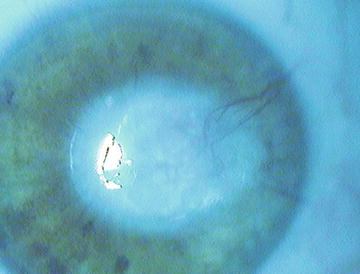
Fig. 2.1
Arcus senilis. (Archives Dr. A.M. Roszkowska)
Beyond senescence, the lipid arcus can be present in young males with hypercholesterolemia and hypertriglyceridemia. In fact, such association is actually considered a sign of cardiovascular diseases, and a special medical care with cardiovascular evaluation should be recommended in the presence of the arcus in the young [3–5].
2.2.2 Vogt Limbal Girdle
It is represented by limbal semilunar whitish lines that have an onset in the interpalpebral rim with a prevalence on the nasal zone. Limbal girdle is characterized by stromal thinning frequently associated to subepithelial calcium deposition. This common degenerative corneal change is present in 100 % of over 80-year-old subjects [3, 6].
Vogt described two types of girdle: type I, separated from the limbus by a clear zone, includes calcium deposits and is considered an early form of band keratopathy, while type II consists of hyaline degeneration with hyperelastosis in the peripheral Bowman’s membrane (Fig. 2.2).


Fig. 2.2
Vogt limbal girdle. (Archives Dr. A.M. Roszkowska)
2.2.3 Crocodile Shagreen
It involves mainly the anterior corneal stroma, but in some rare cases, it can involve the posterior as well. Clinically, it presents evident polygonal cloudities separated by the clear lines that recall the crocodile shagreen (Fig. 2.3). Such clinical manifestation seems to be related to the particular abnormal orientation of the stromal fibers. Electron microscopy revealed the presence of vacuoles throughout the corneal stroma, with some of them containing electron-dense material. Crocodile shagreen corneal degeneration is rather uncommon and can be observed casually during a routine slit-lamp ocular examination. It is considered innocuous, but in its posterior variant, in some cases it can affect visual acuity [7, 8].
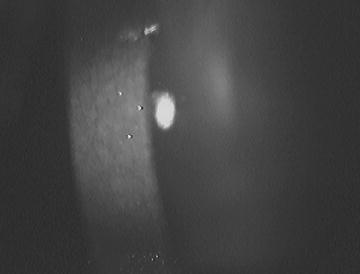
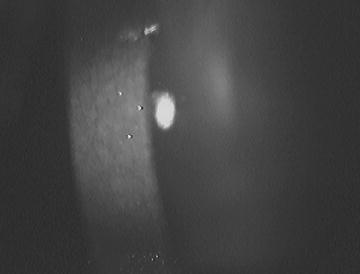
Fig. 2.3
Crocodile shagreen. (Archives Dr. A.M. Roszkowska)
2.2.4 Peripheral Corneal Guttae
Age-related changes in the corneal endothelium are related above all to the progressive cell loss with reduction of the cell density [9, 10]. The peripheral guttae are also known as Hassall-Henle bodies and are formed by the localized deposition of abnormal collagen secerned by the aging endothelial cells (Fig. 2.4). They consist of sporadic excrescences on the corneal endothelium localized prevalently in the middle periphery. This differentiates them from the Fuchs’ endothelial dystrophy, which starts in the center and spreads to the periphery, causing time corneal failure [11]. The number and extension of guttae are limited, so the endothelial cell density and function are not affected. In the pathogenesis of this age-related degeneration, the role of oxidative stress could be considered. In fact, oxidative stress involvement was established at the onset and progression of the Fuchs’ endothelial dystrophy, where similar histopathological alterations occur [2].
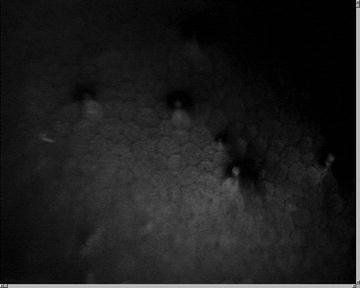
Fig. 2.4
Hassall-Henle bodies. (Archives Dr. A.M. Roszkowska)
2.3 Corneal Degenerations with Tissue Thinning
2.3.1 Terrien’s Marginal Degeneration
Terrien described it in 1900 as a noninflammatory, painless, evolutive thinning in the peripheral cornea, and its etiology remains poorly understood. Association with autoimmune disorders was described, so the autoimmune mechanism underlying the pathogenesis was hypothesized. Recently, an association with the chronic inflammatory skin condition known as erythema elevatum diutinum was reported [12]. Terrien’s marginal degeneration could be observed at any age, but prevalence in middle-aged males was observed. Generally, it is bilateral but asymmetric. Terrien’s degeneration generally starts in the superior area with a local haze separated from the limbus by a clear cornea. Successively, the peripheral stromal thins with typically an intact epithelial layer that characterizes this degeneration. Then the degenerative processes extend in a circumferential manner involving progressively the whole corneal periphery, and in the advanced forms, the degeneration becomes circumferential. Progressive neovascularization could arise, as well as lipid deposits, in the central border of the thinning (Fig. 2.5). Patients are asymptomatic until visual changes occur because of the progressive increment of irregular astigmatism [13, 14]. In some sporadic cases, slight inflammation could be present, as reported by confocal findings, and it responds well to the topical steroid therapy [15, 16]. Histopathological studies showed an increased lysosomal activity together with the absence of the Bowman’s membrane in the site of thinning [14]. As to the instrumental findings, the topographical examination demonstrates irregular astigmatism in advanced stages of the disease. The AC-OCT evaluation might be helpful in the evaluation of the peripheral thinning and in differential diagnosis with other peripheral corneal disorders. Recent AC-OCT findings report the stromal cavity formation in the peripheral cornea due probably to the collagen phagocytosis [17]. The differential diagnosis should consider the peripheral corneal melt, Mooren’s ulcer, pellucid marginal degeneration, and dellen. The treatment consists of optical correction of irregular astigmatism. In advanced forms, contact lenses are recommended. The most dreaded complication in severe Terrien’s degeneration is related to corneal perforation. Perforation could be spontaneous or could result from any trauma, so the surgical approach should be considered when extreme thinning occurs [18]. Lamellar ring-shaped peripheral corneoscleral grafting is usually considered, but in some cases, tissue excision with appropriated suture could be performed [19, 20].
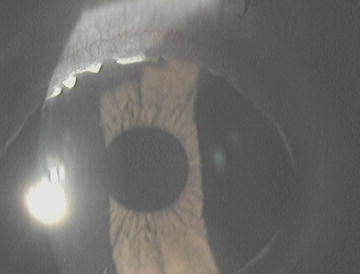
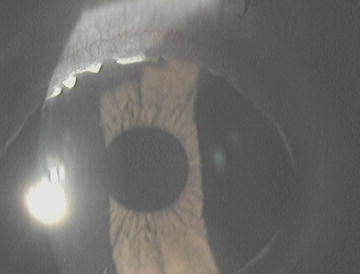
Fig. 2.5
Terrien’s marginal degeneration. (Archives Dr. A.M. Roszkowska)
2.3.2 Dellen
Dellen is a localized area of corneal thinning in the periphery next to the limbus. It is located in proximity to the areas of tissue swelling or inflammation when correct spreading of the tear layer is highly disturbed. Frequently, it follows some surgical procedures that induce conjunctival chemosis with paralimbal elevation, which produces a localized abnormality of the tear film layer with following localized dehydration and thinning [21–24]. This relatively common condition is reversible. In fact, the restoration of the normal film layer spreading and intense lubrication constitute the appropriate therapy for this disorder. Recently, the use of a large-diameter soft contact lens was proven to be an effective therapeutic solution to treat the dellen that arose after a pterygium removal [25].
2.4 Corneal Degenerations with Material Deposits
2.4.1 Salzmann’s Nodular Degeneration
Salzmann’s nodular degeneration (SND) is a noninflammatory, slowly progressive disease characterized by single or multiple whitish-gray subepithelial corneal nodules. Salzmann described it in 1925 in association with keratoconjunctivitis, but with time, several different disorders coexisting with this disorder were detected. To date, its etiopathogenesis remains unknown, but it is considered to be associated with ocular surface inflammation or chronic trauma. However, several cases with no previous corneal pathology have been reported and are considered idiopathic.
Clinically, the typical clinical signs could be observed during slit-lamp examination, with either solitary or multiple nodules elevated on the corneal surface and located in the midperiphery of the cornea. In some cases, single or few nodules are present in one or more quadrants during routine ocular examination in asymptomatic patients, and sometimes, the nodules may invade the central zone. When multiple nodules are present, they have a typical circular arrangement and might be confluent in the advanced stages. A normal clear cornea between the nodules is a characteristic clinical feature (Fig. 2.6). The ocular surface disorders involved in the etiopathogenesis of Salzmann’s degeneration are Meibomian gland dysfunction and dry eye disease followed by rosacea, phlyctenular keratitis, vernal keratoconjunctivitis, trachoma and interstitial keratitis. The chronic injuries that are most commonly associated with the development of the degenerative changes are extended contact lens use and previous corneal surgery followed by actinic exposure, recurrent erosions, and chemical or thermal injuries [26–29].
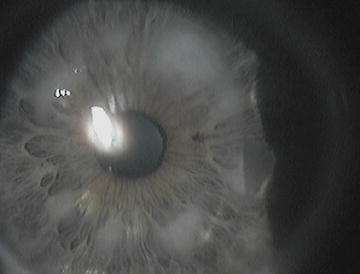
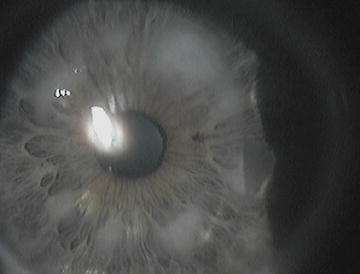
Fig. 2.6
Salzmann nodular degeneration. (Archives Dr. A.M. Roszkowska)
Recently, SND in patients with Crohn’s disease was reported, and a hypothesis about association with systemic diseases was advanced [30, 31].
Therefore, although the etiology remains uncertain, it is hypothesized that Salzmann’s nodular degeneration can be triggered by multiple events that lead to a nonspecific corneal tissue reaction based on individual predisposition. It appears to be more frequent in middle-aged women, and it is bilateral in about 60 % of cases. The main symptoms are visual disturbances and photophobia, ocular discomfort, mainly characterized by dryness, and foreign body sensation. In severe forms, characterized by very elevated nodules, painful epithelial lesions can occur. Visual impairment is progressive and due to an astigmatic defect produced by the nodules. Severe corneal irregularities in advanced stages generate high irregular astigmatism with severe visual loss. Although the diagnosis of Salzmann’s degeneration is exclusively based on clinical findings, several instrumental examinations such as corneal topography, anterior segment optical coherence tomography, and confocal microscopy are useful to provide a better understanding of the corneal alterations and to quantify the amount of visual impairment. Corneal topography demonstrates the irregularities of the corneal shape produced by corneal nodules, and the induced surface alteration depends on their number and localization.
AC-OCT allows the evaluation of the nodules’ dimension and depth, allowing the investigation of the stromal extension of the nodules that can help decide the surgical approach [32]. Confocal microscopy showed an increased reflectivity of the anterior stroma with abnormal and activated keratocytes and marked stromal scatter corresponding to the nodules as a result of the presence of fibrosis [33–35].
Histopathological studies have revealed that the corneal nodules are located subepithelially but may extend to one-third of the anterior stroma and are formed by a dense connective tissue with hyaline degeneration. The corneal epithelium has an irregular thickness, with extremely increased thinning over the corneal nodules. The Bowman’s membrane exhibits disruption, and in the correspondence of the nodules, it is no longer appreciable and frequently replaced by fibrosis. Subepithelial fibrosis is a frequent histopathological finding, with activated fibroblasts beneath the epithelial cells. Increased expression of matrix metalloproteinase-2 (MMP-2) was recently detected in patients affected by Salzmann’s degeneration, and this may be responsible for the induction of the basement membrane and Bowman’s layer disruption [33, 35–37].
Therapy is related to the symptoms and severity. In early forms, treatment is aimed at reducing the presenting symptoms with conservative therapy concerning eyelid hygiene, lubricants, and anti-inflammatory eyedrops sufficiently to eliminate dry eye symptoms and foreign body sensation. Visual loss is an indication for surgical treatment, which consists of the removal of the nodules and the restoration of corneal surface regularity. In superficial nodules, manual removal with a crescent knife is sufficient and leaves a uniform smooth underlying surface. In the case of deeper ingrowth that involves the anterior stroma, after the nodule’s removal, the excimer laser PTK is usually performed to smoothen the surface. In some cases with deep ingrowth, the anterior lamellar becomes necessary [38, 39]. The recurrence of Salzmann’s nodules after surgical removal can occur with varying prevalence rates (18–21.9 %) and periods of time to recurrence (1 month to 6 years) [40–42].
2.4.2 Band Keratopathy
Band keratopathy consists of the deposition of calcium salts in the interpalpebral region. It starts in proximity to the limbus in the corneal periphery nasally and temporally at the same time. Successively, it spreads gradually to the center, forming a band-like whitish-gray plaque. Clear cornea separates the peripheral border of the band from the limbus. Visual acuity decreases with the advancement of deposits. In fact, in the advanced stages, the density of calcium deposition might create a severe visual impairment (Fig. 2.7). Moreover, in severe lesions, the deposits become elevated and produce considerable discomfort because of the ocular surface alterations.
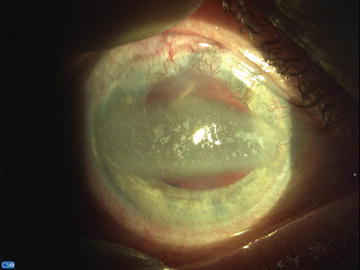
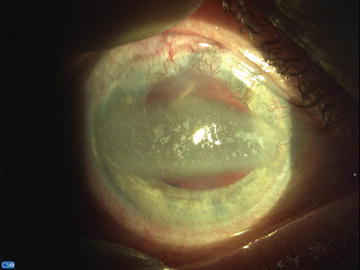
Fig. 2.7
Band Keratopathy. (Archives Prof. E. Wylegala)
Band keratopathy can affect a single eye when it arises after local disorders such as chronic anterior uveitis, interstitial keratitis, severe injury, chronic corneal inflammations, and phthisis bulbi. It is bilateral when generated by a general disorder. Systemic conditions underlying the band keratopathy onset are chronic renal failure, juvenile rheumatoid arthritis, and hyperuricemia.
Histology shows calcium salt deposits localized in the Bowman’s layer, basement membrane of epithelium, and anterior stroma [43].
As for the treatment, the cause of band keratopathy should be addressed. The coexistence of an underlying systemic or local disorder must be recognized and treated first. Successively, calcium deposits are treated with a chelation procedure, which has been proven to be effective and easy to perform. Mechanical debridement was demonstrated to be effective as well in early stages. In case of dense and thick deposits, the manual scraping is necessary prior to chelation. Chelation is performed using a 1.5–3.0 % solution of ethylenediaminetetraacetic acid (EDTA) for 15–20 min. If required, the corneal surface might be further smoothened by excimer laser phototherapeutic keratectomy. Epithelial layer restoration could be enhanced by amniotic membrane application, which may help optimize the clinical outcome. Only in very advanced cases with severe visual impairment could the lamellar keratoplasty be considered a therapeutic option [43–45].
2.4.3 Lipid Keratopathy
Lipid keratopathy can occur spontaneously or may be a consequence of a previous ocular injury or inflammation. The first form is a primary one, rather infrequent, because of stromal deposits of cholesterol, fats, and phospholipids. It is not associated with vascularization.
The second form occurs as a secondary disorder associated to previous ocular diseases or injury. The secondary lipid keratopathy is much more common, and it is typically associated with corneal vascularization (Fig. 2.8). The most frequent corneal pathologies underlying the secondary lipid keratopathy are herpetic infections, both simplex and zoster. Treatment should focus on the underlying disease first. Successively, abnormal vascularization should be eliminated by argon laser photocoagulation or needle point cautery to induce the absorption of the lipids through the destruction of the feeder vessels.