A surgeon facing the problem of a child with subglottic stenosis currently has a wide range of surgical options. Cricotracheal resection is the preferred option for grade IV and severe grade III stenoses that are clear of the vocal cords. Laryngotracheal reconstruction as a less extensive procedure is preferred for some grade II and less severe grade III stenoses. Stenosis close to the vocal cords remains a challenge and can be treated by extended partial cricotracheal resection. Pediatric surgeons and otolaryngologists should learn carefully the technique of partial cricotracheal resection for use in infants and children to achieve better results than with laryngotracheal reconstructions.
The management of laryngotracheal stenosis remains a challenging problem for otolaryngologists, especially in the pediatric age group. The complexity of the various preoperative situations implies that no single treatment modality can solve the problem. One has to take into consideration the type of the stenosis (congenital or acquired), its location (supraglottic, glottic, subglottic, or combined), its degree of obstruction and length in the craniocaudal axis, and its association with vocal cord ankylosis or neurogenic paralysis. The presence of tracheal damage (stenosis or localized malacia) related to the tracheostoma or the tracheotomy cannula can further complicate surgical management. According to the nature and severity of the conditions, various types of treatments exist. They range from endoscopic laser sessions with or without dilatation or stenting to laryngotracheal reconstruction (LTR) with anterior, posterior, or combined costal cartilage grafts to partial cricotracheal resection (PCTR) for the most severe grades of stenosis, to extended PCTR for combined glotto-subglottic stenosis .
The principle of subglottic resection in infants and children is basically identical to that described for adults. A child’s airway is smaller, however, and postoperative management is more challenging. Pediatric subglottic stenosis (SGS) is often associated with glottic scarring (eg, posterior glottic stenosis, cicatricial fusion of the vocal cords), and sometimes laryngeal and mediastinal malformations significantly add to the therapeutic challenge. The worst situations seen in this group of pathologies always result from (1) previously failed LTRs that can distort the laryngeal framework, (2) inappropriate overuse of the laser, and (3) misplacement of the tracheostoma that unnecessarily damages the normal trachea.
The best chance for patients lies in a successful first surgery, which implies that surgeons be fully trained in pediatric upper airway endoscopy and laryngotracheal surgery, because inappropriate initial management of SGS may lead to permanent, intractable sequelae.
Diagnosis
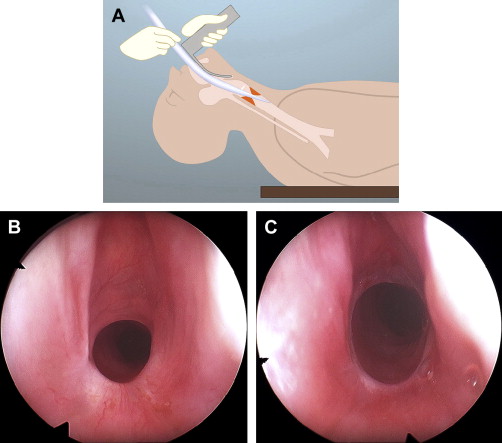
Infants and children with mild to moderate (< 60% reduction in luminal size) SGS may become symptomatic only during exercise or upper respiratory tract infection. They present with inspiratory stridor, dyspnea, and marked suprasternal and intercostal retractions. Recurrent or prolonged episodes of croup indicate possible SGS and warrant an endoscopic evaluation. In cicatricial stenosis, the endoscopic evaluation of the larynx and trachea provides all of the information required for the preoperative evaluation. Vocal fold mobility is assessed by transnasal fibroscopy with mask ventilation in deep sevoflurane anesthesia and spontaneous respiration ( Fig. 1 ). This examination also provides information on the patency of the nose, choanae, nasopharynx, and oropharynx.

Differentiating vocal fold immobility as a result of neurogenic causes from an interarytenoid fibrous adhesion is done by carefully inspecting the posterior commissure of the larynx using a 30-degree angled telescope and directly palpating the arytenoid cartilages during suspension microlaryngoscopy. The systematic use of Lindholm’s self-retaining vocal cord retractor (Storz No. 8654 B) helps differentiate bilateral vocal fold paralysis from posterior glottic stenosis ( Fig. 2 A–C). A fixed arytenoid raises the suspicion of fibrous ankylosis of the joint, but in the most difficult cases, this diagnosis is only safely made during open surgery.

Location, extent, and degree of stenosis are assessed using a bare magnifying telescope and the intubation laryngoscope while the patient is under general anesthesia and fully relaxed. The exact location of the stenosis with respect to the vocal folds, the tracheostoma, and the carina is measured in millimeters and in number of residual normal tracheal rings above and below the tracheostoma ( Fig. 3 A, B). The degree of the stenosis is measured by passing telescopes, endotracheal tubes, or bougies of different sizes through the stricture. In the pediatric community, the Myer-Cotton airway grading system is routinely used . This system classifies SGS in four grades and helps predict the rate of success after LTRs, because the less severe grades (I and II) have a far better outcome than the most severe grades (III and IV), which correspond to subtotal or total obstruction. For PCTR, this grading system is not useful as a predictor of success or failure because the stenotic segment is fully resected.

The endoscopy report also should mention the presence of any localized tracheomalacia and a possible infection of the airway. A bacteriologic smear is routinely taken. Finally, in the presence of congenital SGS, a bronchoesophagoscopy is performed to rule out a mediastinal malformation (eg, tracheoesophageal fistula, tracheobronchial anomalies, extrinsic vascular compression of the airway) . If precise description and measurements of the stenosis are obtained from the endoscopy, then radiographs add little to the preoperative evaluation. Lateral soft tissue and anteroposterior high kilovoltage radiographs, or more commonly CT scans with three-dimensional reconstructions, are useful in documenting the length of the segment to be resected in cases of complete stenosis of the airway. When a malformation of the mediastinum is suspected, MRI is the modality of choice .
Finally, if a single-stage operation is planned, then pulmonary function tests and neurologic evaluation should be considered, especially in children with malformations or previous long-term intubation for neonatal dyspnea of different origins. Gastroesophageal reflux disease should be ruled out systematically or actively treated if present .
Cricotracheal resection
Indications
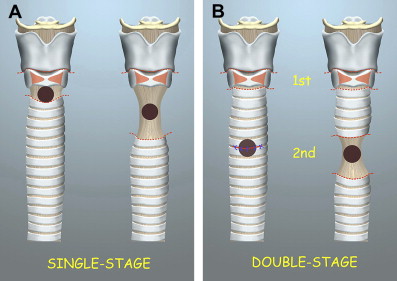
PCTR is the procedure of choice for the treatment of severe SGS (> 70% luminal obstruction) of congenital or acquired origin, but it is generally recommended to wait until a child reaches 10 kg of body weight before surgery is undertaken . The latter is performed as a single-stage operation (with concomitant resection of the tracheostoma during the surgery) when the stenosis is purely subglottic and the child is otherwise healthy. In children with multiple congenital anomalies or impaired neurologic or cardiopulmonary function, a double-stage PCTR (with postoperative maintenance of the tracheostoma) is preferable. If the SGS is combined with glottic involvement, such as posterior glottic stenosis, cicatricial fusion of the vocal cords, anterior laryngeal web extending into the subglottis, or distortion of the laryngeal framework resulting from failed LTRs, then PCTR is supplemented with a posterior cricoid split and costal cartilage graft that need stenting and maintenance of the tracheostoma until a complete healing of the subglottic area is obtained. This procedure is called “extended PCTR.”
Anesthetic technique
Jet ventilation for nontracheotomized children
In nontracheotomized children, the induction of anesthesia is done by mask ventilation with sevoflurane, followed by fentanyl and vecuronium. The stenosis is dilated with tapered bougies, and the child is intubated with the largest nasotracheal tube that will pass the stenosis ( Fig. 4 A–C). Because the stenosis is resected, the trauma induced to the subglottis by dilatation has no adverse consequence on the final outcome. Anesthesia is maintained with propofol, fentanyl, and vecuronium as needed. Once the cricothyroid membrane is incised, the endotracheal tube is withdrawn, and its tip is securely fixed with a Mersilene thread. A 10-Fr and 400-mm long catheter (external diameter: 3.3 mm) is passed through the tube and placed distally into the tracheal stump by the surgeon. Once the jet catheter is placed correctly, the endotracheal tube is further withdrawn from the operation field.
Resection of the stenosis is performed under excellent visual control, because the jet catheter can be displaced easily out of the operation field. The stenotic segment is resected, and after the posterior anastomosis is completed, all sutures for the lateral and anterior anastomosis are placed. Just before the sutures are tied, the distal trachea is rinsed with saline to moisten the mucosa and clean blood and secretions from it, and the endotracheal tube is pushed down into the trachea over the jet catheter using the leading Mersilene thread. The jet catheter is withdrawn, and normal ventilation is ensured through the endotracheal tube repositioned beyond the anastomosis. All sutures are then tied with the knots on the outside .
Conventional ventilation system in tracheotomized children
This setup is used in tracheotomized children whose tracheostomas will be resected during the same procedure. Two sets of ventilation tubes are prepared before draping the patient—one on the thorax for ventilation through the tracheostoma and another at the head end of the patient for ventilation through a nasotracheal tube. The whole dissection and resection of the stenosis is done while the patient is ventilated through the tracheostoma. The nasotracheal tube is passed through the larynx, and its tip is securely fixed with a Mersilene thread. The tube is withdrawn into the pharynx to provide a free operative field to the surgeon. The sutures of the posterior anastomosis and two lateral cricotracheal stitches are placed and tied while the child is still ventilated through the tracheal stump. Using the leading Mersilene thread, the nasotracheal tube is pushed beyond the posterior anastomosis into the distal trachea, and the remainder of the lateral and anterior sutures are placed with the knots tied on the outside .
Operative technique
Purely subglottic stenosis
The procedure is performed with the neck fully extended. Especially in small children, it is advisable to use magnifying glasses because of the small size of the structures being manipulated. It also aids in meticulous placement of the anastomotic sutures. A collar incision is usually made at the level of the second tracheal ring. In tracheotomized children, a horizontal crescent-shape excision of the skin is made around the stoma. The subplatysmal skin flaps are elevated, and the strap muscles are separated from the midline to provide exposure from the hyoid bone to the suprasternal notch. The isthmus of the thyroid gland is transected in the midline. The trachea is dissected anteriorly and laterally without identification of the recurrent laryngeal nerves by staying in close contact with the underlying cartilaginous rings. The vascular supply coming laterally from the tracheoesophageal grooves always should be carefully preserved, especially in extensive mobilization of the distal trachea.
At the level of the cricoid arch, the cricothyroid muscles are sharply dissected from the underlying cartilage until the cricothyroid joint is identified bilaterally. After having placed stay sutures to the distal normal tracheal wall, the inferior resection line is made first at the lower end of the stenosis or at the level of the tracheostoma if the latter is to be resected during the same surgical procedure. This allows a view of the stenosis from below and offers a good distal airway for ventilation. The membranous trachea is then dissected and separated from the anterior wall of the esophagus over a distance that corresponds to the height of the cricoid plate.
Unnecessary extensive separation of the trachea from the esophagus should be avoided. The advancement of the distal tracheal stump upward is achieved by freeing the cartilaginous rings from the mediastinal structures only anteriorly and laterally. Because of its elasticity, the esophagus shortens spontaneously without anterior bulging. The superior incision is started at the inferior margin of the thyroid cartilage in front and is passed laterally just anterior to the cricothyroid joints, which results in the complete resection of the anterior cricoid arch while avoiding injury to the recurrent laryngeal nerves that run posteriorly to the joint. In the subglottis, the uppermost incision of the posterior mucosa is made just below the cricoarytenoid joints, and the submucosal fibrosis that constitutes the posterior aspect of the SGS is fully resected, thus exposing the cricoid plate completely.
Because the luminal diameter of the distal airway is always much larger than that of the proximal subglottic resection line, the first normal tracheal ring used for the anastomosis must be adapted to the size of the subglottic lumen. In children, the difference in diameter between the subglottic space and the tracheal stump is even more pronounced than in adults. Any attempt at reducing the caliber of the trachea should be avoided. Instead, one should enlarge the subglottic lumen as much as possible without compromising voice quality. This approach is best achieved by widening the cricoid plate posteriorly and laterally with a diamond bur and performing an inferior midline thyrotomy up to the level of the anterior commissure of the larynx without transecting it ( Fig. 5 A).
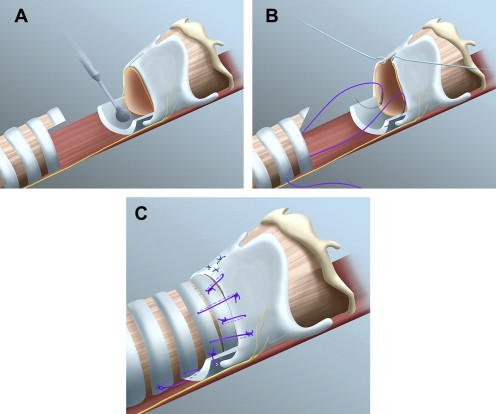
Because the thyroid cartilage is usually soft and pliable in infants and children, the inferior margins of both thyroid alae are easily spread apart. In this way, the subglottic lumen is enlarged considerably while the anterior commissure is kept intact, thus preserving a good voice. The triangular defect is filled in with a mucosa-lined cartilaginous wedge that is obtained from the first normal tracheal ring below the resected stricture. This procedure requires an additional resection of the lateral portion of the first normal tracheal ring used for the anastomosis. The denuded cricoid plate is covered with the membranous trachea after its upward mobilization.
Interrupted vicryl sutures (6-0 or 5-0 in children) are used for the posterior anastomosis, with the knots tied inside the lumen. The disadvantage of having a few sutures tied inside the lumen posteriorly is largely compensated for by the optimal approximation of the mucosa that is difficult to obtain with the knots tied outside the lumen. Fibrin glue is used to secure the membranous trachea to the cricoid plate. Depending on the child’s age, 4-0 or 3-0 vicryl sutures are used for the anterior and lateral anastomosis. The first stitch is passed through the posterolateral aspect of the first normal tracheal ring and through the cricoid plate laterally. It should emerge in a subperichondrial plane from the outer surface of the cricoid plate to avoid any lesion to the recurrent laryngeal nerves. This stitch is important and should be placed as meticulously as possible to bring the mucosa of the subglottis in close contact with the mucosa of the trachea ( Fig. 5 B). The thyrotracheal anastomosis is completed by placing the vicryl sutures between the tracheal ring and the thyroid cartilage anteriorly, with the knots tied on the outside. A tension-releasing suture is also placed between the third or fourth tracheal ring laterally and the inferior border of the cricoid plate ( Fig. 5 C).
Various techniques of tracheal and supralaryngeal release may be used to diminish the tension on the suture line, depending on the length of the tracheal segment to be resected and on the individual anatomy. Usually, the advancement of the distal tracheal stump upward is much easier in children than in adults. If necessary, a laryngeal release suffices; hilar and pericardial mobilizations, sometimes used in adults, should remain as an exception in children. At the end of the procedure, the neck is maintained in a flexed position. Sutures placed from the chin to the chest are never used to limit the extension of the neck during the postoperative period, although this measure has been recommended by different authors.
Single-stage versus double-stage partial cricotracheal resection
If a child is fit for a single-stage surgery, then two options usually exist, depending on the location of the tracheostoma. A single-stage PCTR with perioperative resection of the tracheostoma is chosen if no more than five tracheal rings must be resected with the SGS ( Fig. 6 A). This was the case in 55 of 90 (61%) PCTRs performed at our institution and implied that the tracheostoma had been placed at the third or fourth tracheal ring. The absence of a postoperative tracheostoma is favorable for the healing of the anastomosis, but longer tracheal resections carry greater risk of anastomotic dehiscence.