Diseases of the External Ear: Introduction
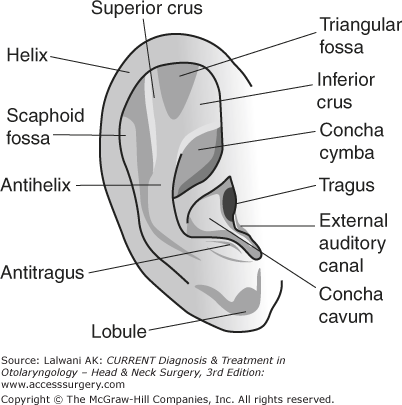
The pinnae of the external ear are cartilaginous frames that aid in focusing and localizing sound. Each pinna is anchored to the cranium by skin, cartilage, auricular muscles, and extrinsic ligaments. The anatomy of the pinna is illustrated in Figure 47–1.
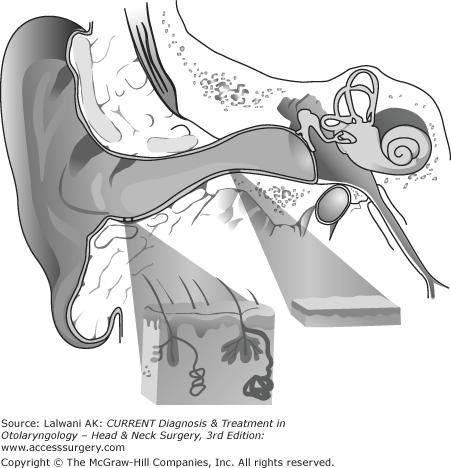
The external auditory canal (EAC) is typically 24 mm in length with a volume of 1–2 mL. The lateral third of the canal is made of fibrocartilage, whereas the medial two thirds are osseous. During early childhood, the canal is straight, but takes on an “S” shape by the age of 9. The EAC has an important relationship with the mastoid segment of the facial nerve, which lies posterior to the EAC as it descends toward the stylomastoid foramen. The temporomandibular joint is anterior to the EAC, and disease processes affecting this joint may lead to otalgia.
The EAC is lined by stratified squamous epithelium that is continuous with the skin of the pinna and the epithelial covering of the tympanic membrane. The subcutaneous layer of the cartilaginous portion of the canal contains hair follicles, sebaceous glands, and ceruminous glands, and is up to 1 mm thick. The skin of the osseous canal does not have subcutaneous elements and is only 0.2 mm thick (Figure 47–2). The epithelium of the EAC migrates laterally, allowing the canal to remain unobstructed by debris. The rate of epithelial migration is 0.07 mm/d and is thought to occur at the basal cell layer.
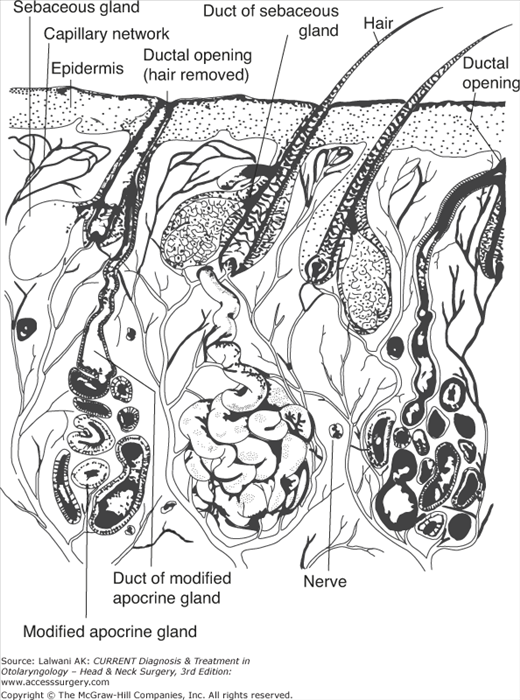
The ceruminous glands are modified apocrine sweat glands surrounded by myoepithelial cells; they are organized into apopilosebaceous units (Figure 47–3). Cerumen prevents canal maceration, has antibacterial properties, and has a normally acidic pH, all of which contribute to an antibacterial effect of cerumen.
The pinna is innervated laterally, inferiorly, and posteriorly by the great auricular nerve (cervical plexus). Arnold’s nerve (a branch of the vagus nerve) innervates the inferior bony canal, the posterosuperior cartilaginous canal, and corresponding segments of the tympanic membrane and the cymba concha. The posterosuperior bony EAC is innervated by branches of the facial nerve. The auriculotemporal branch of V3 supplies the anterior portion of the pinna. The glossopharyngeal nerve contribution to the external ear is not well delineated.
The anterior and superior wall of the EAC and tragus are drained by preauricular lymph nodes. The infraauricular lymph nodes drain the helix and the inferior wall of the EAC, whereas the concha and antihelix are drained by the mastoid nodes.
The posterior auricular artery and the superficial temporal artery arise from the external carotid artery and supply the auricle and lateral EAC. The deep auricular branch of the maxillary artery supplies more medial aspects of the canal and the external surface of the tympanic membrane. The posterior auricular and superficial temporal veins drain the external ear.
The external ear aids in the efficient transmission of sound to the tympanic membrane by serving as a functional resonator and, in particular, boosts transmission in the speech frequencies.
The hairs in the lateral canal, as well as the depth and tortuosity of the EAC, protect the tympanic membrane and structures of the middle ear.
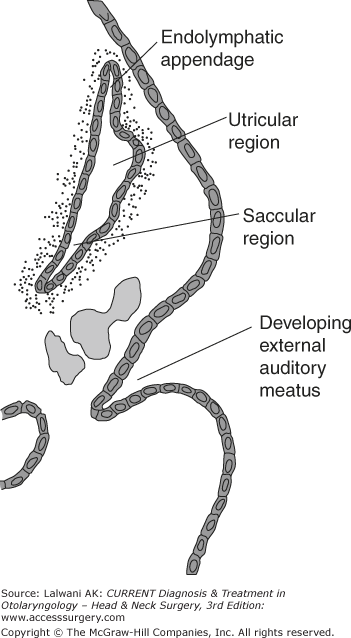
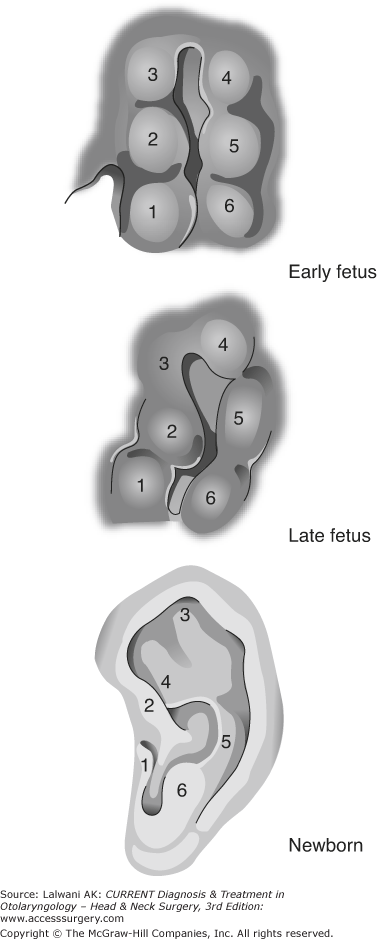
The mammalian ear is divided into external, middle, and inner ear components, which differ in their embryologic origin (Figure 47–4). The external ear consists of the pinna, the EAC, and the tympanic membrane, and is embryologically derived from the first and second branchial arches, and includes both ectodermal and mesodermal components. The mesenchymal tissue of the arches is composed of paraxial mesoderm and neural crest cells. The pinna is formed by gradual change in shape and fusion of components of the six auricular hillocks, which are derived from the first and second branchial arches (Figure 47–5). The formation of the external auditory meatus results from an ingrowth of a solid epithelial plate of ectodermal cells, the meatal plug, which eventually resorbs with only the lining of the canal remaining. The canal is lined by epithelial cells of ectodermal origin. The tympanic membrane begins to develop during the 28th week of gestation and arises from the most medial aspect of the meatal plug, which eventually becomes the external layer of the tympanic membrane.
Congenital Anomalies of the External Ear
Congenital anomalies of the external ear include a spectrum of malformations of the pinna as well as varying degrees of atresia and stenosis of the EAC. The causes of these disorders may be genetic or secondary to environmental exposures. These disorders include variants of microtia, lop ear, cup ear, Stahl’s ear, cryptotia, and prominent ear. Patient evaluation requires a thorough head and neck examination to exclude additional congenital anomalies. The list of associated syndromes is extensive and includes Goldenhar (hemifacial microsomia), branchio-oto-renal, Treacher Collins, and Robinow syndromes.
Multiple genes may have redundant roles in outer ear formation, which can account for phenotypically similar malformations. The sequence of such dysregulation is only beginning to be understood with the help of murine knock-out and knock-in models. The auricular hillocks that give rise to the pinna arise during the sixth week of embryogenesis, whereas the inner two thirds of the EAC are not formed until the 26th week. Untoward events throughout this period could give rise to structural anomalies of the external ear.
Patients typically present at birth with obvious auricular malformations. Several classification systems are used to further subcategorize this entity, one of which is detailed below.
The ear exhibits mild deformity, typically with a slightly dysmorphic helix and antihelix. This group includes low-set ears, lop ears, cupped ears, and mildly constricted ears. All major structures of the external ear are present to some degree. The lop ear is characterized by inferiorly angled positioning of the auricular cartilage and poor development of the antihelical fold, whereas the cup ear protrudes with a deep conchal bowl.
All pinna structures are present, but tissue deficiency and significant deformity exist.
Also known as, classic microtia or peanut ear, type III microtia has few or no recognizable landmarks of the auricle. The ear lobule is usually present and anteriorly positioned. This subgroup includes anotia, which is complete absence of the external ear.
Classically, microtia has been treated by a multistage auricular reconstruction. Patients undergo observation until the age of five to allow for growth of rib cartilage, which is harvested for reconstruction, and the development of the contralateral ear. This approach offers the benefit of reconstruction with autogenous material, which ultimately requires little or no maintenance. However, it is difficult to achieve a perfect cosmetic result. Typically, reconstruction occurs in four stages.
Rib graft is typically harvested from the chondrosis of ribs 6, 7, and 8. The goals of this stage include symmetry in the position of the reconstructed cartilaginous ear framework with the normal ear. Postoperatively, the patient must be assessed for pneumothorax, which may arise with rib harvest.
This procedure should be performed 2–3 months after Stage-I reconstruction and aligns the lobule with the reconstructed cartilage framework.
A postauricular sulcus is created to allow the ear to project away from the mastoid. This step should be performed 3 months after Stage-II reconstruction. Skin for the creation of the sulcus may be harvested from the groin, lower abdomen, buttocks, contralateral postauricular sulcus, or back.
This should be performed several months after Stage-III reconstruction.
Another option for reconstruction includes the placement of a prosthesis. This can be either glued on or anchored to bone. If the patient selects a bone-anchored prosthesis rather than auricular reconstruction, he/she must be aware that daily maintenance is required and that the anchor may compromise the vascularity of the surgical site, complicating future reconstructive surgery if the patient becomes dissatisfied with the prosthesis. A prosthesis does offer the advantage of a minor surgical procedure and allows for auricular replacement at an earlier age than surgical reconstruction. Complications of all types of auricular reconstructions include infection, hematoma formation, skin-flap necrosis, scar contracture, and poor contouring.
An increase in the distance from the helical rim to the mastoid is thought to be due to a lack of the antihelical fold and prominence of the conchal bowl. Ideal distance has been described as 15–20 mm with an ideal angle of 30°. Greater than 45° angulation is considered abnormal. This entity is most frequently bilateral.
Otoplasty is the mainstay of treatment for protruding ears. Often used techniques include recreating the antihelical fold utilizing 2–4 horizontal mattress sutures through the cartilage and anterior perichondrium (Mustarde technique). Stiff cartilage may require additional contouring. Conchal excess may be treated by removal of soft tissue and skin from the postauricular sulcus followed by concha-to-mastoid sutures at the fossa triangularis, cavum concha, and cymba concha.
Excessive overcorrection of the middle third of the ear should be avoided to prevent development of the “telephone ear” deformity. Hematoma is the most common complication following otoplasty occurring in approximately 3% of cases. Lack of patient satisfaction, although not a true complication, is not an uncommon occurrence as loss of up to 40% of correction has been reported.
Congenital anomalies of the EAC range from mild stenosis to complete atresia. These are often seen in association with malformations of the pinna and the structures of the middle ear. A canal cholesteatoma can develop in the face of severe EAC stenosis, and may also occur with epithelial rests left behind the atresia plate.
Audiologic evaluation via behavioral or electrophysiologic measures should be performed to confirm normal hearing in the contralateral ear in unilateral disease, and to assess for ipsilateral sensorineural hearing loss. The typical pattern of hearing loss in affected ears is a conductive hearing loss of 50–70 dB. Axial and coronal computed tomography (CT) scans are essential in the evaluation of patients with canal atresia or stenosis. CT scanning assesses for ossicular, facial nerve, and otic capsule abnormalities as well as for the degree of temporal bone pneumatization. In addition, CT scanning can be used to identify a cholesteatoma that would necessitate earlier surgical intervention.
A discussion on reconstruction for aural atresia can be found in Chapter 48, Congenital Disorders of the Middle Ear.
External Ear Trauma
The external ear is subject to a wide variety of injuries. All trauma patients require appropriate stabilization and triage of associated injuries based on their severity. Adherence to basic surgical principles and wound care prevents complications and improves the likelihood of a successful outcome.
- History of auricular trauma
- Edematous, fluctuant, and ecchymotic pinna with loss of normal cartilaginous landmarks
- Early diagnosis and treatment necessary to minimize cosmetic deformity.
Auricular hematoma refers to the accumulation of blood in the subperichondrial space, usually secondary to blunt trauma.
Cartilage lacks its own blood supply and instead relies on the vascularity of the perichondrium via diffusion. Shearing forces secondary to blunt trauma to the pinna lead to an accumulation of blood in the subperichondrial space. This creates a barrier for diffusion between the cartilage and the perichondrial vascularity, leading to necrosis of the cartilage and predisposing it to infection and further injury.
A patient with an auricular hematoma usually presents with an edematous, fluctuant, and ecchymotic pinna, with loss of the normal cartilaginous landmarks. Failure to evacuate the hematoma may lead to infection and/or cartilage necrosis and permanent disfigurement known as “cauliflower ear.”
The evacuation of hematomas can be performed using a skin incision parallel with the natural auricular skin folds. The irrigation of evacuated hematomas with topical antibiotics reduces the likelihood of infection. Splinting after drainage prevents the reaccumulation of hematomas, and options include cotton bolsters, plaster molds, silicon putty, and water-resistant thermoplastic splints. Through-and-through whip-type absorbable mattress sutures without a bolster have also been described.
Sharp or severe blunt trauma may lead to laceration or avulsion of the auricle. The expeditious repair and prevention of infection are essential. Auricular lacerations should be cleansed and débrided prior to repair. Simple lacerations can be closed primarily, whereas extensive injuries with tissue loss may require undermining, flap reconstruction, or tissue grafts. In the case of a near-total ear avulsion still attached to the helical root, the ear can be successfully reattached as the supply of the upper auricular-helical artery seems to be sufficient for the entire ear. Leech therapy may be required to support venous outflow until neovascularization occurs. Repairs should be covered with pressure dressings to prevent edema and hematoma formation, and cartilage-penetrating antibiotics such as quinolones should be prescribed. Excellent cosmetic results can be achieved, even with extensive lacerations.
- Otalgia, otorrhea, pruritus, hearing loss, history of water exposure
- In severe cases in which edema occludes ear canal, wick is critical to maintain EAC and permit antibiotic drops to reach infected tissues
- Cases in which erythema and tenderness extend outside of EAC require oral antibiotics with antipseudomonal activity.
Otitis externa is an inflammatory and infectious process of the EAC. Pseudomonas aeruginosa and Staphylococcus aureus are the most commonly isolated organisms. Less commonly isolated organisms include Proteus species, Staphylococcus epidermidis, diphtheroids, and Escherichiacoli. Fungal otitis externa is discussed in the next section.
In the preinflammatory stage, the ear is exposed to predisposing factors, including heat, humidity, maceration, the absence of cerumen, and an alkaline pH. Loss of acidity has been shown to be proportionate to the degree of infection. This can cause edema of the stratum corneum and occlusion of the apopilosebaceous units. In the inflammatory stage, bacterial overgrowth ensues, with progressive edema and intensified pain. Incomplete resolution or persistent inflammation for more than 3 months refers to the chronic inflammatory stage.
Symptoms of otitis externa may vary, depending on the stage and extent of disease. The clinical diagnosis is suggested by the presence of otalgia, otorrhea, aural fullness, pruritus, tenderness to palpation, and varying degrees of occlusion of the EAC. The patient may also present with hearing loss, which results from occlusion of the EAC by edema and debris. Signs of otitis externa include pain on distraction of the pinna, EAC erythema, edema, otorrhea, crusting, and, in more advanced disease, lymphadenopathy of the periauricular and anterior cervical lymph nodes. Skin changes of cellulitis may be present as well. In the chronic stage, the skin of the EAC may be thickened. A culture may be helpful for infections that are refractory to treatment.
Treatment for otitis externa involves meticulous atraumatic debridement of the EAC with the help of a microscope. Analgesia can be achieved with nonsteroidal antiinflammatory drugs (NSAIDs), opioids, or topical steroid preparations. After cleansing is complete, otic drop preparations that are antiseptic, acidifying, or antibiotic (or any combination of these) should be used. These have been shown to be equally effective in the management of uncomplicated otitis externa in a recent Cochrane review. If the degree of stenosis of the canal is severe, a wick must be placed in an effort to stent open the EAC and permit delivery of drops to the medial portion of the canal.
Available antiseptic preparations include acetic and boric acids, ichthammol, phenol, aluminum acetate, gentian violet, thymol, thimerosal (eg, Merthiolate), cresylate, and alcohol. Available antibiotic preparations include ofloxacin, ciprofloxacin, colistin, polymyxin B, neomycin, chloramphenicol, gentamicin, and tobramycin. Polymyxin B and neomycin preparations are often used in combination for the treatment of Saureus and P aeruginosa
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree