Purpose
To report early complications of Descemet stripping automated endothelial keratoplasty (DSAEK) to treat late endothelial failure after penetrating keratoplasty (PK) using a specific surgical strategy.
Design
Retrospective analysis of a prospectively collected dataset.
Methods
All 17 eyes with a preoperative diagnosis of failed penetrating keratoplasty graft were identified out of a total pool of 793 eyes that had received DSAEK for endothelial dysfunction in a prospective Institutional Review Board–approved study of endothelial keratoplasty. A standard surgical strategy of careful slit-lamp examination and preoperative optical coherence tomography (OCT) to determine optimal DSAEK graft diameter was combined with undersized Descemet stripping and peripheral bed scraping.
Results
A total of 17 eyes in 16 patients were identified. The DSAEK graft size ranged from 7.0 to 8.0 mm, with all DSAEK graft diameters less than or equal to the PK diameter. The average follow-up was 16 months (range 2-38 months). All PK grafts cleared and the visual acuity improved in all patients. There were no cases of pupillary block or primary graft failure. There was 1 dislocation (5.9%). The dislocation occurred in an eye with aniridia, prior trabeculectomy, and scleromalacia with postoperative hypotony from a wound leak.
Conclusion
DSAEK for failed PK using DSAEK grafts with a diameter less than or equal to the PK diameter allowed improved vision with a low complication rate. Preoperative OCT of posterior PK contour can aid in graft diameter selection.
Failed grafts from prior penetrating keratoplasty (PK) have become an increasingly common indication for corneal transplantation. In 2008, 32 524 PKs were performed in the United States. Sixteen percent of these were regrafts. Each time a PK is repeated it has a successively higher likelihood of failure. After a repeat PK, the patient is once again subjected to prolonged visual recovery, potential for suture-related complications, unpredictable refractive result, and creation of an unstable full-thickness wound.
Endothelial keratoplasty (EK) has become the procedure of choice for primary endothelial failure from conditions such as Fuchs dystrophy and pseudophakic or aphakic bullous keratopathy. Price and Covert have also shown that it can also be a successful technique for rapid restoration of graft clarity in cases of late endothelial failure of prior PK. However, the complication rate after Descemet stripping automated endothelial keratoplasty (DSAEK) for failed PK has been reported to be much higher than in Fuchs dystrophy or pseudophakic bullous keratopathy eyes receiving DSAEK.
We have used EK to achieve a quick restoration of PK graft clarity, particularly in cases that had an acceptable refractive outcome with the initial graft. The purpose of this paper is to report on our early postoperative complications with DSAEK for failed PK. In addition, we describe our specific surgical strategy that we use to achieve our results.
Materials and Methods
Protocol
This study is a retrospective analysis of data from our institution’s ongoing prospective Institutional Review Board–approved study of endothelial keratoplasty. This study represents a retrospective analysis of 1 subgroup from that dataset.
This study reviews the early postoperative outcomes of 17 consecutive eyes treated with DSAEK for failed PK grafts from endothelial failure with minimal stromal opacities. The complications experienced in the study group of 17 eyes are compared to our previously published complication rates for DSAEK surgery using the same technique.
The inclusion criterion for the study group was all eyes with a prior standard PK graft that had failed because of immunologic or nonimmunologic endothelial failure. Patients were considered eligible for EK rather than repeat PK if they had enjoyed better best-corrected visual acuity prior to failure of their graft and the edema of the PK graft was felt to be responsible for the decrease in the visual acuity level. Patients were deemed to be poor candidates if they had good retinal potential but presented with significant stromal scarring or significant post-PK astigmatism that was not previously amenable to good visual correction with spectacles or contact lenses. These eyes received a repeat PK instead of an EK.
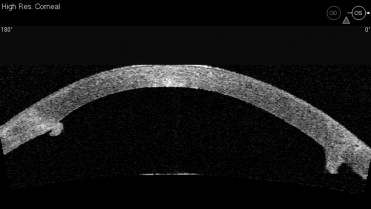
A careful slit-lamp examination was obtained in all patients preoperatively. An anterior segment Visante optical coherence tomography (OCT) (Carl Zeiss Meditec, Oberkochen, Germany) was obtained in 11 of 17 patients preoperatively. An OCT was not obtained preoperatively on the first 6 patients in this series as their surgeries occurred prior to obtaining the OCT equipment in 2007. The OCT was used to aid in determination of the optimal graft size. The selected graft size was either the same size as the PK or smaller for all cases in this series. A smaller graft size was selected when a significant PK graft-host interface posterior lip was identified on the preoperative slit-lamp examination or OCT ( Figure 1 ). Efforts were made to avoid any overlap of an EK button edge with an irregular protuberant posterior PK lip.
The specific outcomes assessed in this study included any intraoperative or immediate postoperative complications. The postoperative complications assessed included graft dislocation or decentration requiring intervention, iatrogenic primary graft failure (IPGF), pupillary block glaucoma, and iatrogenic PK wound dehiscence. The complication of IPGF was defined as any graft that had to be replaced with a new graft within 2 months of surgery. The complication of graft dislocation was defined as any transplant that required a subsequent injection of an air bubble to ensure adhesion. Performance of concurrent procedures such as cataract surgery, vitrectomy, iridoplasty, and secondary intraocular lens (IOL) insertion was also recorded. Patient records were also examined for ocular comorbidities such as prior glaucoma surgery, anterior chamber intraocular lens (ACIOL), or other anterior segment abnormality.
Surgical Procedure: Standard DSAEK Procedure
All DSAEK surgeries were performed with our standard technique as previously described. Videos of this technique have been shared and are available at our research website, dlek-dsek.com. Our surgical video titled “Descemet-Stripping Automated Endothelial Keraoplasty: Technique, Tips, and Ways to Prevent Dislocation” volume 21, from 2006, is also available at www.aao.scientificposters.com . (accessed July 2, 2010).
A 5-mm scleral tunnel incision is used for all of our DSAEK surgeries. Stripping of Descemet membrane with a reverse Terry-Sinskey hook (Bausch and Lomb Surgical, St. Louis, Missouri, USA) and scraping of the peripheral recipient bed with a Terry scraper (Bausch and Lomb Surgical) are performed using Healon (Abbot Medical Optics, Santa Ana, California, USA) for anterior chamber maintenance. After evacuation of all of the viscoelastic, attention is directed to preparation of the donor tissue. “Precut” tissue is used for all of the surgeries in this study and an operating microscope is used for all donor tissue manipulations. The donor cornea is placed endothelial side down on a lint-free surface. The wide scleral rim and corneal curvature prevent contact of the endothelium with the surface. The bed of resection is measured and confirmed to be of adequate size for trephination of the donor button. The peripheral gutter from the microkeratome cut is dried and marked with a gentian violet marker to ensure centration of the trephination. A centering mark is also placed on the epithelial cap. The tissue is trephinated to the desired size on a Teflon block, endothelial side up, using the prior marks for centration. After a strip of Healon is applied to the endothelium, the tissue is carefully folded in a 40/60 underfold configuration, taking care to avoid contact with the endothelium or any undue stretching forces in the folding process. The folded tissue is then grasped with Charlie insertion forceps (Bausch and Lomb Surgical) and quickly inserted into the anterior chamber with the stroma of the 60% side oriented anterior to the host cornea. Once inserted, the graft is unfolded with a combination of balanced salt solution (BSS) and air. The graft is then positioned and interface fluid removed with gentle external compression of the corneal surface with the Cindy Sweeper (Bausch and Lomb Surgical) with the anterior chamber completely filled with air. We do not routinely use stab “venting” incisions to remove interface fluid, and none were used in the study group. The main wound is sutured. The tissue is left undisturbed for 10 minutes to promote adherence. Dilating drops of cyclopentolate 1% and phenylephrine 2.5% are instilled at this time. After the 10 minutes has elapsed, nearly all of the intracameral air is exchanged with BSS. Finally, a 5- to 9-mm freely mobile air bubble is injected to support the graft postoperatively. The patient remains supine for 1 hour at the hospital and then as much as possible at home until the postoperative day 1 examination.
Surgical Procedure: Specific Surgical Strategies for DSAEK Under PK
Mild modifications of our DSAEK technique are made to minimize potential complications in post-PK eyes. Great care is taken to avoid any disruption of the posterior graft-host interface to avoid jeopardizing structural integrity of the PK wound. All stripping and scraping of the posterior corneal surface is completed central to the healed edge of the prior full-thickness graft. The graft size is also modified to ensure that it will fit inside the area of the prior PK and would avoid any posterior protuberance of the PK wound that may limit graft adherence. No other modifications are made to our basic technique.
Additionally, no changes are made regarding the parameters of the donor tissue. We accept donor tissue with a central endothelial cell density (ECD) greater than 2000 cells/mm 2 , any age between 4 and 75 years old, and death-to-transplantation time of up to 12 days. The same tissue parameters apply to both our EK grafts and our full-thickness PK surgeries.
Results
The study group was composed of 17 eyes of 16 patients that underwent DSAEK under PK at our institution between October 1, 2006 and November 30, 2009. The surgeries were performed at 1 institution using 1 consistent technique by 2 experienced surgeons and 1 cornea fellow.
Preoperative vision was recorded at a mean of 20/555 (range, 20/50 to hand motion). Postoperatively, the cornea was clear in all eyes and the vision was improved. The mean postoperative visual acuity was 20/101 (range, 20/30 to count fingers). The average follow-up was 16 months (range, 2-38 months). In the study group, concurrent cataract surgery was performed in 3 eyes (18%); IOL exchange was completed in 1 eye with removal of a dislocated IOL and placement of a posterior chamber, ciliary sulcus sutured IOL. One eye was left phakic and the remaining eyes were pseudophakic with a stable posterior chamber IOL at time of initial evaluation (12 of 17 eyes [71%]). Six eyes (35%) had undergone prior glaucoma surgery. No eyes had ACIOLs at the time of surgery. Two eyes of 1 patient had aniridia with scleromalacia and prior glaucoma surgeries.
In the 11 eyes with preoperative OCT imaging of the posterior PK surface, 8 eyes (73%) were identified with significant edge irregularity with posterior protuberance of the healed PK graft edge ( Figure 1 ).
Postoperative Complications
There were no cases of pupillary block glaucoma or iatrogenic primary graft failure in the study group. No separation of the PK wound occurred intraoperatively or postoperatively. No other early postoperative complications occurred. All patients had clearing of the failed PK graft and improved vision following their EK surgery. All grafts were clear at the last follow-up visit.
One graft dislocation occurred in the study group (1 of 17 eyes [5.9%]). There were no decentered grafts in the study group. The dislocation in the study group occurred in an eye with aniridia, a prior trabeculectomy, prior glaucoma drainage implant, 6 prior PKs, and severe scleromalacia that necessitated a supranasal wound placement. On postoperative day 1, the patient had a wound leak from a paracentesis site with resultant hypotony and partial graft dislocation. The patient underwent wound revision and a rebubbling with successful attachment of the EK graft and resultant clearing of the PK graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


