 Conjunctival Lymphoid, Leukemic, and Metastatic Tumors
Conjunctival Lymphoid, Leukemic, and Metastatic TumorsConjunctival Lymphoid and Plasmacytic Tumors
General Considerations
A lymphoid tumor can occur in the conjunctiva as an isolated condition or it can be a manifestation of systemic lymphoma (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20). In the authors’ clinical series of 1,643 conjunctival tumors, there were 128 lymphoid lesions, accounting for 8% of the 1,643 lesions (5). The details of classification, clinical features, histopathologic characteristics, and prognosis are discussed elsewhere (1,2) and are beyond the scope of this chapter. It is traditional to divide lymphoid infiltrates into benign reactive lymphoid hyperplasia (BRLH) and malignant lymphoma. It is not usually possible to differentiate the BRLH and lymphoma clinically; the histopathologic differential is also sometimes difficult. Hence, they are discussed collectively here. In recent years, there has been increasing emphasis on the fact that many conjunctival “lymphomas” are low-grade B-cell lymphomas of the mucosa-associated lymphoid tumor (MALT) type (12). There is also some controversy as to the role of inflammation (conjunctivitis) in the pathogenesis of MALT lymphoma (6). MALT lymphoma is best known to occur in the stomach. The gastric lesion appears to have an association with Helicobacter pylori infection. There is currently an increasing interest in the relationship between conjunctival MALT lymphoma and H. pylori. If such a relationship is established, antibiotics may prove to be the best initial management.
Plasmacytoma and closely related lymphoplasmacytoid tumors can rarely arise in the conjunctiva (1,2,3,4,5,6,7,8,9,10). In a sense, plasmacytoma is a neoplasm that is related to a lymphoma in that the plasma cell is a highly differentiated form type of B lymphocyte (1). Tumors composed of malignant plasma cells are often associated with multiple myeloma, in which cases the disease is manifested mainly in bone. However, soft tissue plasmacytoma can also occur as part of multiple myeloma or as a solitary lesion. Extraskeletal plasmacytoma can occasionally be the first sign of myeloma (21,22,23,24,25,26,27,28,29). Because lymphoma and plasmacytoma are so similar clinically, they are discussed together in this chapter.
Clinical Features
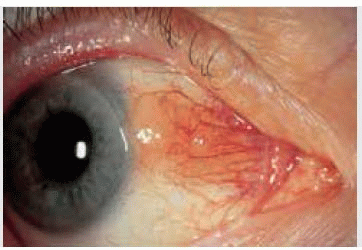
Clinically, a lymphoid tumor is usually a diffuse, slightly elevated fleshy pink mass that has been likened to smoked salmon. It is generally located in the forniceal or bulbar conjunctiva, but occasionally occurs at the limbus. It does not seem to have a predilection for the interpalpebral conjunctiva like squamous cell lesions. It usually has a mild vascular supply, but large dilated conjunctival nutrient vessels can be apparent in larger tumors. Although conjunctival lymphoma usually has a smooth surface, it can have a multinodular appearance and resemble follicular conjunctivitis.
It is not usually possible to differentiate clinically between a benign and malignant lymphoid tumor. Therefore, biopsy is necessary to help establish the diagnosis and a systemic evaluation should be done in all affected patients to exclude the presence of systemic lymphoma. It is also important to counsel the patient with a conjunctival lymphoid infiltrate as to the chances of developing systemic lymphoma. A review of 117 patients who presented with such a conjunctival lesion revealed that 31% had or eventually developed systemic lymphoma overall (11). If the lymphoid infiltrate was unilateral, the chance of systemic lymphoma was 17% and if the lymphoid infiltrate was bilateral the chances for systemic lymphoma were 47%. The authors use these figures in counseling the patient with a conjunctival lymphoid infiltrate. With longer follow-up, it is most likely that a higher percent of affected patients would develop systemic lymphoma.
Pathology
Histopathologically, a lymphoid tumor is composed of solid sheets of lymphocytes and the lesion is classified as BRLH, atypical lymphoid hyperplasia, or malignant lymphoma, depending on the degree of cellular anaplasia The benign and atypical lymphoid hyperplasia are less likely to be associated with systemic lymphoma and the malignant lymphoid tumor is more likely to be associated with systemic lymphoma. Although there is much overlap, BRLH is generally polymorphic, with well-differentiated lymphocytes and plasma cells. In general, lymphoma tends to be more monomorphic. Immunohistochemistry may be helpful in determining whether the lesions are monoclonal or polyclonal. However, it seems that immunohistochemistry has limitations in determining prognosis; many monoclonal lesions may follow a benign clinical course. Most conjunctival lymphomas are non-Hodgkin B-cell lymphomas; Hodgkin lymphoma and T-cell lymphoma affect the conjunctiva less frequently (9).
Management
If the conjunctival lesion is small and circumscribed, an excisional biopsy and supplemental cryotherapy can sometimes be performed and no further treatment may be necessary. If a conjunctival lymphoid lesion is large and cannot be excised completely, we recommend a generous biopsy, histopathologic staging, and then treatment with chemotherapy or radiotherapy. However, we biopsy enough tissue for diagnosis, but not so much as to require grafting. This seems logical since conjunctival lymphoma is sensitive to radiotherapy and wide excision seems unnecessary. Others have suggested that larger lesions should be excised, even if amniotic membrane transplant is necessary to close the defect (8). When the lesion has been biopsied and confirmed histopathologically, more treatment should usually be given. If the patient has systemic lymphoma, then treatment should initially be chemotherapy. Rituximab has been successful in selected cases (19). If the lesion is solitary, with no systemic lymphoma, external beam irradiation is
generally the treatment of choice. All types of lymphoma are particularly sensitive to radiotherapy. The dose of external beam irradiation ranges from 2,000 cGy for benign lesions to 4,000 cGy for more malignant lesions.
generally the treatment of choice. All types of lymphoma are particularly sensitive to radiotherapy. The dose of external beam irradiation ranges from 2,000 cGy for benign lesions to 4,000 cGy for more malignant lesions.
We have seen several patients with low-grade MALT lymphoma of the conjunctiva who had little or no residual tumor after biopsy and who were reluctant to undergo irradiation because they were asymptomatic We have simply observed the lesion in a number of such patients and have been impressed that the majority of them show no progression and the patient remains asymptomatic. A recent report described some patients who actually had regression of the lesion after biopsy only (14). Although it remains controversial, we currently believe that periodic observation may be the preferred treatment in some cases. In patients with extensive residual tumor or with progression after biopsy, however, radiotherapy is generally advisable.
Management of conjunctival plasmacytoma is similar to that for lymphoma. The patient should be evaluated initially and periodically for multiple myeloma and monoclonal gammopathy. The conjunctival lesion can be completely excised if small and localized. Larger, more aggressive lesions respond to irradiation or chemotherapy that is given for the systemic disease (21,22,23,24,25,26,27,28,29).
Selected References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


