Contact Lens and Prosthesis Infections
John K. G. Dart
In the past three decades the use of contact lenses (CLs) has dramatically increased both in affluent societies and in the emerging economies. Estimates of the numbers of CL wearers, based on market research, give 34 million users in the United States in 2000 (Contact Lens Council, 8201 Corporate Drive, Suite 850 Landover, MD20785), an overall population penetrance of 12% (USA 2000 Census data, U.S. Dept of Commerce, Economics and Statistics Administration). In England and Wales, in 1998 there were over 2.25 million CL users, a penetrance of 5%, with wide regional variations,1 These figures are likely to be representative of those for the developed economies. Most lenses are used as an alternative to spectacles for the correction of low refractive errors. This is sometimes termed “cosmetic” lens wear to distinguish it from the medical use of lenses, either for the correction of refractive errors such as aphakia and keratoconus, or as therapeutic lenses in the management of ocular surface disease. Prosthetic contact lenses are used to improve the appearance of damaged eyes. To the majority of users these applications of lenses have delivered vision and cosmesis, unobtainable with spectacles.
However, CLs have always been associated with complications. Most of these have no long-term consequences for vision and resolve when lens wear is discontinued.2 Of the infections that may complicate lens wear, microbial conjunctivitis is generally self-limiting. However, microbial conjunctivitis is probably over-diagnosed in CL users and is often mistaken for other, non-microbial, causes of conjunctivitis that are peculiar to CL and prosthesis users. This can result in inappropriate treatment and unnecessarily prolonged morbidity. On the other hand, corneal infection (microbial keratitis), although infrequent, is one of the most serious complications of CL wear because of its potential for loss of vision and progression after lens removal. It may occasionally result in a fulminating infection with corneal perforation and blindness. With such large numbers of users of contact lenses, even a low incidence of serious complications may result in substantial numbers of affected individuals in the community. In some populations CL wear has now become the major predisposing factor for corneal infection3,4,5 and is a matter of public health importance. Infections in CL users have a different epidemiology and pathogenesis compared to infections in other patient groups.2 Understanding these differences is essential to the management and prevention of keratitis in this large population of susceptible individuals.
This chapter discusses the differentiation of microbial conjunctivitis and keratitis from the other causes of conjunctival and corneal inflammation in CLs users. The epidemiology in terms of the causative organisms and the incidence and risk factors are summarized. The evidence from the epidemiologic, clinical, and laboratory studies is integrated to describe the current understanding of the pathogenesis of infection in lens users.
CONTACT LENS CLASSIFICATION
CLs may be classified by their material, type of fit, wearing and disposal schedules6,7 as shown in Table 1. They may also be classified by the indication for their use. Differences between lenses are important because they are associated with different risks for the development of infection. Differences in the fit (relationship of the lens to the ocular surface) and physical characteristics of CLs may account for some of the differences in the risks for keratitis (discussed later).
TABLE 1. Classification of Contact Lenses | |||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||
Soft contact lenses (SCLs), which look the same whether for daily or extended wear but differ in their water content and thickness, are fitted to ride over the limbus and move 1 to 2 mm with each blink. These lenses depend on oxygen diffusion through the lens material to satisfy the oxygen requirements of the cornea.8 Silicone hydrogel, a new soft lens material, was introduced in 1999 and approved for extended wear use for periods of 6 and 30 days in different countries.9 Unlike soft hydrogel, this material utilizes silicone to greatly increase oxygen transmission through the lens while maintaining the “feel” of a soft lens.10
Rigid contact lenses (RCLs) are usually fitted within the cornea to enable good movement with each blink. The lens movement and the shape of the lens edge in a rigid lens is designed to ensure adequate flow of oxygenated tears under the lens in order to meet the oxygen demands of the cornea; in rigid gas-permeable (RGP) CLs, oxygen also diffuses through the lens. Modern RGP lens materials provide a greater oxygen transmission than soft hydrogel lens materials. As a result of this and the tear flow under the lens, these meet corneal oxygen requirements.11
Scleral lenses are fitted to the sclera, and the physiologic requirements of the cornea are met, as far as possible, by designing the lens to allow tear exchange under the lens. More recently, gas-permeable scleral lens materials have become available.12
Lens wearing and replacement schedules also influence the risk for keratitis. Wearing schedules may be either daily wear (DW), in which they are removed for sleep, or extended wear (EW), in which they are retained for at least 24 hours without removal, usually for 1 to 4 weeks of continuous wear. In the United States, the Food and Drug Administration recommends that the use of soft hydrogel lenses for continuous wear be limited to 7 days only.13 Silicone hydrogel lenses were approved in 2001 for up to 30 days of continuous wear following evidence of a reduced risk of infection. SCLs are much more widely used than RGP CLs for extended and flexible wear. SCLs may be reusable, planned replacement, or disposable types. Reusable SCLs are maintained for 6 months or more. Planned replacement SCLs are replaced every 1 to 26 weeks; they are usually dispensed in multipacks and replaced periodically after further assessment by the practitioner. Disposable SCLs are discarded after each use, either daily (daily disposable) or after a period of continuous wear.
Most CLs are worn for cosmetic reasons as an alternative to spectacles by individuals with low degrees of hyperopia and myopia rather than for any improvement in vision. The most common medical indications are the correction of vision in keratoconus (usually RGP CLs) and aphakia (commonly daily or extended wear RGP CLs or SCLs), and as therapeutic CLs, which are fitted primarily for maintaining the integrity of the eye and relieving pain, rather than for vision; these may be of any design and material but are usually semi-scleral SCLs. Prosthetic CLs are fitted to improve the appearance of a damaged eye and may be made of a variety of materials, usually in semi-scleral or scleral designs, to achieve their prosthetic effect; soft, polymethylmethacrylate, and gas-permeable materials are all used.
CONJUNCTIVITIS
DISTINGUISHING INFECTIVE FROM OTHER CAUSES OF CONJUNCTIVITIS
Conjunctival inflammation in cosmetic CL and prosthetic CL users has several causes that must be distinguished from infection. CL-related papillary conjunctivitis (giant papillary conjunctivitis)14 is frequently confused with conjunctival infection particularly in prosthetic CL users,15 in whom lens-related papillary conjunctivitis can be florid. Thimerosal keratoconjunctivitis, now an infrequent diagnosis as a result of the withdrawal of this agent as a disinfectant in CL solutions in most countries, may also be misdiagnosed as microbial conjunctivitis.16 These diseases can usually be distinguished by distinctive features of their onset, symptoms, and signs that only superficially resemble those in microbial conjunctivitis. Conjunctival culture is seldom necessary and may be misleading, as a light growth of organisms from the conjunctival sac is a normal finding. Table 2 describes the principal distinguishing features of these disorders. Complete resolution of clinical signs is normal after microbial conjunctivitis, unless this is associated with membrane formation, whereas, following both CL-related papillary conjunctivitis and thimerosal keratoconjunctivitis, signs of disease may persist for months or years even though the symptoms improve rapidly after discontinuing CL wear.
TABLE 2. Clinical Characteristics of the Principal Causes of Conjunctivitis in Contact Lens Users | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
EPIDEMIOLOGY AND PATHOGENESIS
It is not clear whether bacterial conjunctivitis in cosmetic CL users is an intercurrent event unrelated to the use of CLs or whether CL wear may precipitate bacterial conjunctivitis. The well-established contamination of CL storage cases might be expected to result in an excess of conjunctivitis in CL users, but it is also possible that the ocular surface defenses against infection largely neutralize this potential. There have been several studies on the conjunctival microbial flora of CL wearers. A common finding has been a decreased frequency of positive cultures from the eyes of CL wearers compared with controls. These flora have usually been reported as qualitatively unchanged from those in normal eyes or in eyes before lens wear.17,18,19,20,21 However, an increase in gram-negative organisms has been shown in both RCL21 and SCL22 users. Contamination of the lens care materials was shown in only one of the studies.22 The decreased frequency of positive cultures reported in CL wearers has been ascribed to better hygiene during the study period and the effect of antimicrobial lens solutions, introduced by the CLs, on the resident flora in the conjunctival sac.
Prosthetic CL wear, on the other hand, has been associated with bacterial conjunctivitis. Conjunctival cultures from prosthetic CL users show a higher prevalence of bacteria and an increase in the proportion of gram-negative organisms.23 This may be related to a reduced standard of hygiene in prosthetic CL users. Viral keratoconjunctivitis may be transmitted by hand-to-eye contact, upper respiratory droplet infection, or contaminated solutions. Adenovirus conjunctivitis may be transmitted by all three routes but has not been identified as a particular hazard of cosmetic or prosthetic CL wear; there have been few studies of viral contamination of CL care materials. CL fitting carries a risk of transmitting viral as well as bacterial infection, including human immunodeficiency virus type 1 (HIV-1) which has been isolated from both the tears and ocular surface cells of AIDS patients, although HIV infection via this route has never been demonstrated.24 However, most lens care regimens are probably effective against HIV-1,25 although not necessarily against adenoviruses.26 Soft trial lenses are no longer reused in the United Kingdom (UK) because of theoretical risks for the transmission of variant Creutzfeld-Jacob disease (vCJD). Hard trial lenses can be disinfected in hydrogen peroxide 3%, which is probably effective against vCJD as well as viral infection.27
Cosmetic and prosthetic CL use has not been shown to result in any modification of the pathogenesis of microbial conjunctivitis, with the possible exception of chlamydial conjunctivitis. The latter has been reported in a series of 20 CL users who had a mild follicular conjunctivitis without the hyperemia or conjunctival discharge usually associated with this condition.28
MICROBIAL KERATITIS
Microbial keratitis is defined as corneal inflammation due to the presence of replicating organisms. The characteristic appearance is the result of focal corneal inflammation as a response to the presence of organisms. However, this appearance is non-specific and often occurs in the absence of infection. The difficulty of differentiating, either clinically or with laboratory investigations, between corneal ulcers due to replicating organisms (MK) and corneal ulcers resulting from hypersensitivity responses to a variety of stimuli (sterile keratitis) has led to controversy that has been compounded by the terminology. The terms ulcerative keratiti29 and presumed microbial keratitis4 describe keratitis that is probably due to replicating organisms, but in which laboratory investigations may have been negative. A heterogeneously named collection of conditions (summarized in Table 3) describes focal keratitis in CL users that is nonprogressive and probably the result of a hypersensitivity response initiated by the presence of microorganisms. The terms peripheral sterile ulcers,30 sterile corneal infiltrates,31,32 and contact lens induced peripheral corneal ulcers,33 refer to focal keratitis lesions either with or without epithelial involvement or with minimal ulceration, whereas the terms peripheral corneal infiltrates34 and infiltrative keratitis (IK) which may be asymptomatic33 refer to similar symptomatic lesions but without corneal epithelial defects. In these conditions there is no evidence of replicating organisms. In this chapter, microbial keratitis (MK) is used to describe keratitis resulting from invasion by replicating microorganisms, and CL-associated sterile keratitis (CLASK) describes keratitis due to other causes.
TABLE 3. Definition of Microbial Keratitis and Aseptic Keratitis With Distinguishing Clinical Characteristics | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||
DISTINGUISHING INFECTIVE FROM OTHER CAUSES OF KERATITIS
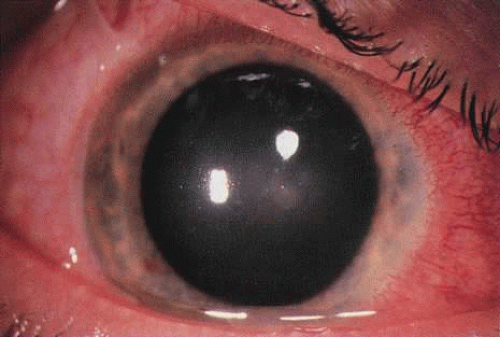
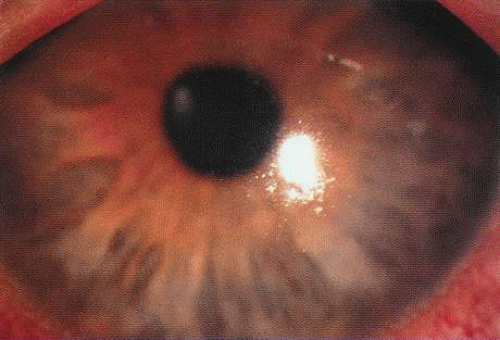
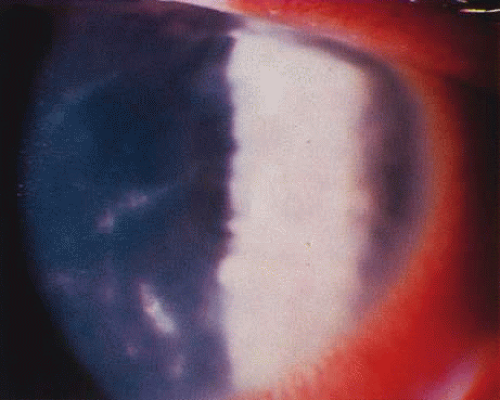
Differentiating MK from CLASK is important both because the management of the individual patient is quite different for the two disorders and because a satisfactory case definition is critical to the study of these different diseases. Current laboratory techniques cannot be reliably used to differentiate microbial from sterile keratitis. CLASK is a diagnosis of exclusion, both because there are no laboratory investigations to substantiate the different causes, and because microbiologic investigation in CLASK has a low sensitivity. It is well established that a negative corneal culture cannot be used to eliminate a microbial cause or, conversely, to validate a sterile cause. Large series of MK cases have documented a culture-positive rate of 50% in in-patient populations comprising the more severe cases,35 whereas a high proportion of CLASK cases are small lesions that may be expected to be culture positive less often. Negative culture results from microbial lesions may occur for several reasons: small volumes of infected material are available for culture, viable organisms present in deep tissues are less available to corneal sampling methods, and pretreatment with antibiotics reduces the viability of invading organisms. For these reasons, clinical criteria have to be used both for the diagnosis of individual patients and in studies designed to investigate these disorders. The size and position of the lesion and presence or absence of an epithelial defect31 are not diagnostic, although these criteria alone have often been used to attempt to differentiate the lesions. The clinical criteria that may be used to differentiate these lesions are summarized in Table 331,32 and illustrations of the lesions are shown in Figures 1, 2, 3, and 4. The use of clinical criteria has been supported by epidemiologic data showing that these definitions can distinguish between distinct disease processes.36
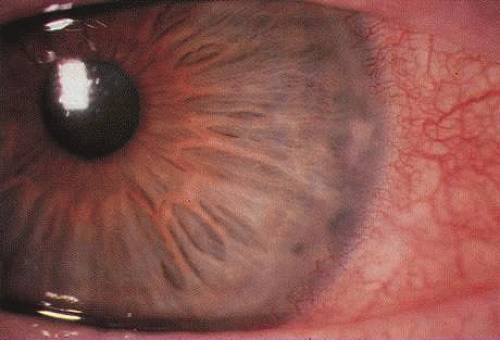 Fig. 1. A contact lens–associated sterile infiltrative keratitis (CLSIK) without an epithelial defect showing a common peripheral arcuate morphology. |
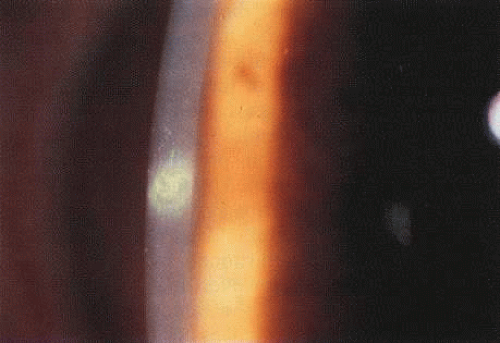 Fig. 2 Contact lens-asociated sterile ulcerative keratitis (CLSUK) showing a typical focal lesion with an epithelial defect. |
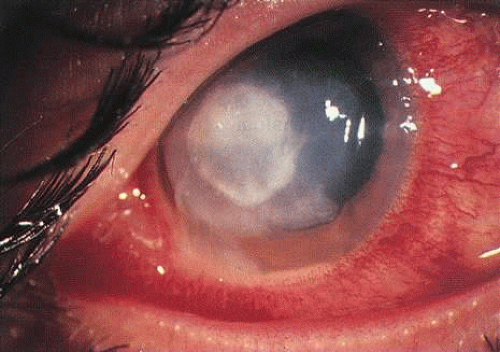 Fig. 4. Established Pseudomonas keratitis with a corneal abscess. The onset of symptoms was 3 days earlier. |
There is only sparse literature on keratitis associated with prosthetic CL use or the use of therapeutic CLs (TCLs). It is a reasonable assumption that those aspects of the epidemiology, pathogenesis and prevention of keratitis in prosthetic CL users that are determined by the materials, wearing pattern, and lens care systems will be similar to those in cosmetic CL userses. However, aspects determined by the ocular response to lens wear will be modified in unpredictable ways by the effects of prosthetic and therapeutic lenses on already abnormal ocular tissues. The following discussion refers principally to cosmetic CL wear although separate reference is made, where appropriate, to special considerations for prosthetic and therapeutic CL wear.
EPIDEMIOLOGY
Epidemiology is the study of the distribution and determinants of disease in a population. Epidemiologic studies have made a substantial contribution to our knowledge both of predisposing causes and of some of the factors to be considered in the pathogenesis of MK, particularly in CL wearers. Until the use of CLs became widespread as an alternative to spectacles, MK occurred in eyes with disrupted ocular defence mechanisms. The most important causes were corneal trauma and surgery, post-herpetic corneal disease, bullous keratopathy, corneal anaesthesia, corneal exposure, and the dry eye. CL wearers made up only a small proportion of patients with this disease.37,38,39 In the 1980s the number of CL users grew and the proportion of MK cases attributed to CL wear rose to over 50% in some centers,3,5,40,41 making CL wear one of the major predisposing factors for MK in some populations. This problem has been of concern because, unlike other causes, it can be avoided and is potentially preventable.
Pathogenic Organisms in Therapeutic Contact Lens Users
TCL users are affected by a spectrum of organisms that differs from those affecting other contact lens users.5,41,42 Pseudomonas is a relatively rare cause of infection TCL users, whereas gram-positive organisms, particularly Streptococci, are common. Candida and other fungi,43 as well as unusual bacteria, are relatively frequent causes of keratitis in this group.44
Pathogenic Organisms in Cosmetic Contact Lens Users
In cosmetic CL users, bacteria and free-living amoebae are the principal causes of keratitis. It is an unfortunate accident of nature that Pseudomonas is one of the most virulent pathogens that can invade the cornea and Acanthamoeba among the most difficult to eliminate.
BACTERIA
Bacterial infections predominate. However, polymicrobial infections are common and consist of any combination of bacterial types. Less often, bacterial keratitis may be combined with fungi, amebae, and herpesvirus. Descriptive studies and keratitis case series have shown that gram-negative bacterial infections predominate in cosmetic CL wear. Pseudomonas is the commonest organism (see Figs. 3 and 4) followed by gram-positive infections with Staphylococcus aureus and S epidermidis. Serratia is also frequently isolated with other gram-negative enterobacteria, including Escherichia coli.45
ACANTHAMOEBA
One of the most astounding developments in ocular microbiology in the last 15 years has been the emergence of Acanthamoeba as an important pathogen in CL users. Figures 5 and 6 show the early stages of Acanthamoeba keratitis. Before 1986 only 31 cases were reported to the Centers for Disease Control in the U.S., whereas in a 9-month period in 1986, 24 cases, 20 of which were CL-associated.46 The number of cases increased to about 200 by 1989; it was proposed that the increase partly resulted from the growth in popularity of CL wear,47 which is associated with Acanthamoeba infection in about 85% of cases.
The highest reported numbers of Acanthamoeba keratitis cases are from the UK, possibly as the result of the widespread use of domestic tank-stored water supplies in which the organism can proliferate.48 Acanthamoeba keratitis increased in the UK in the early 1990s, with one major center reporting 20 cases from 1984 to 1989, rising to 162 cases for the period 1990 to 1995.49,50 In Europe, the disease is possibly rarer, under-diagnosed, or under-reported.51,52
FUNGI
Although fungi can contaminate the lens case and have the potential to invade soft lens materials, they have rarely been implicated as a cause of MK in CL users. It is likely that CL use has a minimal effect on the predisposition to fungal infection. Fusarium, Curvularia, and Paecilomyces have been reported.43,53 Fungal infection has also been reported in daily disposable and planned replacement SCL users.54,55
Table 4 summarizes some case series of keratitis and is divided into two periods; up to 1987,40,42,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75 when Acanthamoeba was infrequently reported in CL users and when the range of CL types available was limited, and from 1988,54,55,76,77,78,79 when Acanthamoeba keratitis was reported in greater numbers at the same time that a wider range of lens types became available. Currently the proportion of CL keratitis cases resulting from Acanthamoeba keratitis varies from 5% to 25% of all culture-positive cases.76,77,78,79
TABLE 4. Summary of Case Series of Keratitis in Contact Lens Users 1960–2001 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
HERPESVIRUS, RARE BACTERIAL CAUSES, AND MICROSPORIDIA
Herpetic keratitis has not been associated with or apparently modified by CLs wear, although it is frequently misdiagnosed in CL users with amoebic keratitis, some of whom may have both conditions concurrently.80 Most of the rare bacterial causes of keratitis have been isolated from CL users, including Nocardia asteroides in EW SCL users,81 atypical mycobacteria in both RCL and SCLusers,82,83 and Microsporidia in an immunocompetent CL user.84 The importance of these uncommon associations is to be aware that CL users, like other patients, may be infected by a range of organisms; when the disease course is atypical, clinicians should be alert to the possibility of a less common cause. For example, the cases of fungal ring infiltrates in disposable CL wearers were initially mistaken for Acanthamoeba infection.55
Measuring the Incidence and Risks of Keratitis
Information about the incidence and risks of serious complication of CLs wear is needed both to ensure that lenses and lens care systems are safe and to give users and practitioners information that will allow them to make informed choices about the risks and benefits of different lens types and care systems. There is now heightened awareness of the potential problems associated with the use of different modalities of CL wear since the identification of the increased risks of extended wear in 1989 and 199085,86 and publication ofstudies showing increased, and largely avoidable, risks for Acanthamoeba keratitis in planned replacement DW SCL users.87
Information has come from a number of sources: national surveys, clinical trials, descriptive studies, population-based incidence studies, and case control studies. All these study designs have limitations that must be understood to interpret the data. National surveys have been limited by incomplete ascertainment of the cases and the size of the population at risk. Many small, prospective cohort studies of complications of different types of lens wear have usually been carried out as clinical trials. This design is generally inappropriate for the study of rare conditions because the size of the cohort may need to be too large to be practical. This has sometimes been taken to mean that the problem is too infrequent to be of concern. However, this is not the case when there is a very large population exposed or when the disease, like keratitis, may be severe. The limitations of this study design have often been overlooked when it has been used to assess the potential of CLs for keratitis and when data from clinical trials have provided little information about the risks for keratitis. For these reasons, descriptive studies in the form of the case reports and case series summarized in Table 4, rather than clinical trials, first identified the probability that there was an increased risk of keratitis associated with some CL types. Recently, the case control study design has been used to overcome some of the problems of clinical trials and to resolve the uncertainties arising from the results of descriptive studies in the assessment of risk for rare complications like keratitis. The case control study is ideally suited to investigating whether there are differences in risks among CL types, allowing comparison of new types of lens and lens-wearing regimens with those for which the level of risk is better established. The advantages and disadvantages of these different study designs have been reviewed.88 Case control studies have provided quantitative data on differences in risk for different lens types and other causes of keratitis. They have also been used to investigate, by multivariable analysis, the influence of additional factors that are associated with the use of different lens types and which might contribute to the risk of keratitis. The data derived from these different approaches to quantifying risk and incidence are describedin the following section.
Incidence and Risks of Keratitis in Groups with Medical Indications for Contact Lens wear
The incidence of keratitis in these groups has to be considered separately from that associated with cosmetic CL wear because of differences in the age of the users, characteristics of the lens, and differences in the ocular tissues which may affect the predisposition to keratitis.
Aphakic CLs users are usually elderly; the high plus power that is required in the lenses reduces the oxygen transmission; and corneal sensation and corneal metabolism are affected by cataract surgery. Because the number of patients at risk has been relatively small and the optical benefits of CL wear, as opposed to aphakic spectacle wear, is so great, keratitis in aphakic CL users has received relatively little attention. There have been a number of clinical trials evaluating aphakic CLs, most of which included a few cases of keratitis, unlike the similar studies carried out for the evaluation of cosmetic CLs. These studies showed an incidence of 0% to 6% during various follow-up periods.89,90,91,92,93,94 The numbers in these clinical trials were too small to establish a precise estimate for the incidence but these studies confirmed the clinical impression that it is relatively high compared to that for cosmetic CL use.
The most precise figures for the incidence of ulcerative keratitis in aphakic lens wear come from a population-based incidence study95 in which the overall annualized incidence for aphakic lens wear was estimated at 52:10,000 with a 7 times higher risk for extended wear compared to daily wear and 6 to 8 times greater risks for aphakic lens wear compared to cosmetic DW SCLs.
For TCL users the risk of infection is known to be high because of the abnormal ocular environment predisposing to infection.96,97,98 As outlined above, this group of CL users is affected by a different spectrum of organisms than other CL users, compared to whom TCL users have fewer gram-negative infections and a higher incidence of keratitis due to fungi, streptococci, and uncommon bacterial opportunists. Patients using these lenses for the management of bullous keratopathy and neurotrophic keratitis are frequently affected.44 In one study of TCLs for bullous keratopathy four of 30 patients developed keratitis.99
Incidence of Microbial Keratitis in Cosmetic Contact Lens Users
National surveys of CL-related disease have been carried out in both the UK and the U.S. In 1960 a postal survey of U.S. ophthalmologists documented six out of 49,950 eyes blinded from ulcerative keratitis associated with RCL wear in one year. Although no other cases were recorded, some with a better outcome did occur.56 In 1976, 13 cases of corneal infections were recorded in a postal survey of 54 consultant ophthalmologists in the UK over a 3-month period100 when the population of CL users could be only approximately estimated at 250,000. More recent and more precise estimates of the incidence of MK in CL users come from analysis of the pooled results of 48 consecutive pre-market approval studies (clinical trials) for the U.S. Food and Drug Administration, providing annualized incidence rates for keratitis of 6.8:10,000 for DW GPCL use, 5.2:10,000 for DW SCL use, and 18.2:10,000 for reusable EW SCL use.101 These studies were carefully carried out but were not comparative. They were conducted on carefully monitored volunteer users who had given informed consent, with individuals who failed to adhere to the follow-up schedules often excluded. For these reasons, such trials may not be representative of the population of CL users in the real post-marketing situation. Although the information provided by these studies is valuable, the individual studies were too small to give precise estimates of the incidence of keratitis in CL users. As a result, neither the licensing authorities nor CL practitioners were aware of the risks for keratitis associated with the use of EW SCLs.
The problems associated with the interpretation of these data have been successfully addressed in a population-based survey for estimating the incidence of ulcerative keratitis associated with CL wear in New England. This study estimated an annual incidence of ulcerative keratitis in the U.S. of 20.9:10,000 for EW SCL use compared to 4.1:10,000 for DW SCL use.102 The study did not have the power to identify differences between rigid and soft lens types.
A more recent well-designed national study from the Netherlands77 is remarkable in that it demonstrated the same incidence and risks for keratitis in GP, DW, and EW-SCLs that were demonstrated by the studies in the U.S. and the UK 10 years previously.4,29,102 This study is the only incidence study to date that included planned replacement SCL users; although the number of DW SCL users in this category was not reported, almost all the EW SCL users were on 1- to 2-week replacement schedules and were likely to have been using these lenses as disposable lenses. These studies are summarized in Table 5.
TABLE 5. Summary of Studies of Annualized Incidence of Microbial Keratitis and Acanthamoeba Keratitis in Cosmetic Contact Lens Wear | ||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree