Corneal Opacification in the Developing World
Praveen Nirmalan
Prashant Garg
Gullapalli N. Rao
Corneal Opacification in Resource-Poor Countries
Blindness is a major public health problem globally.1 In 2002 an estimated 161 million people worldwide had vision impairment, including 37 million people who were blind.1 The distribution of the burden of blindness varies by location, age, and gender.1 In the least developed countries, the elderly and women bear the maximum burden of blindness. Reducing the burden of blindness worldwide requires an understanding of the factors influencing the burden of disease, including the magnitude and etiologic or risk factors and the development of appropriate service delivery models. This is especially important for countries that must use limited resources for health care delivery to address several health care priorities. Much of service delivery development in the realm of eye care, especially in resource-poor countries, has focused on service delivery models for age-related cataract and more recently for refractive services, primarily due to the larger prevalence and the relative ease of treatment for these two diseases.
Is Corneal Opacification Amenable to Service Delivery Model Development?
Service delivery model development, in resource-poor countries, should preferably be taken up only if the following criteria are met:
The magnitude of the disease or condition of interest is known and is sufficiently large to justify the development of a program.
There is enough understanding about the etiology, risk factors, and natural history of the disease or condition of interest.
The disease or condition of interest is amenable to screening and meets the World Health Organization (WHO) guidelines for any screening program.
Early detection and intervention are useful and prevent complications or recurrence.
Effective treatment for the disease or condition of interest exists and can be achieved with good outcomes.
Corneal opacification meets all of these criteria.
Magnitude
Corneal opacification is a major cause of blindness worldwide. Corneal opacification from causes other than trachoma accounts for 5.1% (range 3% to 12%) of global blindness and blindness from trachoma accounts for 3.6% (range 0.025% to 7.4%) of global blindness.1 These figures indicate that an estimated 1.9 million people across the world may be blind from corneal opacities due to nontrachomatous etiologies, and an additional 1.3 million people from corneal opacification due to trachoma.
These figures do not offer a complete picture of the burden from corneal opacification. The WHO defines blindness as a best corrected visual acuity worse than 3/60 or 20/400 in the better eye. Therefore, moderate to severe visual impairment is not reflected in these estimates. Additionally, the definition restricts itself to bilateral blindness and unilateral blindness from corneal opacification that is either related to trauma or scars after infectious keratitis is not reflected in these estimates. Thus, the actual burden of corneal opacification is much higher than the estimated 3.2 million. A study from India reported 6.8 (95% confidence interval [CI]: 5.0 to 8.8) million people are estimated to have corneal blindness in at least one eye, and one million of these have corneal blindness in both eyes.2
This “underreporting” of the burden of corneal opacification has several implications, one of which is the positioning of corneal opacification as a priority within eye care programs in relation to the other four major noncorneal causes for blindness: age-related cataract, age-related macular degeneration, glaucoma, and diabetic retinopathy. These four diseases are more likely to be bilateral than unilateral, and hence the estimates may more reasonably represent the burden of these diseases. It is entirely possible that corneal opacification, as a cause of blindness, may be second in magnitude only to age-related cataract if the burden of blindness from corneal opacification is estimated using the number of eyes affected. Information on the true impact of corneal disease is currently not available on a global scale. Another implication of the lack of knowledge of the full scale of corneal disease relates to the determination of workload and the development of adequate infrastructure and trained human resources to meet this workload. The actual number of keratoplasty surgeries that need to be performed will be much higher than estimates based on the 3.2 million people blind from corneal opacities. Much of corneal blindness occurs at younger ages compared to the later onset of cataract, macular degeneration, glaucoma, or diabetic retinopathy. A study from south India reported 2.67 million blind person years from corneal opacification and an additional 2.29 million blind person years from corneal opacities following childhood fevers.3
Etiologic and Risk Factors for Corneal Opacification
A multitude of disease mechanisms may lead to corneal involvement and opacification. Additional contributing factors include lack of public education about prevention, poor personal hygiene, poor sanitation, malnutrition, inadequate safety regulations in industry and other occupational areas, consanguineous marriages, and poor standards of medical and ophthalmic practice. However, accurate information is not available on the relative importance of these factors.
The epidemiology of corneal blindness is diverse and highly dependent on the ocular diseases endemic in each geographical area. Traditionally, important diseases responsible for corneal blindness include trachoma, onchocerciasis, leprosy, ophthalmia neonatorum, and xerophthalmia.4
Trachoma.
Currently trachoma is still the world’s leading infectious cause of blindness and is a leading cause of ocular morbidity. It is estimated by WHO that blindness from trachoma accounts for 3.6% (range 0.025% to 7.4%) of global blindness.1 Trachoma has always been associated with poverty, poor sanitation, and low socioeconomic status. The infection is transmitted from eye to eye by contaminated fingers, clothes, eye makeup, flies, and aerosolized nasopharyngeal secretions. It often results in corneal scarring with dense vascularization and ocular surface problems and frequently results in entropion and trichiasis. All these factors lead to disappointing outcomes of penetrating keratoplasty in trachoma patients.
Onchocerciasis.
Although onchocerciasis is currently a major cause of blindness in the world, progress toward eradication of the disease is a modern public health triumph. Data from West Africa show that blindness rates due to onchocerciasis are below 1% in communities that had up to 10% blindness rates at the onset of onchocerciasis control program. The incidence of new cases of onchocerciasis-related blindness in West Africa is now zero.5 There are still 18 million people infected with Onchocerca volvulus, over 95% of them in Central Africa and the rest in Central America.
Microfilariae, dead or alive, in the corneal stroma, produce “snowflake” or onchocercal punctate keratitis. Onchocerciasis can be a mild and reversible phenomenon, but severe longstanding invasion of numerous microfilariae into the cornea may lead to sclerosing keratitis, especially along the lower limbus, gradually spreading to the central optical zone.6 Sclerosing keratitis is usually seen in severe cases and is claimed to be the most common pathway to blindness in the savannas.
Ocular Leprosy.
Although there has been remarkable progress in the treatment of leprosy in the past 20 years, as many as 10 to 12 million people worldwide suffer from leprosy, and about 250,000 are blind from ocular leprosy.7 A majority of those affected are in Africa and the southern part of India. Involvement of the eye in leprosy has been reported with a variety of corneal manifestations, some of which may lead to blindness.8 Lagophthalmos with exposure keratitis and consequent infection resulting in scarring is an important mechanism. Hypoesthesia of cornea also can lead to corneal ulceration and ultimate opacification.9 Interstitial keratitis may also occur due to direct corneal infiltration by Mycobacterium laprae.10
Xerophthalmia.
Xerophthalmia, caused by vitamin A deficiency, is still the leading cause of childhood blindness. Most of these malnutrition-related ocular problems occur in resource-poor countries. It is estimated that about 10 million children have ocular signs of vitamin A deficiency and probably about 250,000 to 500,000 children become blind as a result every year, mainly in Asia and Africa. The subsequent high mortality in these children explains the relatively low prevalence of xerophthalmia in these countries in spite of its high incidence. Vitamin A deficiency is a predisposing factor in respiratory tract infections, diarrhea, corneal ulceration, blindness, and increased child mortality. Vitamin A deficiency occurs from decreased intake of the vitamin or its precursors or from an increased bodily requirement of the vitamin during infections, particularly measles. Predisposing factors for acute corneal ulceration from vitamin A deficiency are protein-energy malnutrition, malabsorption (chronic diarrhea), and measles. Corneal involvement manifests as bilateral, deep, punched-out ulcers with lack of luster in the remaining cornea, leading to rapid perforation (keratomalacia).11
Ophthalmia neonatorum.
Ophthalmia neonatorum or conjunctivitis in newborns refers to any conjunctivitis with discharge that occurs in the first 28 days of life. Although the worldwide incidence of ophthalmia neonatorum is not known, it represents a significant cause of childhood corneal blindness in developing countries. In the past century there has been a significant change in the spectrum of organisms causing this disorder as the incidence of chlamydial infection has risen dramatically in comparison to gonorrheal infections, especially in industrialized countries. If the infection is caused by Neisseria gonorrhoea the risk of blindness is high, compared to Chlamydia trachomatis or other less virulent pathogens. Ophthalmia neonatorum causes corneal blindness by producing corneal ulceration with subsequent scarring or perforation.
Several topical agents have been used for prophylaxis of ophthalmia neonatorum. In the more developed countries, antibiotics such as erythromycin and tetracycline are often used because of their effectiveness against chlamydial infection. In the developing world, access to these antibiotics and even silver nitrate may be limited by availability and associated expenses. However, antibiotics are becoming increasingly cheaper as more generic versions are available. Previous studies have demonstrated that 2.5% povidone-iodine, which may be reconstituted locally from powder at minimal cost, is an appropriate alternative. The incidence of ophthalmia neonatorum was reduced by 44% by povidone-iodine, compared to 34% by erythromycin and 24% by silver nitrate.12 It was more effective against Chlamydia, similarly effective against gonococcus, and even effective against herpes virus and human immunodeficiency virus. Thus, it acts against a broader spectrum of microbial agents and is well tolerated. Povidone-iodine is freely available even in the developing world as a surgical scrub agent. The temporary brown staining of the conjunctiva makes it easy to confirm administration.
Although these diseases still remain important causes of blindness, the recent success of public health programs in controlling onchocerciasis and leprosy as well as a gradual worldwide decline in the number of cases of trachoma has generated new interest in other causes of corneal blindness. These include corneal trauma, corneal ulceration, and complications from the use of traditional eye medicines.
Trauma.
In 1992, Thylefors et al. drew attention to the fact that trauma is an important cause of unilateral loss of vision in developing countries.13,14 They estimated that approximately 1.6 million people were blind, 2.3 million had bilateral low vision, and 19 million were unilaterally blind or had low vision from injuries. The geographic location, pattern of injury, causative agent, and age are among the factors that determine the degree of damage (Table 1).
TABLE 1. Pathways to Corneal Blindness from Trauma | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||
In urban areas and in the industrialized world, chemical injuries, accidents at the workplace, and automobile injuries are common. In rural areas of the developing world, minor trauma due to hazardous practices in agriculture, cottage industries, and other work places, as well as sports accidents, are responsible for a large proportion of corneal blindness. The effects of trauma are often aggravated by the use of inappropriate medications often sourced as over-the-counter medications and other harmful eye practices.
Corneal ulceration.
Corneal ulceration has been recognized as a silent epidemic in developing countries.15 Gonzales et al. found that the annual incidence of corneal ulceration in Madurai district in southern India was 113 per 100 000 people—ten times the annual incidence in United States.16 Extrapolating the estimated incidence of corneal ulcer from India, approximately 1.5 to 2 million people develop corneal ulcer annually in developing countries. Corneal infections caused by bacteria, fungi, viruses, and parasites are a frequent occurrence in most developing countries. Poverty, illiteracy, ignorance, lack of access to medical care, delayed or incorrect diagnosis, unavailability of appropriate drugs, and exposure to harmful treatment practices are impediments to effective prevention of corneal blindness in such cases. Medical attention is often sought only at an advanced stage.
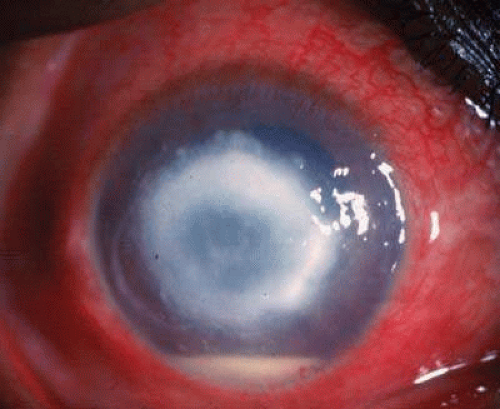
Bacterial corneal infections are caused by a wide variety of organisms. Pneumococcus seems to be the most common causative organism (Fig. 1); however, this varies according to the geographic location. In addition, staphylococcal, pseudomonal, and gonococcal infections frequently are encountered.17 This high incidence of Pneumococcus infection may be related to its association with chronic dacryocystitis.18
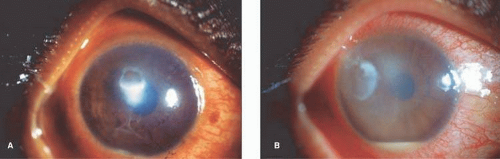 Fig. 1. Clinical photograph of bacterial keratitis caused by S. pneumoniae (A) and P. aeruginosa (B). |
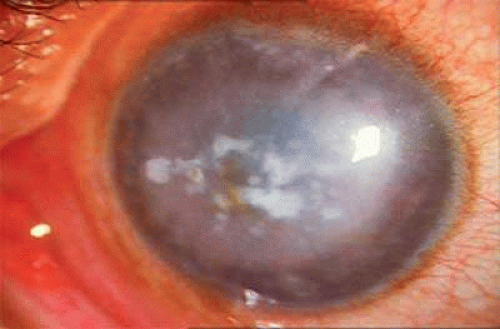
Fungal keratitis (Fig. 2) is as frequently seen as bacterial keratitis in many parts of the world. Aspergillus and Fusarium are the two most commonly isolated organisms, although this again may vary with geographic location. Predisposing factors include trauma, foreign body, and injudicious usage of topical steroids or indigenous medications. Delay in diagnosis, the relative ineffectiveness of antifungal agents, and the unavailability of effective drugs in most parts of the world hinder prevention and management.
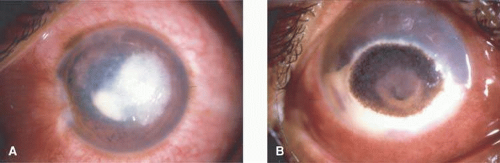 Fig. 2. Classical fungal keratitis characterized by raised infiltrate with hyphate edges. Note the presence of black pigmentation (B) caused by dematiaceous fungi. |
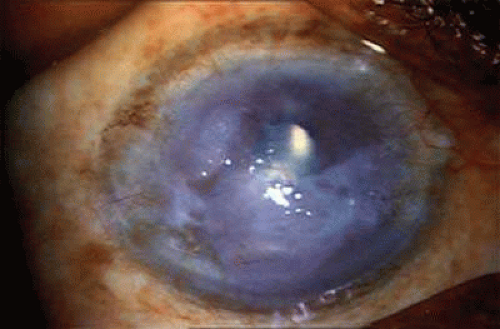
Acanthamoeba infection of the cornea is being reported with increasing frequency. While this is associated with contact lens wear in industrialized countries, in resource-poor countries it is almost exclusively seen in non–contact lens wearers (Fig. 3). Misdiagnosis and inappropriate treatment are common.19,20
Herpes simplex keratitis has the potential to cause corneal devastation, particularly when it presents as stromal disease. Failure to make the clinical diagnosis, lack of laboratory facilities, and inappropriate treatment often lead to recalcitrant stromal disease and consequent corneal opacification.
Traditional Eye Medicines.
The use of traditional eye medicines is an important risk factor for corneal blindness in many resource-poor nations. The extent of these harmful eye practices is not well known, but data from African countries indicate that these may be responsible for a significant proportion of childhood blindness (26% in Malawi, 20% in the United Republic of Tanzania).17,21 A study from India reported that 47.7% of subjects with corneal ulceration had been exposed to harmful traditional eye practices.22 A major problem with traditional eye medicines is that the ingredients are often contaminated, thus potentially leading to infections. Some remedies may cause a chemical burn in the eye. Usually such remedies are applied to both eyes, and their effects are often seen in the form of superimposed infections of the cornea. Children often show signs of having been subjected to harmful eye practices, and these cases are often clustered, especially in association with epidemics of measles or in relation to a particular traditional healer. The diagnosis is often difficult, as the patient or caregiver is often reluctant to reveal the details of such treatment.
The use of eye drops and ointments containing corticosteroids could be dangerous, particularly where these are freely available without a prescription. Injudicious use of topical steroids aggravates infectious diseases such as fungal keratitis and herpes simplex keratitis.
Congenital/Hereditary Diseases.
Corneal blindness due to congenital/hereditary problems occurs frequently in developing countries, particularly in areas such as the Middle East, which has high rates of consanguinity. Manifestations range from sclerocornea in the newborn to corneal dystrophies in various age groups (Fig. 4).
The exact prevalence of corneal blindness due to congenital/hereditary problems is not clearly established.
Iatrogenic Diseases.
Advances in ophthalmology have led to a number of new surgical techniques. However, the success of these techniques depends on adequate infrastructural support including modern equipment and adequate training of ophthalmologists. But the high cost of infrastructure, lack of human resources and training facilities, and inaccessibility to standardized and safe drugs and other supplies are major obstacles.
The prevalence of aphakic and pseudophakic corneal edema (Fig. 5) is high and now constitutes a common indication for penetrating keratoplasty.23 Poor surgical techniques, use of noxious pharmacologic agents, poor quality of intraocular lenses, and delay in the diagnosis and treatment of complications aggravates the problem.
Screening for Corneal Opacification
Four cardinal principles are recommended by WHO for any screening program:
The condition should be an important health problem with a recognizable presymptomatic state.
An appropriate screening procedure that is acceptable both to the public and health care professionals should be available.
Treatment for patients with recognizable disease should be safe, effective, and universally agreed.
The economic cost of early diagnosis and treatment should be considered in relation to total expenditure on health care, including the consequences of leaving the disease untreated.
Blindness from corneal opacification is preceded by any of the etiologic factors listed previously. Identification of corneal opacification is relatively easy and can be performed by trained community workers. Treatment for corneal opacification is essentially surgical with reasonably good reported outcomes. A study from the L.V. Prasad Eye Institute, Hyderabad, south India, reported graft survival at 1, 2, and 5 years of 79.6% (95% CI: 77.3%, 81.9%), 68.7% (95% CI: 65.7%, 71.7%), and 46.5% (95% CI: 41.7%, 51.3%), respectively.24 If treatment is inappropriate or delayed, corneal opacities from these different etiologic factors can progress, leading to further visual impairment or blindness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree