Conjunctiva
Alex V. Levin
Thomas W. Wilson
David Rootman
Jerome Kazdan
The conjunctiva is derived from surface ectoderm and has an important role in maintaining ocular surface integrity. Goblet cells within the conjunctiva provide the inner layer of the trilaminar tear film for lubrication and surface wetting. Tumors of the conjunctiva are often benign but must be observed for possible malignant transformation. Conjunctival findings may assist in the diagnosis of systemic diseases, and conjunctival biopsy can be a useful diagnostic tool. As the conjunctival epithelium is contiguous with the corneal epithelium and vascular supply to the limbus is brought in part by the conjunctiva, it is not uncommon for conjunctival disease to coexist with corneal disease or anterior segment inflammation (iritis).
The conjunctiva also extends upward and downward to form the superior and inferior fornices where it reflects out onto the inner surface of the lids. Bulbar conjunctiva, which overlies the globe, may or may not be affected in some disorders. The same is true for palpebral conjunctiva. The fornices may serve as repositories for chemical or particular matter, and therefore, lid eversion is an essential part of complete conjunctival examination. Defects or foreign bodies in the conjunctiva can be detected by topical fluorescein staining, whereas rose bengal can be used to detect devitalized conjunctival epithelial cells.
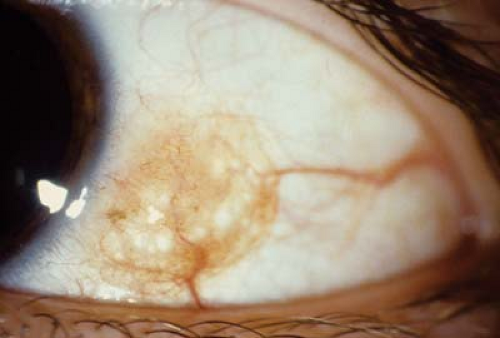
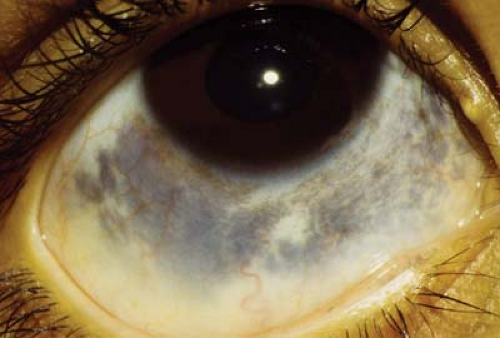 Figure 4.5 Ocular Melanosis Ocular melanosis is a form of episcleral pigmentation, usually slate gray, that tends to occur as broad patches with no anatomic correlate, unlike Axenfeld loops (see Fig. 4.4). This form of episcleral pigmentation is seen in darkly pigmented individuals and is not associated with malignant transformation. The lesions may be uni- or bilateral. Pigmentation does not move with the conjunctiva. |
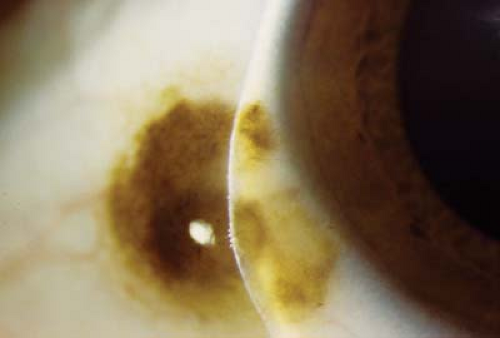
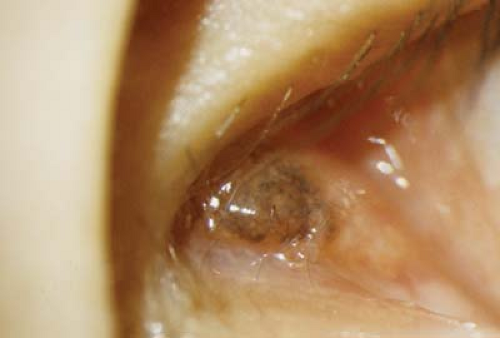
 Figure 4.6 Oculodermal Melanocytosis The combination of ocular melanosis (see Fig. 4.5) and similar skin pigmentation, known as nevus of Ota, is called oculodermal melanocytosis. The skin has a bluish gray appearance. Other uveal structures, including the iris and retinal pigment epithelium, can have increased pigmentation (Fig. 4.7). Nevus of Ota is more common in darkly pigmented individuals and is typically unilateral. It is more common in certain ethnic groups, particularly in far eastern Asia. When found in the Caucasian population it has a higher incidence of associated malignancy, including choroidal melanoma. |
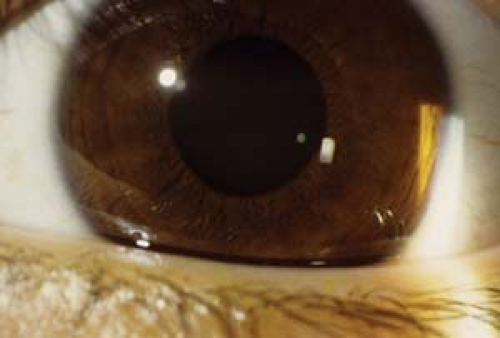 Figure 4.7 Iris Melanosis Iris melanosis is often associated with oculodermal melanocytosis (see Figs. 4.5 and 4.6). The usual iris crypts are missing, particularly in the peripheral two thirds of the iris. Instead, the iris appears flat with or without a large number of tiny bumps following no particular pattern. The iris tends to be chocolate brown, particularly when compared to the other eye. Gonioscopy is normal and there is no increased association with glaucoma. However, eyes with iris melanosis in the presence of oculodermal melanocytosis may have a higher risk of ocular melanoma. Malignant transformation is very rare in childhood.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|