5 μm between blinks.6 Therefore, the preocular tear film is relatively thin when compared with the thickness of any contact lens (minimum 30 μm, to an average of 60 to 120 μm, and more than 250 μm for lenses of considerable optical power). Moreover, tear volume is limited to 7 ± 2 μL, so the volume of tear fluid to physically cover or to hydrate contact lenses is limited.
The following major contact lens-induced changes have been documented in the tear film and ocular surface:
- ♦ All contact lenses divide the tear film into two compartments—pre-LTF and post-LTF. The pre-LTF is very unstable, if present, leading to increased evaporation, and the interchange of the post-LTF with habitual tear film is restricted.6,46,69–72
- ♦ The physical presence of the contact lens alters the tear menisci along the upper and lower lids,9 and creates a localized thinning of the tear film at its edge.73
- ♦ Contact lenses increase evaporation, with elevation of tear osmolarity and resultant dryness symptoms.1,21,33,38,74,75
- ♦ Stability of the tear film is disturbed, and frequent blinking is required for resurfacing.6 However, wearing of contact lenses may compromise blink frequency or blink amplitude.6,34
- ♦ Lid surface congruity is altered by all contact lenses.24
- ♦ All contact lenses prevent habitual, direct rubbing action of the lids on covered ocular surfaces, and thus interfere with physiological sloughing of the ocular surface epithelia, the clinical significance of which is unknown.6
- ♦ Corneal sensitivity is reduced by contact lens wear.1,13,36,37
- ♦ Initial insertion of a lens on an unadapted eye usually results in increased reflex tear secretion, with definitive changes in concentration of tear ingredients and a subsequent return to baseline.13,38,73–77
- ♦ Histopathological changes occur on the ocular surface, namely conjunctival squamous metaplasia,78,79 decrease in goblet cell density,78,79 and abnormal epithelial cell chromatin material.78,79
Effects of Contact Lenses on the Tear Film
A contact lens placed over the ocular surface disrupts the normal structure of the tear film and divides it into two layers; the pre-LTF and the post-LTF. The pre-LTF is approximately 3.7 μm thick as measured by interferometry,72 and it is thought to consist anteriorly of the superficial lipid layer, with a base layer that is more aqueous. The post-LTF thickness measurements range from 2 to 12 μm as measured by optical pachymetry,80 optical coherence tomography,81 interferometry,82 and three-dimensional in vivo confocal microscopy.83 This layer is thought to consist anteriorly of aqueous fluid, with a mucin gradient near the corneal epithelium. Although the major role of the pre-LTF is to provide comfort through lubrication and lens hydration, it also ensures a smooth surface for an optimal visual performance. On the other hand, the post-LTF provides lens movement and comfort through lubrication, ensures epithelial hydration and removal of debris and exfoliated cells, and has antimicrobial effects (Fig. 11-2).
The pre-LTF lipid layer is thin, if present at all,6,7,41,46,69–72 and this renders the pre-LTF rather unstable, leading to increased evaporation.7,35,41,84,85 Following evaporation of the pre-LTF, a soft contact lens may start to dehydrate and then absorb the post-LTF to rehydrate. Absorption of the post-LTF dries the eye, interferes with the interchange with habitual tear film, and desiccates the ocular surface. With an altered lipid layer, the lens continues to dehydrate, which exacerbates the cycle of tear evaporation and post-LTF depletion. Depletion of post-LTF, on the other hand, has been thought to be implicated in significant outcomes such as ocular surface desiccation,59,86–89 impairment in antimicrobial properties of tears,90 and accumulation of metabolites and inflammatory debris,35,88,91 leading to inflammatory or infectious complications.
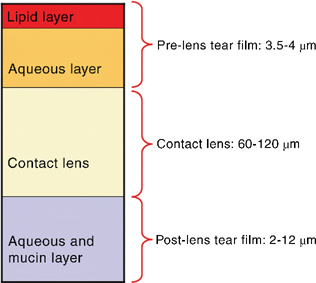
Figure 11-2 Tear film and contact lens relationship.
The post-LTF may be dependent on base curve and elasticity of contact lens (higher elasticity leading to pressure, drawing more tears), and vertical interpalpebral fissure width (small fissure associated with higher lid tension).91 Lens diameter is a significant factor that affects tear mixing; unfortunately, however, decreasing lens diameter also decreases comfort.88 Contact lens material has also been suggested to effect post-LTF elimination rate in some studies,88,92 whereas other studies have not found differences between hydrogel or silicone hydrogel contact lenses.72,82The post-LTF has been measured to be thick immediately after contact lens application, showed significant thinning during the next 30 minutes, and then was somewhat thicker for the rest of the lens-wearing period to reach a steady state.46 It is not clear, however, whether the post-LTF ever reaches a steady state or instead continues to thin, and studies provide preliminary evidence that the tear film thickness changes potentially over the course of the day for all contact lens wearers.46
The post-LTF thickness was shown to decrease within a few minutes following eye closure.88 Two factors that play roles in this reduction were suggested to be the downregulation of tear production during sleep93 and the mechanical pressure of the eyelid.88 It follows that the risk of inflammatory complications due to inadequate post-LTF mixing with decreased mediator washout would be especially higher with overnight wear, when the corneal epithelium is particularly vulnerable to adhesion by infectious agents.
Increased Evaporation by Contact Lenses
Individuals without objective signs of dry eye or subjective symptoms may experience classic dry eye disease while wearing contact lenses. Tomlinson et al94 were the first to attribute this to an increase in evaporation from the eye, which occurs with all contact lenses, analogous to dryness symptoms occurring in low humidity, excessive wind, and prolonged close-up visual activities resulting in less frequent blinking in non-contact lens wearers.
The preocular tear film lipid layer is internally layered. A thin polar lipid layer serves as surfactant between a thicker nonpolar hydrophobic lipid layer and the aqueous layer, and it impedes evaporation of the tear film.24 Structured as such, the lipid layer plays an important role in the stability of the tear film.95,96 It has been reported that when the lipid layer is absent or nonconfluent, the tear film is unstable and evaporation was suggested to increase fourfold.97
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree