Fig. 14.1
Cross-section illustration of suprachoroidal potential space between the sclera and the vascular choroid. Copyright JirehDesign, reproduced with permission
14.1.2 Choroidal Physiology
The choroid is highly vascularized and contains large capillaries that are 20–30 μm in diameter. It has been estimated that 70 % of the total blood supply to the eye is distributed to the choroid [21]. The choroidal circulation is designed to provide oxygen and metabolic support to the retina without obstructing vision at the fovea. Four to seven vortex veins provide venous drainage for the choroid [28]. Venous drainage and arterial supply are separated in the choroid, preventing thermal exchange between outgoing and incoming blood. This system suggests a role of the choroid as a temperature moderator for the neural retina.
The choroidal capillaries are fenestrated, allowing small and medium-sized molecules to traverse across. Intraocular pressure (IOP) opposes the outward osmotic pressure and maintains the steady state [2]. Under normal conditions, the albumin concentration of the interstitial space of the choroid is found to be less than 35 % of plasma [3].
The major arterial supply, together with the choriocapillaris, is functionally segmental with very little collateral flow [12]. This contributes to the pattern of large triangular lesions with the bases located anteriorly towards the equator if a vessel is occluded. Discrete lobular infarctions occur if a single end arteriole is blocked and can be associated with systemic hypertension, toxemia of pregnancy, disseminated intravascular coagulopathy, acute posterior multifocal placoid pigment epitheliopathy, giant cell arteritis, Goodpasture’s syndrome, and sickle cell anemia [28].
A conclusive relationship between glaucoma and the choroid has not been established. Numerous potential associations have been proposed, though studies have shown opposing results. Histologically, Yin et al. found a decrease in choroidal thickness in glaucomatous eyes when compared to eyes with optic atrophy of other causes and normal eyes [34]. Spraul et al. found increased choroidal thickness in eyes with a history of glaucoma compared to age-matched controls [31]. Of nine studies published using optical coherence tomography (OCT) measurements, six publications showed no significant difference between the macular choroidal thicknesses of glaucomatous eyes compared with controls [1, 14]. Choroid expansion may play a role in the anterior displacement of the lens in primary angle closure glaucoma according to Quigley [24].
14.2 Diagnosis
When choroidal effusions form, the abnormal accumulation of fluid in the suprachoroidal space can be seen as bullous, solid detachments, separated into quadrants [3]. The effusions usually appear as dome-shaped elevations in the posterior segment that are limited by fibrous adhesions concurrent with the vortex veins. Choroidal effusions may be associated with an exudative retinal detachment (Fig. 14.2). Funduscopic findings can usually differentiate a choroidal detachment from a retinal detachment, as choroidal detachments are solid dome-shaped elevation under the retina, which are relatively immobile, while retinal detachments are mobile detachments of the retina often with folds within the retina.
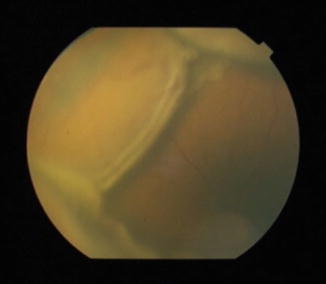
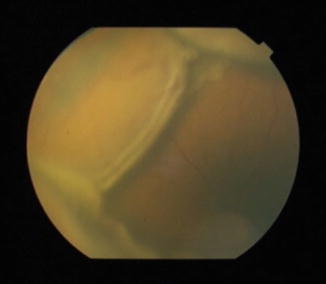
Fig. 14.2
Fundus photograph of choroidal effusions with associated exudative detachment
Ultrasonography can assist in the diagnosis of choroidals when there is a limited view of the posterior pole. B-scan ultrasonography will reveal dome-shaped elevations (Fig. 14.3) that do not cross from quadrant to quadrant [19]. Ultrasound imaging can also differentiate between serous effusions and hemorrhagic choroidals. Highly elevated choroidal detachments with opacities in the suprachoroidal space suggestive of clotted blood are typically noted with the hemorrhagic type. A-scan ultrasonography is also helpful and shows the steeply rising, double-peaked spike characteristic of choroidal effusion with lower reflective spikes from the clotted hemorrhage [5].
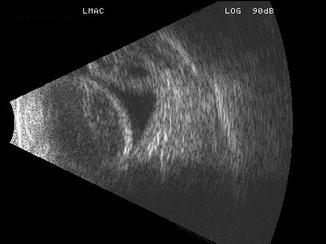
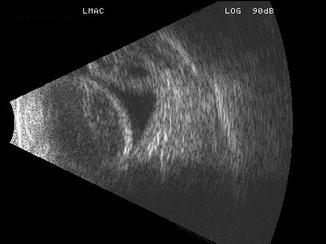
Fig. 14.3
Longitudinal sonographic section through the macula. Note the nasal and temporal bullous choroidal detachments which are not quite apposed to each other
Small and peripheral choroidal effusions are usually asymptomatic with minimal vision loss and/or discomfort. Larger effusions can cause decreased vision if the detachment involves the macula or if there is an anterior displacement of the lens-iris diaphragm causing a myopic shift [26]. Patients may notice an absolute scotoma corresponding to the site of the effusions. Sudden and severe pain with significant loss of vision is a feature of hemorrhagic choroidals. Hemorrhagic choroidals are often associated with headache, nausea and vomiting secondary to a sudden elevation in IOP [5].
14.3 Pathophysiology
The most common type of choroidal effusion is serous, with a protein concentration of approximately 67 % of serum protein. These effusions result from a decrease in IOP following intraocular surgery. This creates a pressure differential that allows small and medium-sized molecules, along with fluid, to traverse across the isoporous choroidal capillary membrane [2]. Normally when IOP is lowered, the hydrostatic pressure of the veins draining the choroid decreases and the hydrostatic pressure of choroid capillaries likely decreases, keeping the net hydrostatic pressure across capillary walls unchanged. However, with very low IOP or hypotony, the venous pressure outside of the eye limits venous pressure inside the eye so equilibrium shifts towards fluid accumulation. In addition, the pressure gradient across the sclera is decreased, so fluid from the suprachoroidal space through the emmisarial scleral openings is eggressed at a slower rate. Fluid begins to accumulate and spontaneous detachment of the choroid from its scleral attachments occurs. If bulk outflow decreases and colloid accumulates in the suprachoroidal space, fluid will enter the space even more rapidly [3]. Although the degree of the detachment correlates to the degree of hypotony, inflammation is also thought to be an important facilitator [29]. Inflammation augments the above process by increasing the rate of colloid movement into the suprachoroidal space. It increases the permeability of choroidal capillaries [26]. Inflammation can also contribute to hypotony possibly by a prostaglandin-mediated decrease in aqueous production combined with an increase in uveoscleral outflow [29].
Bellows et al. described an additional mechanism for intraoperative choroidal effusion that occurs in eyes with prominent episcleral vessels and high episcleral venous pressure, as in patients with a carotid-cavernous fistula or Sturge–Weber syndrome. These effusions have a protein concentration that is 18 % of the serum and thought to be due to a process of molecular sieving. The elevated venous pressure creates a magnified pressure differential when IOP drops to zero, promoting the filtration of larger proteins as fluids flows into the extravascular space [2].
14.4 Sequelae
Persistent large choroidal effusions can result in a flat anterior chamber with corneal decompensation and cataract progression. Choroidal effusions can also turn into the hemorrhagic type with stretching and breaking of the choroidal arteries. This sequence of events may be especially pronounced if the patient is on anticoagulant treatment. Risk factors for hemorrhagic choroidals include older age, a history of glaucoma, previous ocular surgery, and long or very short axial length [19]. Hemorrhagic choroidal detachment is usually associated with severe pain, a flat anterior chamber and high IOP [13]. Liquefaction of the hemorrhage must be considered before attempting drainage. B-scan echography can be used to follow progression of clot lysis that can take a variable amount of time [5]. Large “kissing” choroidals with prolonged retinal apposition may sometimes lead to retinal adherence and secondary retinal detachment, so earlier intervention is more highly considered in this scenario.
14.5 Etiology
14.5.1 Postoperative
The most common cause of choroidal effusions is intraocular surgery with the lowering of IOP. Intraoperative and postoperative hypotony with the inflammation associated with surgery is the proposed etiology with the pathophysiology previously discussed [3]. Associated risk factors for postoperative choroidals include systemic hypertension, older age, prior vitrectomy, nanophthalmos, and elevated episcleral venous pressure [19]. Effusions are commonly observed after panretinal photocoagulation [9]. The number of laser applications and increasing retinal surface treatment area are positively correlated with the development of effusions. Shorter eyes are also at higher risk. Self-limited choroidal effusions are often observed after scleral buckling procedures. The fluid accumulation is thought to be the result of compromised venous outflow at the vortex veins. Risk factors include the size of the buckle and its posterior location [22]. Choroidal effusions can also be found preoperatively in the setting of a rhegmatogenous retinal detachment. Several studies have found poor prognosis for these hypotonous eyes with a retinal detachment and choroidal effusions [29].
14.5.2 Inflammatory
Choroidal effusion can also be primarily associated with inflammatory disorders affecting the posterior pole, such as scleritis and Vogt–Koyanagi–Harada syndrome [15]. Orbital inflammation can also lead to choroidal effusions that are thought to be related to an associated scleritis as well as congestion of the orbital cavity. Treatment of the underlying disease process with control of inflammation usually leads to reabsorption of the fluid.
14.5.3 Medical
Systemic medications such as sulfonamides, tetracycline, diuretics, topiramate and selective serotonin reuptake inhibitors have been reported to be associated with nonsurgical-related choroidal effusions. Discontinuation of the offending medication aids in the resolution of the effusion [26]. The intraoperative use of antifibrotic agents such as mitomycin-C or aqueous suppressants such as timolol or dorzolamide after trabeculectomy may be associated with prolonged hypotony and choroidal effusions [26].
14.5.4 Uveal Effusion Syndrome
Uveal effusion syndrome (UES) is a diagnosis of exclusion that is used to describe cases of uveal effusion with unknown etiology. It is characterized by uveal effusion and serous retinal detachment. UES can be distinguished from other causes of uveal effusion by normal IOP and the lack of significant inflammation. There are several proposed hypotheses for the pathogenesis of UES, with the most likely being reduced scleral protein permeability. It is felt to be related to scleral thickening and poor fluid outflow. UES is more common in males and generally follows a relapsing-remitting clinical course. Most patients with UES have bilateral involvement at some point in the disease process [7].
14.5.5 Choroidal Tumors
Primary or metastatic tumor, such as melanoma, may be associated with serous choroidal detachment. B-scan ultrasonograhy and transillumination may be helpful if tumor is suspected. Primary cancers that may metastasize to the choroid include breast, lung, prostate, kidney, gastrointestinal tract, lymphoma, and leukemia.
14.6 Medical Treatment
Suprachoroidal effusions are usually self-limited and resolve with supportive medical treatment. Resolution is generally expected within a few weeks if the underlying etiology is successfully addressed [19]. Inflammation should be aggressively treated with reversal of hypotony.
All patients with choroidal effusions are encouraged to avoid activities that increase venous pressure in the eye. Examples of such activities include lifting heavy objects, bending, coughing, and Valsalva maneuver. Any elevation in venous pressure increases the pressure differential and promotes movement of molecules and fluid into the suprachoroidal space. Increase in episcleral venous pressure also risks the rupture of these vessels and the occurrence of devastating hemorrhagic choroidals.
Cycloplegia with atropine 1 % or scopolamine 0.25 % is administered to relax an anteriorly rotated ciliary body and deepen a shallow anterior chamber [11]. The pupillary dilation with cycloplegic use also prevents posterior synechiae formation with a miotic pupil. Stabilization of the blood aqueous barrier is also thought to be a secondary action of these agents. Topical corticosteroids are the mainstay for control of inflammation. Frequent use of prednisolone acetate 1 % or difluprednate ophthalmic emulsification 0.05 % for a few weeks is recommended with dosing interval titrated to the inflammation present [11]. Peribulbar injections are effective for administration of steroids to the posterior segment. Sub-Tenon injection of triamcinolone acetonide has been shown to be effective in relieving inflammation in patients with scleritis before systemic corticosteroids take effect [18]. Systemic corticosteroids may be needed if local administration fails to control intraocular inflammation [8].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


