Diabetes and the Eye
Stephen S. Feman
Kevin J. Blinder
Diabetes mellitus is an important cause of visual loss in most parts of the world. In the United States, diabetes has been the leading cause of visual loss among people older than 20 years for most of the past century.1,2 The available data implies that the number of people in this country with diabetes mellitus is increasing.
In 2010 it was estimated that there were more than 100 million people in the world with diabetes mellitus.3 In the United States, in the year 2002, there were 18.2 million people (6.3% of the US population) with that disease.4 However, by December 2011 diabetes was reported to affect 25.8 million Americans (8.3% of the population).5
In general, this disorder is divided into two major types. Type I (often described as insulin-dependent diabetes mellitus) had been called “juvenile-onset diabetes” in the past; it is characterized by an immediate need for insulin at the time of diagnosis. This variety involves almost 10% of American diabetics.4 However, most Americans with diabetes have type II or non-insulin-dependent diabetes; that disorder had been described previously as “adult-onset diabetes.” A problem exists because diabetes mellitus includes many other varieties with different onset patterns and medication needs. For this reason, the classic type I/type II distinction tends to blur in clinical practice. An examination of the features that separate one variety of diabetes mellitus from another is beyond the scope of this chapter. Nevertheless, it is important to be aware that several diverse disorders appear to be included within the generic name “diabetes mellitus.” These disorders share a common feature because all are associated with abnormalities of glucose metabolism. Because of this historical relationship the ocular manifestations of diabetes mellitus were described, originally, as if they were just different aspects of one disease. That may be true, but it is important to be aware that some investigators believe these disorders represent different disease processes brought together only because they share a common final pathway.
In general, type I diabetes mellitus has its highest occurrence rate in the Scandinavian countries. There is a distribution gradient across Europe of a decreasing incidence of insulin-dependent diabetes among children younger than 16 years that starts in Finland (30 new cases per year for every 100,000 children younger than age 16) and becomes reduced as one approaches the Mediterranean coast of Italy (5 new cases per year per 100,000). The one exception is a “hot spot” on the island of Sardinia.6
In contrast, type II diabetes has a different worldwide distribution. Type II diabetes is found most often among certain indigenous peoples, such as the natives of the Nauru Islands in the Pacific Ocean and members of the Pima Nation of North America. In those two groups, the prevalence of type II diabetes approaches 50% of the adult population. A high peak is found among other Native American populations as well, but does not reach that encountered among the Pima.7
In the past, it was discovered that ≥10% of all individuals with diabetes mellitus developed some visual impairment within 15 years of diagnosis.8 In the United States in 1980, it was found that about 8% of the individuals who were legally blind had diabetes described as the primary cause of blindness.9 In 2002, the US National Health Interview Survey found visual impairment in 23.5% of diabetics older than age 50.10
RISK FACTORS FOR DIABETIC RETINOPATHY
In many studies, retinopathy has been used as a “marker” to identify the presence of diabetic eye disease. With statistical analyses similar to the geographic studies described above, certain inheritable human leukocyte antigens (HLAs) have been discovered that may be related to the risk of developing diabetic retinopathy. For example, in type I diabetes mellitus the presence of HLA-DR-4 in the absence of HLA-DR-3 increases the risk of developing proliferative diabetic retinopathy (PDR) by a factor of 5.4.11
The duration of diabetes, age of patient, and patient age at the time of diabetes onset have all been found to be related to the development of retinopathy.12,13 In patients with type I diabetes, retinopathy was infrequent (found in <8% of patients) for the first 3 years after diagnosis. However, after 20 or more years of type I diabetes, 99% had some form of retinopathy, and after 30 years of diabetes, more than 50% of these people developed PDR. In comparison, for patients with type II diabetes, at 3 years from the time of diagnosis, almost 23% had some retinopathy, and 2% of them had PDR. However, after 20 years or more of diabetes, fewer type II patients were found to have any form of retinopathy (60%) or proliferative retinopathy (5%) than the type I patients.12,13
The relationship of blood pressure to diabetic retinopathy remains uncertain. Although studies in the past implied no direct relationship, recent reports indicate that when diastolic blood pressures are routinely elevated, diabetic retinopathy is stimulated to develop and progress.14 The United Kingdom Prospective Diabetes Study found that 8 years of tight blood pressure control was able to reduce the rate of progression of diabetic eye disease.15
Other studies have inferred that elevated serum lipid levels may be associated with progressive visual loss. The Early Treatment Diabetic Retinopathy Study (ETDRS) found a statistically significant relationship between the presence of “hard exudates” in the macula and increased serum levels of lipoproteins and/or cholesterol.16 Over a 5-year interval, a statistically significant visual acuity loss was found to be associated with the severity of “hard exudates” in the macula.16
Hyperglycemia is the most important risk factor for the development and progression of diabetic retinopathy. The Diabetes Control and Complications Trial (DCCT) determined that intensive medical therapy, with the goal of maintaining glucose levels within the normal range, could prevent and/or slow the progression of diabetic retinopathy in type I diabetes mellitus patients.17 Similar features were discovered for type II diabetes patients in a series of studies performed in the United Kingdom.18
PATHOGENIC MECHANISMS IN DIABETIC EyE DISEASE
There are many theories regarding the pathogenic mechanisms that lead to the development of diabetic eye disorders. Those that are most popular at this time are related to abnormalities of (1) advanced glycation end products (AGEs), (2) aldose reductase activity, (3) glycosylated hemoglobin, and (4) protein kinase C (PKC).19 In general, these mechanisms result in a relative tissue hypoxia, and that may be the final common pathway to diabetic eye disease.
AGE production relates to the nonenzymatic reaction of glucose with the lysine residues of protein. Repeated and/or continuously high levels of serum glucose are necessary to produce this type of glucose-protein linkage. The resulting chemical compounds rearrange and transform themselves into irreversible structures called Amadori products. When proteins with Amadori products combine, they form AGEs. Increased levels of AGEs cause biologically active molecules to produce microvascular changes identical to the features found in diabetic retinopathy. Aminoguanidines are one class of agents that were found to inhibit AGE formation in animal studies. Because aminoguanidines can prevent and reverse early microvascular abnormalities in experimental animals, in theory they can influence human diabetic retinopathy.20,21 Whether this will be true in long-term human clinical studies is a subject of great interest.
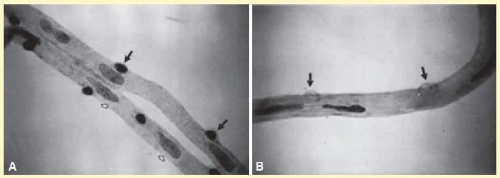
In the presence of high concentrations of sugar, aldose reductase enzymes convert sugar to alcohol. Certain cells, such as the pericytes and the endothelial cells of the retinal blood vessels, are known to have high concentrations of this enzyme. For this reason, in the presence of high levels of blood sugar, alcohols are formed within the pericytes and endothelial cells. An increase in the intracellular concentration of these alcohols can result in the death of those cells. In histopathologic studies, this type of cell death has been described as one of the first stages in the development of diabetic retinopathy22 (Fig. 20.1). The enzyme, aldose reductase, as well as the cellular aftereffects of its activity, have been implicated in many of the ocular problems associated with diabetes mellitus.23 Several different kinds of medications have been developed to inhibit the ocular effects of this enzyme. They have worked well in experimental animal studies. However, clinical trials imply that such agents are not suitable for long-term continuous use in humans.24,25
As indicated previously, the DCCT found a relationship between increased glycosylated hemoglobin levels and the development and/or progression of diabetic retinopathy. Because hemoglobin is continuously produced in the bone marrow, elevated blood sugar levels at the time of hemoglobin production result in increased levels of glucose-bound hemoglobin. Oxygen cannot become free from glycosylated hemoglobin as easily as it can from hemoglobin that is not glycosylated. Lengthy intervals of hyperglycemia result in more glycosylated hemoglobin in circulation. Whenever there is excess glycosylated hemoglobin, there is less tissue oxygenation and a relative tissue hypoxia develops. That tissue hypoxia may be the final common pathway for the development of diabetic retinopathy. The DCCT studies found that maintaining a glycosylated hemoglobin level at 7 or less can delay the development of diabetic retinopathy and/or slow the progression of this disorder when it is present.17,26 Current theories imply that the relative hypoxia associated with elevated glycosylated hemoglobin levels stimulates vascular endothelial growth factor (VEGF) production.27 This may be another feature related to the development of diabetic retinopathy.
PKC is an enzyme found in the eye and many other tissues. It is activated by hyperglycemia. PKC influences retinal blood flow by stimulating angiotensin; however, in addition, it increases vascular permeability, enhances the activity of growth factors (e.g., VEGF), and stimulates the adhesion of leukocytes to the endothelium of blood vessels.28 The ability of oral agents to inhibit the intraocular forms of PKC has been the subject of much recent clinical research. Several reports indicate that there may be an important role for such agents in the prevention and/or management of diabetic retinopathy in the future.29,30
The hemodynamic effect of an oral agent that is a PKC inhibitor was investigated in a double-masked, placebocontrolled, parallel, randomized study. This documented its bioavailability to the retinal vessels and its ability to ameliorate diabetes-induced retinal hemodynamic abnormalities in people with diabetes.31
The PKC-DRS group described the results of the PKC β-inhibitor, ruboxistaurin, when used in a large population, double-masked, multicenter, randomized, placebocontrolled study. Patients with moderately severe-to-very severe nonproliferative diabetic retinopathy (NPDR) received ruboxistaurin versus placebo for 3 or more years. Ruboxistaurin was well tolerated and reduced the risk of moderate visual loss, but had little effect on retinopathy progression.32 However, others have demonstrated that ruboxistaurin can reduce retinal vascular leakage in eyes that had severe leakage associated with diabetic macular edema (DME).33
THE CORNEA
Although diabetic patients have been known for many years to develop decreased corneal sensitivity,34 it was not until recently that the clinical significance of corneal disorders in diabetes mellitus patients became well established.35 However, whether diabetic corneal neuropathy is just a manifestation of a widespread diabetic neuropathy, or whether it exists as a distinct entity itself, remains unknown. Multiple studies36 examined this and their results remain equivocal.
The morphologic changes that develop in a diabetic patient’s corneal epithelial cells are well known. These include polymorphism, polymegathism, irregular cellular distribution, and stunting of surface cell microvilli.37 In diabetes mellitus, changes in the thickness and composition of the basement membranes occur throughout the body, as well as in the cornea. For this reason, it is not surprising that corneal epithelial basement membrane thickening and other tissue structural abnormalities have been described in the eyes of diabetic patients.38 The epithelial barrier function may be altered in the cornea of diabetic patients. The corneal epithelial zonulae serve as a diffusion barrier,39 and the corneal epithelial permeability is increased by a factor of about 5 in diabetics.40
In addition to these corneal epithelial problems, the corneal endothelium has an increased incidence of dysfunction in patients with diabetes.41 Similarly to the features described previously, there are changes in endothelial cell morphology in such patients. The corneal endothelium normally consists of a monolayer of cells arranged in a regular hexagonal pattern. In diabetes, there is inadequate cell volume regulation associated with cytoskeletal abnormalities. Computer-assisted morphometric analysis has found quantitative changes in cell variation (polymegathism) and cell shape variations (pleomorphism).42 As a result, there are diabetic-related morphologic changes in Descemet’s membrane that influence the success rate of corneal surgery.43 Because of these changes, there is great concern regarding refractive surgery in diabetic patients. Reports imply that the rate of refractive surgical complications is 50% higher than the norm in diabetics.44 Although diabetes mellitus has not been examined as a specific factor in refractive surgery studies, most investigations have excluded patients with systemic diseases that influence corneal healing.45 For this reason, many physicians consider diabetes mellitus to be a contraindication for such procedures.46
GLAUCOMA IN DIABETES MELLITUS PATIENTS
The relationship of diabetes mellitus and chronic openangle glaucoma has been uncertain. This had been because different scientific publications did not use the same features to characterize diabetes mellitus and/or chronic open-angle glaucoma. However, studies that have used abnormal glycosylated hemoglobin levels to establish a definition of diabetes mellitus, and a combination of visual field and optic nerve abnormalities as a method of describing glaucoma, discovered a relationship of diabetes mellitus to chronic open-angle glaucoma. In epidemiologic studies that used such criteria, chronic open-angle glaucoma was found twice as often in type II diabetic patients when compared with age-matched nondiabetic populations.47,48,49
The greatest visual threat to patients who have both glaucoma and diabetes is the development of neovascular glaucoma. More than 50 years ago, it was hypothesized that ischemic retinal tissue released a diffusable angiogenic substance that stimulated neovascularization.50 Recently, it was found that VEGF is an agent that satisfies this description.51 It has been discovered that significantly higher VEGF levels occur in the ocular fluids of patients with PDR when compared with patients without that disorder. Extremely elevated levels of VEGF were found in the ocular fluids of patients with neovascular glaucoma.
The clinical course of neovascular glaucoma can be divided into several stages.52 In the “prerubeosis stage,” there is no evidence of clinically detectable new vessel formation in the iris or anterior chamber angle; however, there is PDR in the posterior portion of the eye. In the “preglaucoma stage (rubeosis iridis),” new vessels are visible by clinical exam on the iris or in the anterior chamber angle. These vessels are seen, most often, in the peripupillary region first. Although the anterior chamber angle is open in these patients, vessels can be seen taking a direct path across the peripheral iris-ciliary body band, and scleral spur, at this stage. The next stage is the “open-angle glaucoma stage.” In this situation, there are increased vessels on the iris stroma. By gonioscopy, the anterior chamber angle still appears open, although there are increased numbers of new vessels in the angle. At this stage, a fibrovascular membrane develops that covers the iris and grows into the anterior chamber angle to inhibit aqueous outflow. The final stage of this disorder is the “angle closure glaucoma stage.” In this stage, the fibrovascular membrane contracts to produce changes on the iris and anterior chamber angle. The peripheral iris is pulled forward to create a partial or total peripheral anterior synechia. This synechial closure of the anterior chamber angle results in an intraocular pressure elevation.
The management of this disorder is related to the stage of the disease. In the prerubeosis stage, treatment of the underlying PDR by panretinal photocoagulation can cause regression of the abnormality. The rubeosis iridis stage is treated, again, by panretinal photocoagulation for the underlying diabetic retinopathy. In those cases where panretinal photocoagulation is not possible, panretinal cryoablation, or endophotocoagulation, is a reasonable alternative. For patients in the open-angle stage, it is necessary to first treat the elevated intraocular pressure. This should be attempted with medications and, after the pressure is brought to a normal level, panretinal photocoagulation needs to be applied. If the anterior segment neovascularization can be eliminated with panretinal photocoagulation, such patients are good candidates for filtration surgery. For patients in the angle closure stage, the first therapy should be to alleviate pain and reduce intraocular pressure. Panretinal photocoagulation remains the primary operation of choice, even at this late stage. At this time, such treatment will reduce the amount of anterior segment neovascularization. In some cases, filtration can be done after that. However, these patients often need implant drainage surgery.53
LENS CHANGES IN DIABETES MELLITUS PATIENTS
Diabetes mellitus is a frequent cause of transient variations in refractive error. This most often appears related to osmotic alterations within the crystalline lens. These changes develop from elevated serum sugar levels. Hyperglycemia results in elevated glucose levels in the aqueous fluid. This glucose can enter the lens by diffusion because a transport system is not needed for glucose to penetrate the lens capsule. The resulting incongruity of intralenticular, extracellular, and intracellular osmolality produces a complex balance. Variations in the index of refraction within the lens develop. Changes in lens hydration affect the lens capsule curvature and the magnifying power of the lens. For this reason, it is not uncommon for diabetics to request several eyeglass prescriptions and for each prescription to be unique for a specific time of the day. In those patients, a different refraction is needed for each serum sugar-level change.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree