Disorders of the Orbit
David B. Lyon
PEDIATRIC ORBITAL DISORDERS have a diverse and complex spectrum and must be approached in an organized and disciplined manner to arrive at the best plan of evaluation, diagnosis, and treatment. The common orbital diseases in childhood overlap little with those found in adults. An initial differential diagnosis should be formulated based on the history and physical examination, and it is helpful to classify the disease process based on features of inflammation, infiltration, mass effect, or vascular changes. Clues about the dynamics and location of the disease process may come from evaluation of the motor and sensory nerve effects and the presence or absence of pain. Pain is caused by a rapid increase of mass or pressure effect such as that seen with infection, inflammation or hemorrhage, or from bone or nerve involvement. Neoplasms rarely cause pain until late in their course.
The time progression of the disease process is also important to establish since some processes occur in minutes (hemorrhage), hours to days (rhabdomyosarcoma, thyroid eye disease [TED], neuroblastoma, granulocytic sarcoma, inflammation, or infection), weeks to months (chronic inflammatory conditions, benign neoplasm, or lymphoma), or months to years (dermoid, neurogenic tumors, fibrous dysplasia). Sometimes it is difficult for the patient or family to remember the exact onset of symptoms, and old photos can be helpful in establishing the time of onset and progression of the disease process. Any past ocular, medical, and family history should be obtained. Systemic investigation may be important in the assessment of the patient since endocrinologic, infectious, immunologic, vascular, and neoplastic diseases may have orbital involvement. Imaging techniques may be employed to best define the lesion as to location, composition, contour, vascularity, and effect on the adjacent orbital structures such as compression and infiltration. Many patients will require an orbitotomy for a diagnostic biopsy or removal of the lesion.
ORBITAL ANATOMY
The orbit is delineated by portions of seven of the bones of the face and skull; is surrounded by the brain, paranasal sinuses, and soft tissues of the face; and contains the globe, optic nerve, motor and sensory nerves, extraocular muscles, connective tissue, fat, glandular structures, and blood vessels. Any of these anatomic structures may be involved in a disease process or give rise to a primary orbital neoplasm.
In adults, the orbit is pyramidal in shape with a total volume of 30 mL. The orbital roof is triangular and composed of the frontal bone and lesser wing of the sphenoid and contains the optic canal. The lateral wall, which is at a 45-degree angle to the medial wall, is composed of the greater wing of the sphenoid and the zygomatic bones. The thinner medial wall is composed of the maxillary, lacrimal, ethmoid, and lesser wings of the sphenoid bones. Finally, the orbital floor, which is also triangular in shape, is made up of the maxillary, zygomatic, and palatine bones. The growth of the orbit is complete sometime between 7 years of age and puberty. Loss of an eye before this time may retard orbital bony development.
The optic canal and superior orbital fissure are in the orbital apex and transmit the optic nerve and ophthalmic artery, and cranial nerves III, IV, V-1, and VI. From their origin in the orbital apex at the annulus of Zinn, the extraocular muscles course anteriorly to insert on the globe in the anterior orbit, except the inferior oblique which has its origin at the medial anterior orbital floor. From the posterior sclera, the orbital portion of the optic nerve resides inside the muscle cone and exits the orbit via the optic canal. For descriptive purposes, the retrobulbar orbital is separated into intraconal and extraconal spaces. The lacrimal gland resides in the superotemporal anterior orbit and the lacrimal drainage apparatus is in the medial anterior orbit.
Paraorbital structures include the anterior cranial fossa superiorly and the paranasal sinuses. The ethmoid sinuses are located medially and are present at birth. Superior to the anterior orbit is the frontal sinus that is rarely well developed before 9 years of age. The maxillary sinus lies inferior to the orbit and expands during childhood with a resulting change in the orbital floor configuration.
ORBITAL EXAMINATION
Evaluation of orbital disease in children should include a complete ocular examination with special attention to
inspection, palpation, and documentation of eyelid and globe position. Optic nerve function should be evaluated and followed with best-corrected visual acuity, color vision, pupillary function, visual fields, and optic disk appearance. The status and function of the cranial nerves, corneal and facial sensation, and facial tone and symmetry should be evaluated. Photographic documentation of all abnormalities is helpful at baseline and follow-up exams to evaluate for interval changes of the disease process. Photos should also be taken preoperatively on surgical cases.
inspection, palpation, and documentation of eyelid and globe position. Optic nerve function should be evaluated and followed with best-corrected visual acuity, color vision, pupillary function, visual fields, and optic disk appearance. The status and function of the cranial nerves, corneal and facial sensation, and facial tone and symmetry should be evaluated. Photographic documentation of all abnormalities is helpful at baseline and follow-up exams to evaluate for interval changes of the disease process. Photos should also be taken preoperatively on surgical cases.
Proptosis, or axial globe displacement, is one of the main indicators of orbital disease. Thus, all patients need Hertel exophthalmometer readings to determine if proptosis is present and to quantitate the globe position relative to the lateral orbital rim. The orbit is surrounded by bone, except anteriorly, so that any increase in volume from a mass, infection, or inflammation may result in the displacement of the globe anteriorly, with asymmetry measuring more than 2 mm being significant. Evaluation of globe dystopia vertically or horizontally also helps determine the location of the mass within the orbit. An orbital mass not centered within the orbit will displace the globe off its axis in a direction away from the mass. Intraconal processes usually cause axial proptosis, as seen with optic nerve glioma or TED. Inferomedial displacement can result from superotemporal lesions such as dermoid cysts and lacrimal gland tumors. Lateral displacement can result from medial subperiosteal abscesses (SPAs).
The orbital rims and quadrants should be palpated for masses. If a mass is noted, document its location, size, shape, tenderness, consistency, discreteness, and mobility. Resistance to retropulsion of the globe, compared with the fellow side, may indicate a posterior or apex process that is not palpable. The preauricular and submandibular lymph nodes should also be evaluated with palpation.
Orbital processes can affect ocular motility, either by direct involvement of the muscles or their motor nerves, or by deviation of the axis of the eye. Inflammatory processes often cause pain with eye movements, especially when the muscles or nerves are directly involved.
Pulsation may be secondary to a vascular malformation in the orbit or the absence of orbital bone that allows the transmission of brain pulsation to the orbit as sometimes seen with an encephalocele, surgical removal of the orbital roof, or with absence of the sphenoid wing in some cases of neurofibromatosis. If the flow through an orbital vascular lesion is high, you may hear a bruit or feel a thrill, as with carotid cavernous fistulae, larger dural arteriovenous fistulae, and orbital arteriovenous malformations. Venous lesions of the orbit do not pulsate, but may enlarge with the valsalva maneuver or with the head held in a dependent position.
Evaluation of the visual pathways includes examination of best-corrected visual acuity, color vision, red desaturation, visual fields, and pupillary reactions. All these factors can assist in the detection of visual loss due to an orbital process. Loss of color vision and an afferent pupillary defect are often the first signs of early visual loss. Changes in the size of the pupil can be seen with tumors that invade or compress the parasympathetic (third cranial nerve and ciliary ganglion) or sympathetic fibers that innervate the pupillary muscles. Optic nerve head edema or atrophy helps to determine the duration of the process. Retinal or choroidal striae or folds may be seen from a mass pressing on the globe.
ORBITAL IMAGING
Orbital imaging provides diagnostic information with increased specificity as to the location, character, and size of an orbital lesion. Computed tomography (CT) and magnetic resonance imaging (MRI) are the most commonly used modalities.
CT is utilized in the evaluation of orbital trauma, orbital cellulitis, screening for mass-occupying lesions, and for processes that may involve bone. Spiral CT produces higher quality images with good spatial resolution, faster scanning times (a few minutes per patient), and less expense than MRI scans. The addition of contrast material gives further information regarding the lesion and enhances vascular structures. However, concern of cancer induction from radiation exposure in children is real, and adherence to the as low as reasonably achievable policy of the US Food and Drug Administration is recommended (1).
MRI yields an excellent view of the optic nerve and visual pathways, orbital apex, orbitocranial junction, brain, organic foreign bodies, vascular tumors, or heterogeneous tumors. Fat suppression with gadolinium can be used to enhance orbital structures or processes. With this technique, the normally bright orbital fat will appear dark, allowing visualization of orbital structures and processes such as vascular tumors or inflammation. The advantages of MRI over CT scanning include no radiation exposure, no need for contrast material to visualize vascular structures, and better contrast resolution of soft tissues. The disadvantages of MRI include long acquisition time, sensitivity to motion artifact, possible need for sedation and anesthesia support, higher cost, and decreased spatial resolution. MRI is contraindicated in patients with metallic foreign bodies, metallic clips, or any ferromagnetic material in the area being examined.
Ultrasonography has a complementary role in pediatric orbital disease. Its advantages are no radiation exposure, no contrast needed, readily available, noninvasive, and no sedation required. Useful information regarding the location, size, shape, tissue characteristics, and vascular features of orbital lesions can be obtained. Color Doppler echography will quantitate flow velocity of vascular lesions. Poor resolution around the bone at the orbital apex makes this form of testing less useful. However, it is particularly helpful in identifying lesions adjacent to and involving the globe, such as scleritis and vascular and cystic lesions (2).
Rarely, arteriography is used to study arterial lesions such as aneurysms and arteriovenous malformations. Selective injection, magnification, and subtraction techniques
increase visualization of the lesion. CT angiography and magnetic resonance angiography allow noninvasive visualization of large- and medium-sized vessels of the arterial system, but do not provide the fine detail possible with direct angiography.
increase visualization of the lesion. CT angiography and magnetic resonance angiography allow noninvasive visualization of large- and medium-sized vessels of the arterial system, but do not provide the fine detail possible with direct angiography.
CONGENITAL ABNORMALITIES OF THE ORBIT
Anophthalmos and Microphthalmos
Anophthalmia and microphthalmia refer to the absence of an eye and the presence of a small eye within the orbit, respectively, and represent a spectrum of maldevelopment resulting from failure of the primary optic vesicle to fully develop during the fourth week of embryologic development. Both anophthalmia and microphthalmia are usually bilateral and occur as part of genetic syndromes in 75% of cases with variable phenotype. The remaining cases are usually due to maternal viral infections or ingestions of teratogens. Isolated nonsyndromic heritable unilateral cases are very rare (3).
In true anophthalmos, the orbits and eyelids are usually normally formed, but small. The conjunctival fornices are decreased in size, and the eye cannot be seen or felt in the orbit on palpation. Histologically, no ocular tissue is present. Extraocular muscles may be present and well developed. Infants with true bilateral anophthalmos show an absence of the chiasm, small geniculate bodies, and small optic foramina. Clinical anophthalmos refers to the condition of no visible or palpable globe without radiographic or histopathologic confirmation of true anophthalmos.
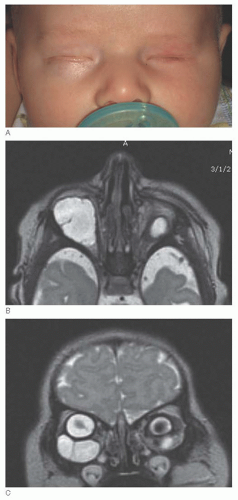
Isolated microphthalmos is usually a unilateral condition that occurs sporadically. The size of the eye is variable and there is sometimes functional vision if it is not too severe. If a coloboma exists, due to failure of closure of the embryonic fissure, microphthalmos may be associated with an orbital cyst that consists of an inner layer of primitive neuroretinal tissue that may contain retinal structures, photoreceptor differentiation, or rosette formation, and an outer layer continuous with the sclera with vascularized connective tissue and occasional cartilage. The size of the cyst varies and often is beneficial for stimulating normal growth of the orbital bone and eyelids. B-scan ultrasonography, CT, or MRI establish the diagnosis, demonstrating a round or irregular cystic lesion adjacent to the microphthalmic globe (Fig. 18.1). Occasionally, the cyst can enlarge greatly, obscuring the microphthalmic globe and expanding the orbit. Management is individualized and may include observation, cyst aspiration or excision, cyst excision with enucleation, and prosthesis fitting with or without surgery (4).
Since both anophthalmos and microphthalmos may be associated with hypoplastic orbits and small eyelids, the goal of treatment is expansion of the eyelids, socket, and bony orbit. Progressively enlarging conformers, fit by an ocularist, are used to expand the eyelids and conjunctival fornices. Clear conformers may be utilized if a microphthalmic eye may have visual potential. When satisfactory expansion has occurred, an ocular prosthesis can be fabricated. Tissue expanders can be placed in the orbit and progressively expanded to enlarge the hypoplastic orbit to then allow for orbital implant placement for
volume augmentation (5). Dermis-fat grafting is another option for volume enhancement with the added advantages of expanding the socket conjunctival surface area and potential for growth with the child.
volume augmentation (5). Dermis-fat grafting is another option for volume enhancement with the added advantages of expanding the socket conjunctival surface area and potential for growth with the child.
Cryptophthalmos
Cryptophthalmos is a rare congenital anomaly, usually bilateral, in which the eyelids are fused to the globe. It may be divided into several grades with and without upper eyelid coloboma (6). In complete cryptophthalmos, the eyelids are absent and the globe is entirely covered by skin extending from the brow to the cheek. In partial cryptophthalmos, the medial eyelid is replaced with a layer of skin fused to the globe, but the lateral portion of the eyelid is normal in structure and function. There is partial or complete absence of the eyebrow, eyelids, eyelashes, and conjunctiva with continuation of the forehead skin to the cheek over the eyes. The hidden eye is usually abnormal, with a wide variety of ocular defects. The partially developed adnexa are fused to the anterior segment of the globe. These defects are thought to result from failure of the eyelid fold formation, which normally occurs in the seventh week of gestation. This condition is often associated with multiple congenital deformities such as cleft palate, syndactyly, dental malformations, nasal deformities, urogenital deformities, and hypoplasia of the facial and orbital bones. Histologically, the eyelids are abnormal with absent conjunctiva and diminished or absent orbicularis and levator muscles, tarsal plate, and meibomian glands, making attempts at reconstruction difficult.
ORBITAL INFECTIONS
Orbital infections range from preseptal cellulitis to orbital abscesses. It is extremely important to know the features of these infections and their proper treatment to avoid visual loss or spread of infection to the cavernous sinus or intracranial structures. Infections occur from three primary sources: direct spread from an adjacent sinus (most common); direct inoculation from trauma, surgical or nonsurgical, or skin infection; and hematogenous spread from a distant focus.
Preseptal Cellulitis
Preseptal cellulitis is an infection of the periorbital soft tissues anterior to the orbital septum and thus is not a true orbital infection. However, it may be difficult to distinguish from orbital cellulitis or may spread to involve the postseptal orbital tissues. It is more common than orbital cellulitis in children and is characterized by eyelid erythema and edema, generally more pronounced in the upper eyelid. If the cellulitis is severe, some chemosis may also be present. Staphylococcal and streptococcal organisms are the main pathogens for which antibiotic coverage is required today, including methicillin-resistant strains of Staphylococcus aureus (MRSA). Children with preseptal cellulitis often have a history of antecedent upper respiratory tract infections, recent eyelid trauma, insect bites, or infections. Oral antibiotics and close observation are the treatment of choice.
Clinical evaluation, sometimes supplemented with CT scanning, is the best method to distinguish preseptal from orbital cellulitis. Proptosis and decreased motility herald orbital cellulitis. Chemosis is a less specific finding. On CT scan, preseptal cellulitis shows soft-tissue edema or abscess formation anterior to the orbital septum, whereas orbital cellulitis shows involvement of the postseptal orbital tissues. This differentiation, however, is usually made clinically. Rapid progression of preseptal cellulitis to orbital cellulitis can occur, and therefore, patients should be followed closely, and admitted for intravenous antibiotics and imaging if the clinical picture deteriorates.
Orbital Cellulitis
Orbital cellulitis requires prompt identification and treatment to prevent visual or life-threatening complications. It is more common in children than in adults, but it is usually related to sinusitis in both. Orbital extension from the ethmoid sinus is most likely, but any or all of the sinuses may be involved. Upper respiratory tract infections interfere with clearance of secretions by the respiratory cilia, causing poor sinus drainage and predisposing children to sinusitis. The bones separating the orbit and sinuses are thin, allowing spread of the infection. The foramina, especially the ethmoid foramina, and the valveless interconnecting venous system of the orbit and sinuses represent other routes for possible spread of infection from the sinuses to the orbit. Other causes of orbital cellulitis are traumatic and surgical wounds, foreign bodies, or spread from odontogenic infections, dacryoadenitis, panophthalmitis, dacryocystitis, or endogenous septicemia. Immunosuppressed children can develop fungal orbital cellulitis, which is often fatal, and present with fever and neutropenia and mild symptoms (7).
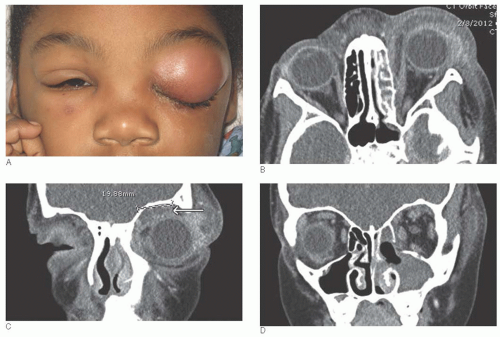
Signs of orbital cellulitis include eyelid edema, pain, decreased motility, proptosis, chemosis, decreased vision, orbital tension, and headache (Fig. 18.2A). Decreased vision, an afferent pupillary defect, or dilated pupil indicate involvement of the orbital apex and require aggressive treatment. Delayed treatment may result in an orbital apex syndrome, cavernous sinus thrombosis, possible blindness due to apical optic nerve compression, cranial nerve palsies, brain abscess, and even death. Permanent visual loss can also result from direct optic neuritis or vasculitis. Spread via the vascular emissaries to the cavernous sinus can lead to cavernous sinus thrombosis, and spread through the diploic vessels to the intracranial cavity can lead to subdural empyema or intracranial abscesses. The recent medical history is usually positive for an upper respiratory tract infection, but the symptoms may be mild. The child is sick, lethargic, tired, and often febrile, which helps to differentiate this from orbital inflammatory disease. CT or MRI scans show orbital
involvement by soft-tissue edema, proptosis, fat stranding, phlegmon, and possible intraorbital abscess which may vary in location and extent. They also reveal the accompanying sinus infection, which helps to secure the diagnosis of infection in most cases (Fig. 18.2B-D).
involvement by soft-tissue edema, proptosis, fat stranding, phlegmon, and possible intraorbital abscess which may vary in location and extent. They also reveal the accompanying sinus infection, which helps to secure the diagnosis of infection in most cases (Fig. 18.2B-D).
In contrast to adults, the pathogens in orbital cellulitis in young children tend to be single aerobic organisms, including streptococcal and staphylococcal species. Other grampositive and gram-negative organisms are possible causes. If foul smelling, anaerobic infections should be considered, especially if the wound has been contaminated by soil and bites. Before the introduction of the HiB vaccine in 1985, Haemophilus influenzae was the most common pathogen isolated in patients with orbital cellulitis. Antibiotic treatment should be targeted to cover the most likely infecting organisms, again including MRSA. Since the disease process can threaten vision and life, high-dose intravenous antibiotics and nasal decongestants must be used.
Due to the delay in development of the sinuses in children, the most frequent locus of the disease is the ethmoidal sinus. Since the sinuses are the primary site of infection, and the orbit is a bystander, surgical sinus drainage by otolaryngology is often indicated. Close monitoring of vision, pupillary reaction, extraocular motility, and central nervous system (CNS) function must be carried out during the first 24 to 48 hours. If there is no evidence of improvement or if the condition worsens, an orbital or subperiosteal abscess should be considered and looked for with repeat imaging. Abscesses within the orbital soft tissues can extend posteriorly, resulting in life-threatening consequences such as cavernous sinus thrombosis, meningitis, and intracranial abscesses. Third, fourth, fifth (V-1), and sixth cranial nerve dysfunction may occur in septic cavernous sinus thrombosis. Systemic signs of toxicity are present, including sepsis, nausea, vomiting, meningeal signs, and altered levels of consciousness. When an abscess of the orbit or brain is identified, it requires immediate drainage to prevent serious complications.
Subperiosteal Abscess
An SPA or infiltrate occurs when purulent material elevates the periorbita away from the bony walls of the orbit adjacent to an infected sinus. On CT scan, the periorbita is tethered at the orbital suture lines so the abscess creates a smooth, dome-shaped elevation of the periorbita with either a homogeneous or heterogeneous collection (Fig. 18.2C). The signs are similar to those of orbital cellulitis, but may also include nonaxial displacement and deformation of the globe. Initial treatment is with broad-spectrum intravenous antibiotics, based on the age of the child, to obtain adequate drug levels in the relatively avascular subperiosteal space. Garcia and Harris outlined the criteria for initial nonsurgical management based on the absence of the following surgical indicators: age of patient, 9 years or older; presence of frontal sinusitis; nonmedial location of SPA; large SPA; suspicion of anaerobic subperiosteal infection (e.g., presence of gas within the abscess space as visualized on CT scan); recurrence of SPA after previous drainage; evidence of chronic sinusitis (e.g., nasal polyps); acute optic nerve or retinal compromise; infection of dental origin, because the presence of anaerobes would be anticipated (8). These criteria are built on an earlier microbiologic study that found negative or single aerobic organisms on cultures of drained material in children less than 9 years old, more severe infections in those 10 to 14 years old, and positive cultures at drainage, even after 3 days of usually appropriate antibiotics, which were often polymicrobial including anaerobes in those 15 and older (9).
Although these guidelines are helpful, each child has to be individually managed in conjunction with otolaryngology. If there is a poor response to antibiotics after 24 to 48 hours, or if there is a threat to the optic nerve, retinal function, suspicion of anaerobic infection, or very tense orbit with significant pain, drainage and culture is indicated either via orbitotomy or endoscopic sinus surgery with orbital drainage. If sinus surgery is being performed, despite the lack of clear criteria for SPA drainage, it is wise to include its drainage if feasible. Large SPAs, now defined as 2 cm or larger in greatest dimension or greater than 1,250 mm3, or that extend along the orbital roof or floor from the ethmoid, or those associated with frontal sinusitis or intracranial complications should be drained promptly (10,11). Sinus infections of dental origin also constitute an indication for surgical intervention because the presence of anaerobes is anticipated. Decisions should be based on the clinical course as improvement on serial CT scans may lag. The use of intravenous corticosteroids may also be beneficial for treatment of the sinusitis and SPA (12).
Dacryoadenitis
Dacryoadenitis, or lacrimal gland inflammation, may be infectious. It is most often viral in nature, occasionally bacterial, and very rare in children. It presents with an inflamed, tender lacrimal gland that is palpable through an edematous upper eyelid. The child may have adenopathy, fever, malaise, and leukocytosis. Since the orbital lobe of the gland is postseptal, infectious dacryoadenitis is a localized form of orbital cellulitis. CT scan shows diffuse lacrimal gland swelling without bony defects. It usually improves spontaneously, and since there is generally no bacterial involvement, antibiotics are rarely indicated. Systemic steroids frequently help accelerate resolution of the process and keep the patient more comfortable. Infectious dacryoadenitis may be difficult to distinguish from the more common idiopathic lacrimal gland inflammation. The presence of preauricular adenopathy makes a diagnosis of viral dacryoadenitis more likely. Other infectious causes include mononucleosis, herpes zoster, mumps, trachoma, syphilis, and tuberculosis.
ORBITAL INFLAMMATION
Thyroid Eye Disease
TED is an inflammatory orbital disorder associated with autoimmune thyroid dysfunction, most commonly Graves’ disease. It is the most common cause of orbital inflammation in adults with manifestations that vary from mild to severe and may cause significant pain and disfigurement, visual disability, and blindness. Pediatric TED is uncommon, but occurs in up to 30% of children with Graves’ disease, especially in teenagers when the incidence of primary and second-hand smoke exposure increases. Like in adults, there is a female predominance. Antithyroid medications are usually the first line of treatment in pediatric Graves’ disease and thyroidectomy is uncommon. Available studies suggest that childhood TED is less severe than in adults, with eyelid retraction and proptosis as the predominant eye changes (Fig. 18.3), whereas the more severe manifestations of restrictive myopathy and optic dysfunction almost never occur in children (13,14,15). Most children require no treatment or supportive treatment of exposure keratitis only with ocular lubricants. Severe inflammation is rare, and thus oral corticosteroids are
seldom used. Orbital decompression, extraocular muscle, and eyelid surgery are very infrequently needed.
seldom used. Orbital decompression, extraocular muscle, and eyelid surgery are very infrequently needed.
Idiopathic Orbital Inflammation
Idiopathic orbital inflammation (IOI) is described histologically as a pleomorphic inflammatory cellular response and fibrovascular tissue reaction without known cause. IOI is rare in children and is a diagnosis of exclusion, accepted after ruling out other known causes of orbital inflammation such as orbital cellulitis, Langerhans cell histiocytosis (LCH), sarcoidosis, TED, Wegener’s granulomatosis, or lymphoproliferative disorders. The character of presentation and temporal sequence help to form the essential diagnostic framework for orbital inflammation. Classically, IOI presents acutely or subacutely with signs of inflammation (pain, swelling, and redness), whereas chronic inflammation from granulomatous disease often presents with a mass effect or chronic bony destruction.
IOI is a multifaceted disease with a wide spectrum of clinical, radiologic, and histopathologic presentations. Many classification schemes have been applied based on location of the inflammatory process, histopathologic characteristics, and stage of inflammation. However, the most useful classification is by the anatomic site of involvement: dacryoadenitis, myositis, sclerotenonitis, diffuse anterior inflammation, perioptic neuritis, or the superior orbital fissure and cavernous sinus syndrome of Tolosa-Hunt.
The inflammatory process is typically characterized by an abrupt onset of pain, proptosis, and inflammatory signs and symptoms, such as swelling and erythema, depending on the location and degree of inflammation, fibrosis, and mass effect. Pediatric IOI differs from the adult presentation by an increased incidence of bilateral involvement and may have associated headache, fever, vomiting, abdominal pain, lethargy, and eosinophilia. The IOI syndromes are initially managed with systemic corticosteroids, with biopsy reserved for cases that are atypical, poorly responsive to treatment, or steroid dependent.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree