Conjunctiva/Sclera/Iris/External Disease
5.1 ACUTE CONJUNCTIVITIS
Symptoms
“Red eye” (conjunctival hyperemia), discharge, eyelids sticking or crusting (worse in the morning), foreign body sensation, <4-week duration of symptoms (otherwise, see 5.2, Chronic Conjunctivitis) (see Figure 5.1.1).
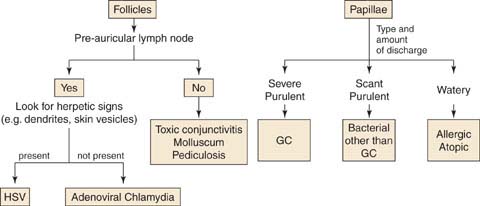
FIGURE 5.1.1. Algorithm for follicles and papillae.
See 8.9, Ophthalmia Neonatorum (Newborn Conjunctivitis), for detailed discussion of acute conjunctivitis in the newborn.
VIRAL CONJUNCTIVITIS/EPIDEMIC KERATOCONJUNCTIVITIS
Symptoms
Itching, burning, tearing, gritty, or foreign body sensation; history of recent upper respiratory tract infection or sick contact. Often starts in one eye and involves the fellow eye a few days later.
Signs
(See Figure 5.1.2.)
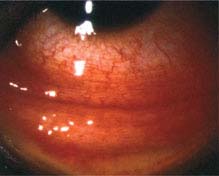
FIGURE 5.1.2. Viral conjunctivitis.
Critical. Inferior palpebral conjunctival follicles (see Figure 5.1.3), tender palpable preauricular lymph node.
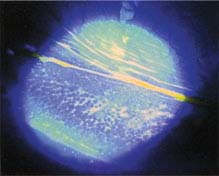
FIGURE 5.1.3. Follicles on the inferior palpebral conjunctiva.
Other. Watery discharge, red and edematous eyelids, pinpoint subconjunctival hemorrhages, punctate keratopathy (epithelial erosion in severe cases), membrane/pseudomembrane (see Figure 5.1.4). Intraepithelial microcysts are an early corneal finding which, if present, can be helpful in diagnosis. Subepithelial infiltrates (SEIs) can develop several weeks after the onset of the conjunctivitis.
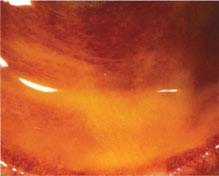
FIGURE 5.1.4. Viral conjunctivitis with pseudomembranes.
Etiology and Variants of Viral Conjunctivitis
 Most commonly adenovirus.
Most commonly adenovirus.
 Pharyngoconjunctival fever: Associated with pharyngitis and fever; usually in children.
Pharyngoconjunctival fever: Associated with pharyngitis and fever; usually in children.
 Acute hemorrhagic conjunctivitis: Associated with a large subconjunctival hemorrhage, coxsackie and enterovirus, 1 to 2 weeks duration. Tends to occur in tropical regions.
Acute hemorrhagic conjunctivitis: Associated with a large subconjunctival hemorrhage, coxsackie and enterovirus, 1 to 2 weeks duration. Tends to occur in tropical regions.
NOTE: Many systemic viral syndromes (e.g., measles, mumps, influenza) can cause a nonspecific conjunctivitis. The underlying condition should be managed appropriately; the eyes are treated with artificial tears four to eight times per day. If tears are used greater than four times daily, preservative-free unit-dose tears should be used.
Work-Up
No conjunctival cultures/swabs are indicated unless discharge is excessive or the condition becomes chronic (see 5.2, Chronic Conjunctivitis).
Treatment
1. Counsel the patient that viral conjunctivitis is a self-limited condition that typically gets worse for the first 4 to 7 days after onset and may not resolve for 2 to 3 weeks or longer with corneal involvement.
2. Viral conjunctivitis is highly contagious, usually for 10 to 12 days from onset, as long as the eyes are red (when not on steroids). Patients should avoid touching their eyes, shaking hands, sharing towels or pillows, etc. Restrict work and school for patients with significant exposure to others while the eyes are red and weeping.
3. Frequent handwashing.
4. Preservative-free artificial tears four to eight times per day for 1 to 3 weeks. Use single-use vials to limit tip contamination and spread of the condition.
5. Cool compresses several times per day.
6. Antihistamine drops (e.g., epinastine 0.05% b.i.d.) if itching is severe.
7. If a membrane/pseudomembrane present, it may be gently peeled or left.
8. If a membrane/pseudomembrane is acutely present or if SEIs reduce vision later, use topical steroids. For membranes/pseudomembranes, use a more frequent steroid dose or stronger steroid (e.g., loteprednol 0.5% q.i.d.) and consider a steroid ointment (e.g., fluorometholone 0.1% ointment q.i.d. or dexamethasone/tobramycin 0.1%/0.3% ointment q.i.d.) in the presence of significant tearing to maintain longer medication exposure. For SEIs, a weaker steroid with less frequent dosing is usually sufficient (e.g., loteprednol 0.2% b.i.d.). Given the possible side effects, prescription of topical steroids is cautionary in the emergency room setting or in patients with questionable follow-up. Steroids may hasten the resolution of the symptoms but prolong the infectious period. Steroid treatment is maintained for 1 week and then slowly tapered. SEIs can recur during or after tapering.
NOTE: Routine use of topical antibiotics for viral conjunctivitis is discouraged unless erosions are present or in severe cases.
Follow-Up
In 2 to 3 weeks, but sooner if the condition worsens significantly or if topical steroids are prescribed.
HERPES SIMPLEX VIRUS CONJUNCTIVITIS
See 4.15, Herpes Simplex Virus, for a detailed discussion. Patients may have a history of perioral cold sores. Manifests with a unilateral (sometimes recurrent) follicular conjunctival reaction, palpable preauricular node, and, occasionally, concurrent herpetic skin vesicles along the eyelid margin or periocular skin. Treat with antiviral therapy (e.g., trifluridine 1% drops or ganciclovir 0.05% gel five times per day) and cool compresses. Steroids are contraindicated.
ALLERGIC CONJUNCTIVITIS
Symptoms
Itching, watery discharge, and a history of allergies are typical. Usually bilateral.
Signs
(See Figure 5.1.5.)
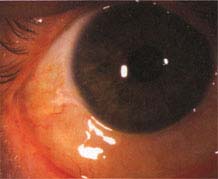
FIGURE 5.1.5. Allergic conjunctivitis.
Chemosis, red and edematous eyelids, conjunctival papillae, no preauricular node.
Treatment
1. Eliminate the inciting agent. Frequent washing of hair and clothes may be helpful.
2. Cool compresses several times per day.
3. Topical drops, depending on the severity.
—Mild: Artificial tears four to eight times per day.
—Moderate: Use olopatadine 0.1% to 0.2%, epinastine 0.05%, nedocromil 2%, bepotastine 1.5%, or ketotifen 0.025% (over-the-counter) b.i.d. to help relieve itching. Ketorolac 0.5%, pemirolast 0.1%, and lodoxamide 0.1% q.i.d. can also reduce symptoms.
—Severe: Mild topical steroid (e.g., loteprednol 0.2% or fluorometholone 0.1% q.i.d. for 1 to 2 weeks) in addition to the preceding medications.
4. Oral antihistamine (e.g., diphenhydramine 25 mg p.o. t.i.d. to q.i.d. or loratadine 10 mg p.o. q.d.) in moderate-to-severe cases can be very helpful.
NOTE: Routine use of topical antibiotics or steroids for allergic conjunctivitis is discouraged.
Follow-Up
Two weeks. If topical steroids are used, tapering is required and patients should be monitored for side effects.
VERNAL/ATOPIC CONJUNCTIVITIS
Symptoms
Usually bilateral but possibly asymmetric itching, thick, ropy discharge, especially in boys. Seasonal (spring/ summer) recurrences in vernal, history of atopy in atopic conjunctivitis. Vernal conjunctivitis is usually seen in younger patients.
Signs
Critical. Large conjunctival papillae seen under the upper eyelid or along the limbus (limbal vernal) (see Figure 5.1.6).

FIGURE 5.1.6. Vernal/atopic conjunctivitis with large superior tarsal papillae.
Other. Superior corneal “shield” ulcer (a well-delineated, sterile, gray-white infiltrate), limbal raised white dots (Horner–Trantas dots) of degenerated eosinophils (see Figure 5.1.7), superficial punctate keratopathy (SPK).

FIGURE 5.1.7. Vernal/atopic conjunctivitis with raised white dots of eosinophils along limbus.
Treatment
1. Treat as for allergic except prophylactically use a mast cell stabilizer (e.g., lodoxamide 0.1% q.i.d. or pemirolast 0.1% q.i.d.), or a mast cell stabilizer and/or antihistamine (e.g., nedocromil 2% b.i.d., olopatadine 0.1% b.i.d., ketotifen 0.025%, bepotastine 1.5%, or azelastine 0.05%) for 2 to 3 weeks before the allergy season starts.
2. If a shield ulcer is present, add:
—Topical steroid (e.g., loteprednol 0.5% or prednisolone 1% drops, dexamethasone 0.1% ointment) four to six times per day.
—Topical antibiotic (e.g., erythromycin ointment q.i.d., polymyxin B/bacitracin q.i.d.).
—Cycloplegic agent (e.g., scopolamine 0.25% t.i.d.).
NOTE: Shield ulcers may need to be scraped to remove superficial plaque-like material before re-epithelialization will occur.
3. Cool compresses q.i.d.
4. Consider cyclosporine 0.05% to 2% b.i.d. to q.i.d. if not responding to the preceding treatment. Maximal effect not seen for several weeks.
5. If associated with atopic dermatitis of eyelids, consider tacrolimus 0.03% to 0.1% q.h.s. or b.i.d. (preferred), pimecrolimus 1% b.i.d., or topical steroid ophthalmic ointment (e.g., fluorometholone 0.1% q.i.d.) to the affected skin.
Follow-Up
Every 1 to 3 days in the presence of a shield ulcer; otherwise, every few weeks. Topical medications are tapered slowly as improvement is noted. Antiallergy drops are maintained for the duration of the season and are often reinitiated a few weeks before the next spring. Patients on topical steroids should be monitored regularly, including IOP monitoring, even if used only on the skin.
BACTERIAL CONJUNCTIVITIS (NONGONOCOCCAL)
Symptoms
Redness, foreign body sensation, discharge; itching is much less prominent.
Signs
Critical. Purulent white-yellow discharge of mild-to-moderate degree.
Other. Conjunctival papillae, chemosis, preauricular node typically absent but is often present in gonococcal conjunctivitis.
Etiology
Commonly, Staphylococcus aureus (associated with blepharitis, phlyctenules, and marginal sterile infiltrates), Staphylococcus epidermidis, Haemophilus influenzae (especially in children and commonly associated with otitis media), Streptococcus pneumoniae, and Moraxella catarrhalis.
NOTE: Suspect gonococcus if onset is hyperacute with significant discharge, see this chapter Gonococcal Conjunctivitis.
Work-Up
If severe, recurrent, or recalcitrant, conjunctival swab for routine cultures and sensitivities (blood and chocolate agar) and immediate Gram stain to evaluate for gonococcus.
Treatment
1. Use topical antibiotic therapy (e.g., trimethoprim/polymyxin B or fluoroquinolone drops q.i.d.) for 5 to 7 days.
2. H. influenzae conjunctivitis should be treated with oral amoxicillin/clavulanate (20 to 40 mg/kg/day in three divided doses) because of occasional extraocular involvement (e.g., otitis media, pneumonia, and meningitis).
3. If associated with dacryocystitis, systemic antibiotics are necessary. See 6.9, Dacryocystitis/Inflammation of the Lacrimal Sac.
Follow-Up
Every 2 to 3 days initially, then every 5 to 7 days until resolved. Antibiotic therapy is adjusted according to culture and sensitivity results.
GONOCOCCAL CONJUNCTIVITIS
Signs
Critical. Severe purulent discharge, hyperacute onset (within 12 to 24 hours).
Other. Conjunctival papillae, marked chemosis, preauricular adenopathy, eyelid swelling. See 8.9, Ophthalmia Neonatorum (Newborn Conjunctivitis), for a detailed discussion of gonococcal conjunctivitis in the newborn.
Work-Up
1. Examine the entire cornea for peripheral ulcers (especially superiorly) because of the risk for rapid progression to perforation. (see Figure 5.1.8).

FIGURE 5.1.8. Gonococcal conjunctivitis with corneal involvement.
2. Conjunctival scrapings for immediate Gram stain and for culture and sensitivities (e.g., blood agar and chocolate agar).
Treatment
Initiated if the Gram stain shows Gram-negative intracellular diplococci or there is a high clinical suspicion of gonococcal conjunctivitis.
1. Ceftriaxone 1 g intramuscularly (i.m.) in a single dose. If corneal involvement exists, or cannot be excluded because of chemosis and eyelid swelling, hospitalize the patient and treat with ceftriaxone 1 g intravenously (i.v.) every 12 to 24 hours. The duration of treatment depends on the clinical response. In penicillin-allergic patients, consider an oral fluoroquinolone (e.g., ciprofloxacin 500 mg p.o. b.i.d. for 5 days) and consider consulting an infectious disease specialist (fluoroquinolones are contraindicated in pregnant women and children). Additionally, due to increased resistance, fluoroquinolones should not be used to treat gonococcal infections in men who have sex with men, in areas of high endemic resistance, and in patients with a recent foreign travel history. For penicillin-allergic patients with the above characteristics, one possible treatment alternative is a single dose of azithromycin 1 g p.o. An infectious disease consultation should be considered.
2. Topical ciprofloxacin ointment q.i.d. or ciprofloxacin drops q2h. If the cornea is involved, use a fluoroquinolone drop q1h (e.g., gatifloxacin, moxifloxacin, besifloxacin, levofloxacin, or ciprofloxacin).
3. Saline irrigation q.i.d. until the discharge resolves.
4. Treat for possible chlamydial coinfection (e.g., azithromycin 1 g p.o. single dose or doxycycline 100 mg p.o. b.i.d. for 7 days).
5. Treat sexual partners with oral antibiotics for both gonorrhea and chlamydia as described previously.
Follow-Up
Daily until consistent improvement is noted and then every 2 to 3 days until the condition resolves. The patient and sexual partners should be evaluated by their medical doctors for other sexually transmitted diseases.
PEDICULOSIS (LICE, CRABS)
Typically develops from contact with pubic lice (usually sexually transmitted). Can be unilateral or bilateral.
Symptoms
Itching, mild conjunctival injection.
Signs
(See Figure 5.1.9.)

FIGURE 5.1.9. Pediculosis.
Critical. Adult lice, nits, and blood-tinged debris on the eyelids and eyelashes.
Other. Follicular conjunctivitis.
Treatment
1. Mechanical removal of lice and eggs with jeweler’s forceps.
2. Any bland ophthalmic ointment (e.g., erythromycin) to the eyelids t.i.d. for 10 days to smother the lice and nits.
3. Antilice lotion and shampoo as directed to nonocular areas for patient and close contacts.
4. Thoroughly wash and dry all clothes and linens.
NOTE: In children, pediculosis is suspicious for possible sexual abuse and involvement of social services and/or child protection agency is recommended.
For chlamydial, toxic, and molluscum contagiosum-related conjunctivitis, see 5.2, Chronic Conjunctivitis.
Also see related sections: 8.9, Ophthalmia Neonatorum (Newborn Conjunctivitis); 13.6, Stevens–Johnson Syndrome (Erythema Multiforme Major); and 5.10, Ocular Cicatricial Pemphigoid.
5.2 CHRONIC CONJUNCTIVITIS
Symptoms
“Red eye” (conjunctival hyperemia), conjunctival discharge, eyelids sticking (worse in morning), foreign body sensation, duration >4 weeks (otherwise see 5.1, Acute Conjunctivitis).
Differential Diagnosis
 Parinaud oculoglandular conjunctivitis (see 5.3, Parinaud Oculoglandular Conjunctivitis).
Parinaud oculoglandular conjunctivitis (see 5.3, Parinaud Oculoglandular Conjunctivitis).
 Silent dacryocystitis (see 6.9, Dacryocystitis/Inflammation of the Lacrimal Sac).
Silent dacryocystitis (see 6.9, Dacryocystitis/Inflammation of the Lacrimal Sac).
 Contact lens-related (see 4.21, Contact Lens-Related Problems).
Contact lens-related (see 4.21, Contact Lens-Related Problems).
 Conjunctival tumors (see 5.12, Conjunctival Tumors).
Conjunctival tumors (see 5.12, Conjunctival Tumors).
 Autoimmune disease (e.g., reactive arthritis, sarcoidosis, discoid lupus, others).
Autoimmune disease (e.g., reactive arthritis, sarcoidosis, discoid lupus, others).
CHLAMYDIAL INCLUSION CONJUNCTIVITIS
Sexually transmitted, typically found in young adults. A history of vaginitis, cervicitis, or urethritis may be present.
Signs
Inferior tarsal or bulbar conjunctival follicles, superior corneal pannus, palpable preauricular node, or peripheral SEIs. A stringy, mucous discharge may be present.
Work-Up
1. History: Determine the duration of red eye, any prior treatment, concomitant vaginitis, cervicitis, or urethritis. Sexually active?
2. Slit-lamp examination.
3. In adults, direct chlamydial immunofluorescence test, DNA probe, chlamydial culture of conjunctiva, or polymerase chain reaction when available.
NOTE: Topical fluorescein can interfere with immunofluorescence test results.
4. Consider conjunctival scraping for Giemsa stain: Shows basophilic intracytoplasmic inclusion bodies in epithelial cells, polymorphonuclear leukocytes, and lymphocytes in newborns.
Treatment
1. Azithromycin 1 g p.o. single dose, doxycycline 100 mg p.o. b.i.d., or erythromycin 500 mg p.o. q.i.d. for 7 days is given to the patient and sexual partners.
2. Topical erythromycin or tetracycline ointment b.i.d. to t.i.d. for 2 to 3 weeks.
Follow-Up
In 2 to 3 weeks, depending on the severity. The patient and sexual partners should be evaluated by their medical doctors for other sexually transmitted diseases. Occasionally a 6-week course of doxycycline may be required.
TRACHOMA
Principally occurs in developing countries in areas of poor sanitation and crowded conditions.
Signs
(See Figure 5.2.1.)
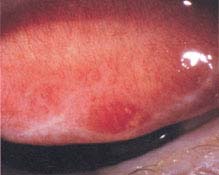
FIGURE 5.2.1. Trachoma showing Arlt line, or scarring, of the surgery tarsal conjunctiva.
MacCallan Classification
 Stage 1: Superior tarsal follicles, mild superior SPK, and pannus, often preceded by purulent discharge and tender preauricular node.
Stage 1: Superior tarsal follicles, mild superior SPK, and pannus, often preceded by purulent discharge and tender preauricular node.
 Stage 2: Florid superior tarsal follicular reaction (2a) or papillary hypertrophy (2b) associated with superior corneal SEIs, pannus, and limbal follicles.
Stage 2: Florid superior tarsal follicular reaction (2a) or papillary hypertrophy (2b) associated with superior corneal SEIs, pannus, and limbal follicles.
 Stage 3: Follicles and scarring of superior tarsal conjunctiva.
Stage 3: Follicles and scarring of superior tarsal conjunctiva.
 Stage 4: No follicles, extensive conjunctival scarring.
Stage 4: No follicles, extensive conjunctival scarring.
 Late complications: Severe dry eyes, trichiasis, entropion, keratitis, corneal scarring, superficial fibrovascular pannus, Herbert pits (scarred limbal follicles), corneal bacterial superinfection, and ulceration.
Late complications: Severe dry eyes, trichiasis, entropion, keratitis, corneal scarring, superficial fibrovascular pannus, Herbert pits (scarred limbal follicles), corneal bacterial superinfection, and ulceration.
World Health Organization Classification
 TF (trachomatous inflammation: follicular): More than five follicles on the upper tarsus.
TF (trachomatous inflammation: follicular): More than five follicles on the upper tarsus.
 TI (trachomatous inflammation: intense): Inflammation with thickening obscuring >50% of the tarsal vessels.
TI (trachomatous inflammation: intense): Inflammation with thickening obscuring >50% of the tarsal vessels.
 TS (trachomatous scarring): Cicatrization of tarsal conjunctiva with fibrous white bands.
TS (trachomatous scarring): Cicatrization of tarsal conjunctiva with fibrous white bands.
 TT (trachomatous trichiasis): Trichiasis of at least one eyelash.
TT (trachomatous trichiasis): Trichiasis of at least one eyelash.
 CO (corneal opacity): Corneal opacity involving at least part of the pupillary margin.
CO (corneal opacity): Corneal opacity involving at least part of the pupillary margin.
Work-Up
1. History of exposure to endemic areas (e.g., North Africa, Middle East, India, Southeast Asia).
2. Examination and diagnostic studies as above (chlamydial inclusion conjunctivitis).
Treatment
1. Azithromycin 20 mg/kg p.o. single dose, doxycycline 100 mg p.o. b.i.d., erythromycin 500 mg p.o. q.i.d., or tetracycline 250 mg p.o. q.i.d. for 2 weeks.
2. Tetracycline, erythromycin, or sulfacetamide ointment b.i.d. to q.i.d. for 3 to 4 weeks.
NOTE: Tetracyclines are contraindicated in children younger than 8 years, pregnant women, and nursing mothers.
Follow-Up
Every 2 to 3 weeks initially, then as needed. Although treatment is usually curative, reinfection is common if hygienic conditions do not improve.
NOTE: Currently, the World Health Organization is conducting a large-scale program to eradicate trachoma through intermittent widespread distribution of azithromycin as well as information on facial cleanliness and water sanitation to endemic areas. The aim is global elimination of blindness caused by trachoma by the year 2020.
MOLLUSCUM CONTAGIOSUM
Signs
Critical. Dome shaped, usually multiple, umbilicated shiny nodules on the eyelid or eyelid margin.
Other. Follicular conjunctival response from toxic viral products, corneal pannus. Immunocompromised patients may have more lesions and less conjunctival reaction.
Treatment
Removal of lesions by simple excision, incision and curettage, or cryosurgery.
Follow-Up
Every 2 to 4 weeks until the conjunctivitis resolves, which often takes 4 to 6 weeks. If many lesions are present, consider human immunodeficiency virus (HIV) testing.
MICROSPORIDIAL KERATOCONJUNCTIVITIS
Signs
Chronic superficial punctate keratitis and conjunctival injection not responsive to conservative treatment. Diagnosed with Giemsa stain of corneal or conjunctival scraping.
Treatment
Topical fumagillin and/or oral itraconazole 200 mg p.o. q.d. Epithelial debridement followed by antibiotic ointment (e.g., erythromycin or bacitracin/polymyxin B t.i.d.) may be useful for mild cases. Treat underlying disease. Consider HIV testing.
TOXIC CONJUNCTIVITIS/MEDICAMENTOSA
Signs
Inferior papillary reaction and/or inferior conjunctival staining with fluorescein from topical eye drops. Most notably from aminoglycosides, antivirals, and preserved drops. With long-term use, usually more than 1 month, a follicular response can be seen with other medications including atropine, brimonidine, miotics, epinephrine agents, antibiotics, and antivirals. Inferior SPK and scant discharge may be noted.
Treatment
Usually sufficient to discontinue the offending eye drop. Can add preservative-free artificial tears four to eight times per day.
Follow-Up
In 1 to 4 weeks, as needed.
5.3 PARINAUD OCULOGLANDULAR CONJUNCTIVITIS
Symptoms
Red eye, mucopurulent discharge, foreign body sensation.
Signs
Critical. Granulomatous nodule(s) on the palpebral conjunctiva; visibly swollen ipsilateral, preauricular, or submandibular lymph nodes.
Other. Fever, rash, follicular conjunctivitis.
Etiology
 Cat-scratch disease from Bartonella henselae (most common cause): Often a history of being scratched or licked by a kitten within 2 weeks of symptoms.
Cat-scratch disease from Bartonella henselae (most common cause): Often a history of being scratched or licked by a kitten within 2 weeks of symptoms.
 Tularemia: History of contact with rabbits, other small wild animals, or ticks. Patients have severe headache, fever, and other systemic manifestations.
Tularemia: History of contact with rabbits, other small wild animals, or ticks. Patients have severe headache, fever, and other systemic manifestations.
 Tuberculosis and other mycobacteria.
Tuberculosis and other mycobacteria.
 Rare causes: Syphilis, leukemia, lymphoma, mumps, Epstein–Barr virus, fungi, sarcoidosis, listeria, and others.
Rare causes: Syphilis, leukemia, lymphoma, mumps, Epstein–Barr virus, fungi, sarcoidosis, listeria, and others.
Work-Up
Initiated when etiology is unknown (e.g., no recent cat scratch).
1. Conjunctival biopsy with scrapings for Gram, Giemsa, and acid-fast stains.
2. Conjunctival cultures on blood, Löwenstein–Jensen, Sabouraud, and thioglycolate media.
3. Complete blood count, rapid plasma reagin (RPR), fluorescent treponemal antibody-absorbed (FTA-ABS), angiotensin converting enzyme (ACE), and, if the patient is febrile, blood cultures.
4. Chest radiograph, purified protein derivative (PPD), and anergy panel.
5. If tularemia is suspected, serologic titers are necessary.
6. If diagnosis of cat-scratch disease is uncertain, cat-scratch serology, and cat-scratch skin test (Hanger–Rose) can be performed.
Treatment
1. Warm compresses for tender lymph nodes.
2. Antipyretics as needed.
3. Disease specific:
—Cat-scratch disease: Generally resolves spontaneously in 6 weeks. Consider azithromycin 500 mg p.o. q.i.d., then 250 mg daily for four doses (for children, 10 mg/kg q.i.d., then 5 mg/kg daily for four doses); alternatives include trimethoprim/sulfamethoxazole DS p.o. b.i.d.; or ciprofloxacin 500 mg p.o. b.i.d. Duration should be individualized. Use a topical antibiotic (e.g., bacitracin/polymyxin B ointment or gentamicin drops q.i.d.). The cat does not need to be removed.
—Tularemia: Tobramycin 5 mg/kg/day in three divided doses q8h or gentamicin (same dosing) for 7 to 14 days. Gentamicin drops q2h for 1 week, and then five times per day until resolved. Often patients are systemically ill and under the care of a medical internist for tularemia; if not, refer to a medical internist for systemic management.
—Tuberculosis: Refer to an internist for antituberculosis medication.
—Syphilis: Systemic penicillin (dose depends on the stage of the syphilis) and topical tetracycline ointment (see 12.12, Syphilis).
Follow-Up
Repeat the ocular examination in 1 to 2 weeks. Conjunctival granulomas and lymphadenopathy can take 4 to 6 weeks to resolve for cat-scratch disease.
5.4 SUPERIOR LIMBIC KERATOCONJUNCTIVITIS
Symptoms
Red eye, burning, foreign body sensation, pain, tearing, mild photophobia, frequent blinking. The course can be chronic with exacerbations and remissions.
Signs
(See Figure 5.4.1.)
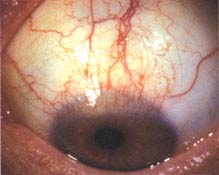
FIGURE 5.4.1. Superior limbic keratoconjunctivitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


