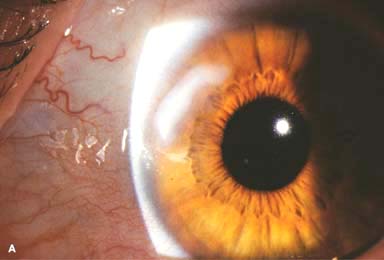
Corneal arcus is a very common, bilateral condition that may be either age-related (arcus senilis) or associated with hyperlipidemia in younger individuals (arcus lipoides).
 Lipid deposits begin inferiorly, then superiorly, and later extend circumferentially to form a white perilimbal band about 1 mm in diameter with a sharp outline peripherally and a more diffuse boundary centrally. A clear zone of cornea separates it from the limbus (Fig. 6-1A).
Lipid deposits begin inferiorly, then superiorly, and later extend circumferentially to form a white perilimbal band about 1 mm in diameter with a sharp outline peripherally and a more diffuse boundary centrally. A clear zone of cornea separates it from the limbus (Fig. 6-1A).
 May be accompanied by mild, nonprogressive thinning of the clear zone of the cornea (furrow degeneration)
May be accompanied by mild, nonprogressive thinning of the clear zone of the cornea (furrow degeneration)
 Check for hyperlipidemia in patients under age 40 years. If unilateral, check for carotid disease on the uninvolved side.
Check for hyperlipidemia in patients under age 40 years. If unilateral, check for carotid disease on the uninvolved side.
 Patients are asymptomatic, and ocular treatment is not necessary.
Patients are asymptomatic, and ocular treatment is not necessary.
WHITE LIMBAL GIRDLE OF VOGT
 White limbal girdle of Vogt is a very common, bilateral, innocuous, age-related condition characterized by chalky-white, crescentic deposits (elastotic degeneration) along the nasal and temporal perilimbal cornea. It may or may not be separated from the limbus by a clear zone (Fig. 6-1B).
White limbal girdle of Vogt is a very common, bilateral, innocuous, age-related condition characterized by chalky-white, crescentic deposits (elastotic degeneration) along the nasal and temporal perilimbal cornea. It may or may not be separated from the limbus by a clear zone (Fig. 6-1B).
 Patients are asymptomatic, and ocular treatment is not necessary.
Patients are asymptomatic, and ocular treatment is not necessary.
CROCODILE SHAGREEN
 Crocodile shagreen is characterized by grayish-white, polygonal stromal opacities separated by relatively clear spaces. The lesions usually involve the anterior stroma (anterior crocodile shagreen), but they may also be found more posteriorly (posterior crocodile shagreen) (Fig. 6-1C).
Crocodile shagreen is characterized by grayish-white, polygonal stromal opacities separated by relatively clear spaces. The lesions usually involve the anterior stroma (anterior crocodile shagreen), but they may also be found more posteriorly (posterior crocodile shagreen) (Fig. 6-1C).
 Patients are asymptomatic, and ocular treatment is not necessary.
Patients are asymptomatic, and ocular treatment is not necessary.
CORNEA FARINATA
 Cornea farinata is a relatively common condition characterized by bilateral, innocuous, minute, “flour-dust” lipofuscin-like deposits in the deep stroma near Descemet’s membrane. It is most prominent centrally.
Cornea farinata is a relatively common condition characterized by bilateral, innocuous, minute, “flour-dust” lipofuscin-like deposits in the deep stroma near Descemet’s membrane. It is most prominent centrally.
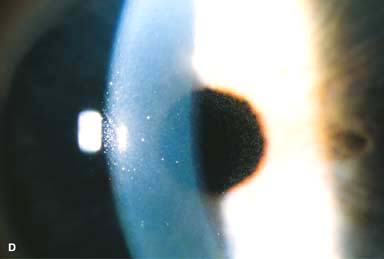
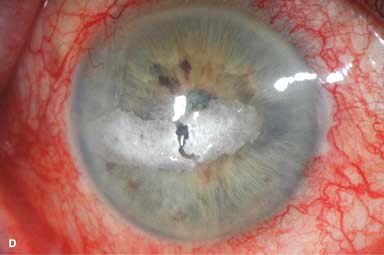
 These opacities are best seen with retroillumination off the iris (Fig. 6-1D).
These opacities are best seen with retroillumination off the iris (Fig. 6-1D).
 Patients are asymptomatic, and ocular treatment is not necessary.
Patients are asymptomatic, and ocular treatment is not necessary.
POLYMORPHIC AMYLOID DEGENERATION
 Polymorphic amyloid degeneration is a fairly common, bilateral, innocuous, degenerative condition usually seen after the age of 50 years.
Polymorphic amyloid degeneration is a fairly common, bilateral, innocuous, degenerative condition usually seen after the age of 50 years.
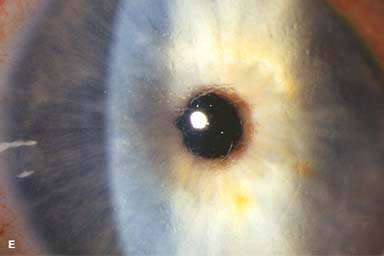
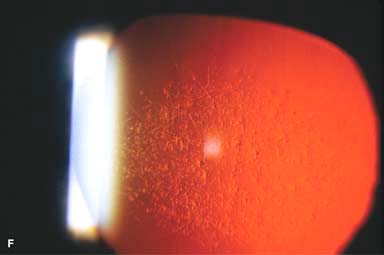
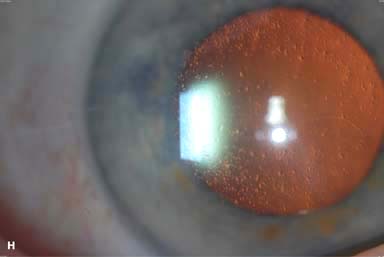
 It is characterized by varying sizes of refractile, punctate, comma-shaped, and filamentous amyloid deposits throughout the stroma, but is generally most prominent centrally and posteriorly. These deposits are best seen with retroillumination off the retina (Fig. 6-1E–H).
It is characterized by varying sizes of refractile, punctate, comma-shaped, and filamentous amyloid deposits throughout the stroma, but is generally most prominent centrally and posteriorly. These deposits are best seen with retroillumination off the retina (Fig. 6-1E–H).
 It is not associated with any systemic disorder.
It is not associated with any systemic disorder.
 Differential diagnosis: cornea farinata and lattice dystrophy
Differential diagnosis: cornea farinata and lattice dystrophy
 Patients are asymptomatic, and ocular treatment is not necessary.
Patients are asymptomatic, and ocular treatment is not necessary.
FIGURE 6-1. Corneal arcus. A. A circular yellow-white lipid deposition is present adjacent to the limbus for 360 degrees. Note the clear zone between the arcus and the limbus. Limbal girdle of Vogt.B. A crescentic, relatively dense white opacity is seen at the limbus at the 9 o’clock position. There is a small clear zone between the limbal girdle and the limbus. Crocodile shagreen. C. Gray-white polygonal stromal opacities are evident in this cornea. They may be located in the anterior or the posterior stroma. Cornea farinata.D. Tiny, “flour-dust” deposits are seen at the pupillary margin. These pinpoint opacities are located in the deep stroma. They do not affect vision. Polymorphic amyloid degeneration.E. Amyloid deposits in various shapes, including dots, commas, and lines, are seen in the corneal stroma. This condition is a degeneration, not a dystrophy. It is similar to lattice dystrophy in that they both involve amyloid deposition; however, lattice dystrophy is an inherited condition that is typically associated with recurrent erosions and decreased vision in young adulthood. F. This eye with polymorphic amyloid degeneration has dense central amyloid deposits readily seen in retroillumination off the retina. Polymorphic amyloid degeneration. G. Multiple small gray-white polymorphic amyloid degeneration opacities are present, primarily in the mid-periphery, in this elderly woman H. The polymorphic amyloid degeneration opacities in the same eye are highlighted in retroillumination.




CORNEAL DEPOSITS—NONPIGMENTED
BAND KERATOPATHY
Band keratopathy is a common condition characterized by calcium deposits in the subepithelial space, Bowman’s layer, and anterior stroma.
Etiology
 Ocular
Ocular
 Chronic ocular inflammation (e.g., iridocyclitis, juvenile rheumatoid arthritis, corneal edema, interstitial keratitis, phthisis bulbi)
Chronic ocular inflammation (e.g., iridocyclitis, juvenile rheumatoid arthritis, corneal edema, interstitial keratitis, phthisis bulbi)
 Silicone oil in the eye, especially the anterior chamber
Silicone oil in the eye, especially the anterior chamber
 Metabolic
Metabolic
 Hypercalcemia or hyperphosphatemia
Hypercalcemia or hyperphosphatemia
 Gout
Gout
 Chronic renal failure
Chronic renal failure
 Hereditary: familial
Hereditary: familial
 Other
Other
 Chronic exposure to toxic vapors (e.g., mercury)
Chronic exposure to toxic vapors (e.g., mercury)
 Idiopathic (age-related)
Idiopathic (age-related)
Symptoms
 Often asymptomatic. If central, vision may be affected. Ocular irritation can develop if thick calcium plaques flake off and cause an epithelial defect.
Often asymptomatic. If central, vision may be affected. Ocular irritation can develop if thick calcium plaques flake off and cause an epithelial defect.
Signs
 Peripheral, interpalpebral plaque of calcium deposit usually separated from the limbus by a thin line of clear cornea (Fig. 6-2A–C)
Peripheral, interpalpebral plaque of calcium deposit usually separated from the limbus by a thin line of clear cornea (Fig. 6-2A–C)
 The plaque typically begins at the nasal and temporal cornea and extends centrally.
The plaque typically begins at the nasal and temporal cornea and extends centrally.
 It often contains small holes and clefts, giving it a “Swiss cheese” appearance.
It often contains small holes and clefts, giving it a “Swiss cheese” appearance.
 Advanced lesions may become plaquelike, nodular, and elevated (Fig. 6-2D).
Advanced lesions may become plaquelike, nodular, and elevated (Fig. 6-2D).
Treatment
 Mild cases may be observed or treated with lubricants (e.g., artificial tear drops or ointments).
Mild cases may be observed or treated with lubricants (e.g., artificial tear drops or ointments).
 Severe cases (with visual, painful, or cosmetic indications) can be treated with chelation using disodium ethylenediamine tetraacetic acid 3% or superficial keratectomy using the excimer laser (phototherapeutic keratectomy, or PTK) or a blade.
Severe cases (with visual, painful, or cosmetic indications) can be treated with chelation using disodium ethylenediamine tetraacetic acid 3% or superficial keratectomy using the excimer laser (phototherapeutic keratectomy, or PTK) or a blade.
Prognosis
 Excellent for the ocular calcium deposits. The band keratopathy can recur, especially if the underlying condition persists.
Excellent for the ocular calcium deposits. The band keratopathy can recur, especially if the underlying condition persists.
 Calcium chelation can be repeated if necessary.
Calcium chelation can be repeated if necessary.
 Epithelial healing problems may occur. Vision is often limited, as a result of residual corneal scarring or other ocular pathology.
Epithelial healing problems may occur. Vision is often limited, as a result of residual corneal scarring or other ocular pathology.
FIGURE 6-2.Band keratopathy. A. A thin layer of calcium deposition can be seen adjacent to the limbus nasally and temporally. Note the thin line of clear cornea between the band keratopathy and the limbus. B. This eye had central calcium deposition obscuring the view of the iris and pupil. Band keratopathy.C. This eye has the classic limbus-to-limbus horizontal “band” of band keratopathy. D. This eye with chronic corneal edema from herpes zoster keratopathy has a dense central plaque of calcium deposition. Some of the plaque spontaneously flaked off centrally.



SALZMANN’S NODULAR DEGENERATION
Salzmann’s nodular degeneration is a fairly common, unilateral or bilateral condition characterized by smooth gray-white elevated lesions of the cornea.
Etiology
 It is often found in eyes with a history of chronic keratopathy, such as interstitial keratitis, vernal keratoconjunctivitis, keratoconjunctivitis sicca, phlyctenulosis, and trachoma, but frequently appears in otherwise normal eyes.
It is often found in eyes with a history of chronic keratopathy, such as interstitial keratitis, vernal keratoconjunctivitis, keratoconjunctivitis sicca, phlyctenulosis, and trachoma, but frequently appears in otherwise normal eyes.
Symptoms
 Often asymptomatic. May affect vision if it involves the paracentral or central cornea; may cause a foreign-body sensation if it becomes very elevated
Often asymptomatic. May affect vision if it involves the paracentral or central cornea; may cause a foreign-body sensation if it becomes very elevated
Signs
 Single or multiple, discrete, white or gray-white or occasionally bluish, smooth, elevated nodules anywhere on the surface of the cornea (Fig. 6-3)
Single or multiple, discrete, white or gray-white or occasionally bluish, smooth, elevated nodules anywhere on the surface of the cornea (Fig. 6-3)
 Long-standing nodules may have iron pigment deposition in the epithelium at the base of the nodule.
Long-standing nodules may have iron pigment deposition in the epithelium at the base of the nodule.
Differential Diagnosis
 Spheroidal degeneration: small, globular, yellow-brown granules are found in the superficial corneal stroma.
Spheroidal degeneration: small, globular, yellow-brown granules are found in the superficial corneal stroma.
Treatment
 Mild cases are observed or treated with lubrication. If the nodules are causing symptoms, they may be treated with superficial keratectomy with a blade or excimer laser PTK. Topical mitomycin C at the time of surgical excision may decrease the rate of recurrence. Rarely, if severe, it may require a lamellar keratoplasty.
Mild cases are observed or treated with lubrication. If the nodules are causing symptoms, they may be treated with superficial keratectomy with a blade or excimer laser PTK. Topical mitomycin C at the time of surgical excision may decrease the rate of recurrence. Rarely, if severe, it may require a lamellar keratoplasty.
Prognosis
 Very good to excellent. Can recur after surgical excision
Very good to excellent. Can recur after surgical excision
FIGURE 6-3.Salzmann’s nodular degeneration.A. A gray-white elevated lesion is seen in the peripheral cornea from the 9 to 11 o’clock positions. These lesions may be single or multiple and peripheral or central. If they are causing symptoms, they can usually be treated with a superficial keratectomy or excimer laser PTK. Salzmann’s nodular degeneration. B. This eye has approximately six Salzmann’s nodules superiorly. Flatter Salzmann’s opacities can be seen in between the more distinct elevated nodules. C. Severe paracentral and peripheral Salzmann’s nodular degeneration is obvious from approximately 9 to 6 o’clock.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


