Congenital Malformations of the Eye
Brian P. Brooks
Elias I. Traboulsi
INTRODUCTION
The purpose of this chapter is to give an overview of congenital malformations of the eye and the ocular adnexa, with emphasis on molecular and developmental mechanisms. Detailed reviews of ocular development, teratology, and many of the specific disorders in this chapter can be found elsewhere in this text.
Ocular malformations may have genetic and nongenetic causes (e.g., environmental.) Those with genetic causes may be familial or sporadic. They may be isolated or part of a broader syndrome. In many cases, the exact cause for a given malformation is not known. Depending on the population studied, the method of ascertainment, and the definition of “ocular malformation,” various published studies have found a birth prevalence of ocular malformations of 0.04 to 6.8 per 10,000 live births.12,3,4,5,6,7
The past decade has witnessed a tremendous increase in our understanding of the molecular and developmental causes of many important ophthalmic malformations (Table 1). Many of the mutations that cause ocular malformations are in transcription factors. Transcription factors are proteins that bind to specific DNA sequences (or to proteins that bind to DNA) to regulate expression of specific genes. A complex pattern of gene expression in different parts of the embryo during different times of gestation is required for normal organogenesis and cellular differentiation. Disruption of this process through the alteration of the function of any important transcription factor can have serious consequences. Development can also be affected by changes in cell-to-cell signaling, cell migration, cell death, and cell adhesion.
TABLE 1. Examples of Developmental Eye Diseases Caused by Mutations in Transcription Factors (transcription factors: see text for details and references) | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
This chapter describes malformations on an anatomic basis. However, current classifications and nosology of congenital ocular malformations are imperfect. For example, some abnormalities are difficult to classify because they affect multiple tissues (e.g., aniridia). Sometimes the same word (e.g., coloboma) is used in the literature to describe several distinct clinical and developmental entities. A primary defect in one structure may cause secondary malformations in another (e.g., the small orbits and short palpebral fissures in anophthalmic patients). A given genetic disorder may have a spectrum of presentations (phenotypic heterogeneity). Lastly, different genetic mutations can cause the same clinical phenotype (genetic heterogeneity). We attempt to clarify these sometimes confusing issues on a case-by-case basis.
Because the disorders covered in this chapter are largely developmental, we review the essential embryology behind each class of disease. A detailed discussion of ocular embryology is presented elsewhere in this text. Although we present development in a compartmentalized fashion, it is important to recognize that multiple, interdependent events are occurring simultaneously during embryogenesis. As such, insults or changes in gene expression at one time point may have multiple effects at later time points. For example, maternal alcohol use during the period of gastrulation—days before any ocular structures are visible morphologically—may result in ocular defects ranging from microphthalmia to coloboma to Peters anomaly.8
Throughout this chapter, we refer to “Online Mendelian Inheritance in Man” or OMIM. OMIM is a comprehensive catalog of inherited diseases available free of charge at http://www-ncbi-nlm-nih-gov.easyaccess1.lib.cuhk.edu.hk/omim. When possible, we will provide the OMIM number for individual disorders.
DISORDERS THAT AFFECT THE ENTIRE EYE
DEVELOPMENTAL BIOLOGY91
Eye development becomes evident at approximately 22 days gestation, when the optic sulci appear as bilateral grooves in the neural ectoderm of the embryo. At approximately 25 days gestation, as the rostral neural tube fuses, the neural ectoderm evaginates further to form the optic vesicles. The optic vesicles are attached to the developing brain via the optic stalks. As the optic vesicles grow laterally and approach the surface ectoderm, they invaginate to form a bilayered optic cup. The inner and outer layers of the optic cup proceed to form the neural retina and the retinal pigmented epithelium, respectively. The invaginated optic cup forms a somewhat spherical structure that is open anteriorly and inferiorly. This inferior “seam” is alternatively called the optic fissure, the choroidal fissure, or the embryonic fissure, and it transmits the hyaloid vascular system beginning at approximately 5 weeks gestation. At 6 weeks gestation, the optic fissure “zippers” shut, beginning equatorially and proceeding anteriorly and posteriorly.
ANOPHTHALMIA
Anophthalmia refers to the complete absence of ocular tissue, presumably caused by abnormalities of optic vesicle formation or maturation. Patients may have unilateral or bilateral anophthalmia, and generally have short palpebral fissures and small orbits. In many cases when there is no clinically apparent ophthalmic tissue, remnants of lens epithelium, neuroretinal, and fibrovascular, choroid-like tissue can be detected on histologic sectioning. Terms such as “true anophthalmia,” “extreme microphthalmia,”10 and “clinical anophthalmia”11 have been used in the literature to describe what may be, in truth, a phenotypic continuum between anophthalmia and microphthalmia (see later).
Anophthalmia may be isolated or associated with a broader syndrome (Table 2).12,13,14,15,16,17,18,19 Isolated anophthalmia is generally an autosomal recessive condition.20 Driggers et al. reported a child with isolated bilateral anophthalmia and an apparent balanced chromosomal translocation {46, XX, t(3;11)(q27;p11.2)}.21 Fantes et al. found that this child had, in fact, a submicroscopic deletion that eliminated the SOX2 gene on chromosome 3, and went on to show nonsense mutations in SOX2 in four of 11 subjects with bilateral anophthalmia.22 SOX2 lies within an intron of a nonexpressed gene, SOX2OT, and is expressed in neuroectoderm early in development.23 SOX2 protein interacts cooperatively with PAX6 in the induction of lens development and delta-crystallin expression.24 Hagstrom, Traboulsi et al. found a null mutation in SOX2 in a girl with bilateral clinical anophthalmia and absence of the optic nerves, chiasm, and optic tracts (unpublished data)
TABLE 2. Clinical Syndromes Associated with Anophthalmia | |||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||
Reconstructive surgery can be helpful in patients with congenital anophthalmia.25 Orbital expansion can be achieved with spherical implants, orbital osteotomies, bone grafts, and/or orbital expanders. Conjunctival sac reconstruction is achieved using serial expanders and buccal mucous membrane grafts. Lid reconstruction sometimes requires tissue flaps and skin grafts.
MICROPHTHALMIA
A microphthalmic eye is one with axial length less than two standard deviations below the age-adjusted mean (ie, <19 mm in a 1-year-old child and <21 mm in an adult.) Microphthalmia encompasses a range of phenotypes. Specific terms, outlined later, are applied to subgroups of microphthalmic eyes with certain characteristics. Authors of scientific communications may not use the same classification scheme or may use the more general term “microphthalmia” when a more specific term could apply. Although we will present these terms as distinct entities, remember that they likely represent points along a single, phenotypic continuum.
Simple Microphthalmia/Nanophthalmos
Simple microphthalmia refers to a small but structurally normal eye.26 The term “nanophthalmos” is used synonymously, but especially when such eyes develop angle-closure glaucoma caused by crowding from the normal-size (ergo, disproportionately large) lens or uveal effusions. Weiss et al. noted that, in general, the posterior segment is proportionately shorter than the anterior segment in such patients.26 Simple microphthalmia/nanophthalmos can be inherited as part of a broader syndrome (Table 3)27,28,29 or as an individual trait. The sclera of nanophthalmic eyes consists of irregularly arranged collagen lamellae, absence of normal elastic fibers, and abnormal glycogen-like deposits.30 These changes likely result in the increased thickness and decreased elasticity of the nanophthalmic sclera—changes that result in decreased blood flow through the vortex veins and/or decreased transscleral flow of protein. This alteration in ocular fluid dynamics increases the risk of uveal effusion and choroidal detachment, especially after surgery.31,32,33
TABLE 3. Syndromes With Simple Microphthalmos/Nanophthalmos as a Phenotype | ||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||
The precise embryologic mechanism for simple microphthalmia/nanophthalmos is unclear. Based on finding this phenotype in patients with fetal alcohol syndrome, achondroplasia, and myotonic dystrophy, Weiss et al. postulated that decreased size of the optic cup, altered vitreous proteoglycans, low intraocular pressure, and abnormal release of growth factors may be important in the pathogenesis of simple microphthalmos.26 These authors point out that given many of these patients have normal corneal diameters and that the area primarily affected is the posterior segment, the pathogenesis in many of these conditions may be related to postnatal, rather than prenatal, changes in ocular development and growth.
In 1998, Othman et al. described a pedigree with autosomal dominant nanophthalmos that localizes to a 14.7cM region on chromosome 11 (NNO1).34 Affected family members had high hyperopia (range of +7.25 to +13 D) and short axial lengths (range of 17.55–19.28 mm). Twelve of 22 affected family members had a history of angle-closure glaucoma or had occludable angles. Although OMIM lists a second nanophthalmos locus, NNO2, on 15q12-q15, the phenotype described in this pedigree is more consistent with a colobomatous, complex microphthalmia (see later).35
Complex Microphthalmia
In cases in which the eye is not only small but also abnormal in other respects, the term “complex microphthalmia” is applied. Examples of associated findings are microcornea, sclerocornea, corneal opacities, aniridia, Peters anomaly and cataract. Complex microphthalmia can be associated with a syndrome (Table 4)19,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61 or can occur as an isolated trait. Complex microphthalmia encompasses a diversity of phenotypes. Patients in the same family with the same underlying disorder may have phenotypes of varying severity. For example, patients with the Lenz microphthalmia syndrome (OMIM 309800) may have anophthalmia, colobomatous microphthalmia, or noncolobomatous microphthalmia.62
TABLE 4. Syndromes with Complex Microphthalmia as a Phenotype | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Numerous chromosomal abnormalities have been associated with microphthalmia (Table 5).63 Warburg and Friedrich provided a comprehensive review of these disorders in 1987.64 Presumably, any chromosomal disorder that significantly affects telencephalon or cranial neural crest development could result in microphthalmia.
TABLE 5. Chromosomal Abnormalities Associated With Microphthalmia | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
Complex microphthalmia is often associated with uveal colobomas. In the most common use of the term, “coloboma” refers to a defect in the iris, retina/uvea, and/or optic nerve as a result of faulty closure of the embryonic fissure at the 7- to 20-mm stage of development. Colobomas tend to be inferonasal, which is the normal position of the embryonic fissure (Fig. 1). The term “coloboma” has also been applied to other anomalies of the optic nerve, the macula, and the uveal tract that are not related to faulty closure of the embryonic fissure. This loose use of terminology creates unnecessary confusion when describing a syndrome. Hornby et al. found in their series that 72 of 185 eyes with coloboma also were microphthalmic and 71 of those 72 had microcornea.65 Thus, not every patient with microphthalmia has coloboma and not every patient with coloboma has microphthalmia. Microphthalmia has been postulated to arise from faulty development of the secondary vitreous and, hence, not enough pressure needed for prenatal eye growth.66
“Microphthalmia with cyst” refers to cases of colobomatous microphthalmia with a posterior eye wall defect through which a cyst lined with neuroectodermally derived tissue protrudes into the orbit. These cysts may be small and only detected by imaging (Fig. 2); sometimes, they may be large enough to cause progressive proptosis. Most cases are isolated, but familial occurrences have been reported.67,68,69 Inheritance is likely autosomal recessive. Depending on the size of the cyst, its appearance, and the visual potential of the microphthalmic eye, these cysts may be managed by observation, excision with or without enucleation, and/or aspiration.70 Aspirated cysts tend to reaccumulate fluid. Socket expansion improves cosmesis.
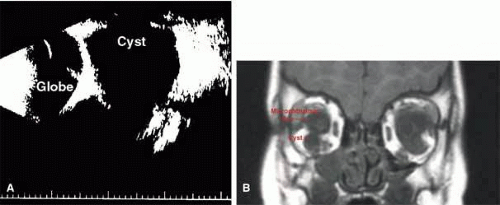 Fig. 2 A. B-scan ultrasonogram shows microphthalmia with cyst. B. MRI demonstrates cyst located on the inferior aspect of a microphthalmic eye. |
Complex microphthalmia can also be seen as part of Peters anomaly and persistent hyperplastic primary vitreous (PHPV). These disorders are covered in the anterior segment and retina/vitreous sections of this chapter.
Not all cases of complex microphthalmia are genetically determined. Intrauterine infection and maternal exposure to alcohol or other teratogens can also cause complex microphthalmia.
Percin et al. described mutations in the homeobox gene CHX10 (14q24.3) in two families with autosomal recessive, nonsyndromic microphthalmia, iris abnormalities, and coloboma.71 Like other homeobox proteins, CHX10 is a transcription factor that binds to specific DNA sequences in the regulatory regions of other genes and affects their transcription during development. Chx10 mutations were previously found in the ocular retardation mouse model, which is characterized by microphthalmia, a thin hypocellular retina, and optic nerve aplasia.72
One form of autosomal recessive complex microphthalmia was found by Bessant et al. to map to 14q32.73 Phenotypic features included sclerocornea (8/8 patients) with secondary corneal vascularization (6/8 patients) and staphyloma formation (3/8 patients), elevated intraocular pressure (5/8 patients), and short axial length (5/5 measured).74 These authors ruled out CHX10 and OTX2 as candidate genes in this pedigree.
Lehman et al. reported a large Mexican American pedigree with isolated X-linked recessive colobomatous microphthalmia that maps to the proximal p or q arm of the X chromosome.75
Microphthalmia can usually be diagnosed by inspection and/or palpation of the eye through the eyelids. The presence of a bulge in the lower lid usually indicates microphthalmos with cyst (Fig. 3). Axial length measurements may aid in the diagnosis of simple microphthalmia/nanophthalmos. Refraction and amblyopia treatment may be helpful in cases in which the macula is well developed. In cases in which no useful vision is present, scleral shells may improved cosmesis. Oculoplastics procedures to enlarge the palpebral fissures and the socket are sometimes helpful.
CONGENITAL CYSTIC EYE
Congenital cystic eye results from failure of the optic vesicle to invaginate, producing a cystic structure that may contain elements of dysplastic retina or lens material.76 These cysts do not contain an epithelial lining, may not be evident at birth, and may grow with time. Approximately 30 cases have been described in the literature. Most cases are unilateral, but bilateral developmental eye anomalies have been described.77,78,79,80 Orbital imaging can aid in the diagnosis and preoperative planning.81
Oculocerebrocutaneous syndrome (Delleman syndrome, OMIM 164180)82 is a sporadic condition associated with orbital cysts, focal dermal hypoplasia, periorbital skin appendages, and cerebral malformations. Anophthalmia may also occur in patients with this syndrome.
PERSISTENT HYPERPLASIA PRIMARY VITREOUS (PHPV) AND PERSISTENCE OF FETAL VASCULATURE (PFV)
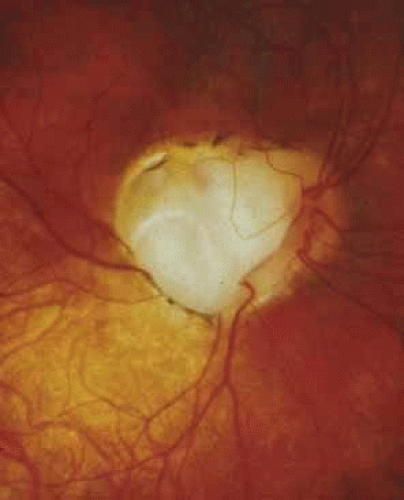
Persistent hyperplastic primary vitreous (PHPV) or persistence of fetal vasculature (PFV) is a complex malformation of the eye characterized by the presence of remnants of the hyaloid and of the tunica vasculosa lentis systems of blood vessels, together with proliferation of fibrovascular tissue behind the lens, and variable degrees of posterior pole and/or anterior retinal dysplasia.83,84 The eye in PHPV is generally microphthalmic but can be enlarged with accompanying myopia.85 Although PHPV primarily affects the posterior part of the eye, the ciliary body, iris, and lens are involved to a variable extent. In the typical case, ciliary processes are elongated and converge to a plaque of retrolental fibrovascular tissue that may involve the lens capsule proper (Fig. 4). The lens may be completely clear or may be cataractous. The fibrovascular plaque may adhere to the posterior lens capsule and vessels can invade the lens—a finding pathognomonic of PHPV. The retrolental membrane may contain adipose tissue, cartilage, and smooth muscle tissue. This is thought to be the result of metaplastic changes in tissues of mesenchymal origin. In a series of 47 eyes, Font et al. found adipose tissue in 10 and cartilage in one.86 The peripheral retina may also be drawn anteriorly into the retrolental membrane. In what has been referred to as “posterior PHPV,” the retina around the disc is pulled up into the posterior vitreous and is thrown into folds that may involve the macular and lead to poor vision. The retina is generally normal in structure, but dysplastic changes have been described. Vitreoretinal traction may lead to retinal breaks and detachment. The fellow eye in PHPV is usually normal but may have a Mittendorf dot or, rarely, one of other abnormalities.
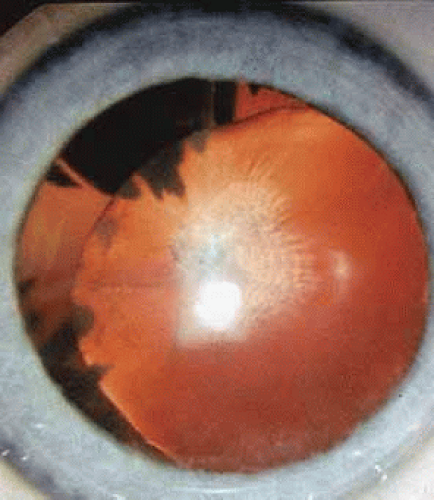 Fig. 4 PHPV. There are numerous elongated ciliary processes drawn to a small lens with an opacified and wrinkled posterior capsule. |
PHPV is unilateral in approximately 90% of cases. The globe varies in size from normal to moderately decreased, being slightly smaller than normal in the majority of cases. The cornea is clear. The anterior chamber is shallow in smaller eyes because of anterior displacement of the iris/lens diaphragm; this predisposes patients with PHPV to angle-closure glaucoma, which usually develops later in life. Lens extraction prevents secondary angle-closure glaucoma. The iris may be normal but frequently shows small notches at the pupillary margin, where iridohyaloidal vessels were located in the developing eye and failed to regress as the iris matures and the tunica vasculosa lentis resorbs. Patent iridohyaloidal vessels may be observed to course over the anterior iris surface, the pupillary margin, and the posterior iris surface to anastomose with vessels in the retrolental membrane. These iridohyaloidal vessels are characteristic of PHPV.
Clinically, patients with PHPV present with a small eye since birth, a white pupillary reflex from a cataract or retrolental membrane, and/or strabismus because of poor vision. Retinoblastoma should be ruled out using clinical examination, ultrasonography, and computed tomography.87 There is no intraocular calcification in PHPV.88 Retinoblastoma generally occurs in normal-size eyes except in patients with 13q deletions and microphthalmia. PHPV and retinoblastoma have been rarely reported together in a microphthalmic eye.89
PHPV and its variants are not very rare. They are a common cause of unilateral congenital cataracts. PHPV has also been reported in patients with recessive oculodento-osseous dysplasia,47 in one patient with protein C deficiency,90 in the oculopalatocerebral syndrome, and in two generations of one family with Rieger anomaly.91
PHPV may be the result of defective formation of the secondary vitreous, which is derived from the inner retinal cells starting in the ninth week of gestation. The secondary vitreous compresses the regressing primary vitreous, which is probably derived from mesenchyme and contains the hyaloid system of blood vessels that anastomose with the tunica vasculosa lentis anteriorly. The globe remains small because its growth depends partly on the expansion of the secondary vitreous.92 The cause of PHPV has not been identified yet. Familial occurrences of PHPV have been reported in dizygotic twins, in two brothers, and in a mother and son.93
Visual prognosis in PHPV is generally guarded. Early cataract surgery may result in relatively good visual results in selected patients.94,95 Eyes with anterior PHPV have a better vision potential than those with posterior pole dysplasia. An anterior approach to lens extraction and retrolental membrane removal is recommended in mild anterior cases. A combined lensectomy-vitrectomy using a pars-plana surgical approach should be considered in patients with significant mid-vitreal or posterior vitreal components to the PHPV. Tractional and rhegmatogenous retinal detachments have been reported in patients with PHPV and are treated surgically as needed.
SYNOPHTHALMIA/CYCLOPIA
Cyclopia refers to a single, midline eye; synophthalmia refers to an apparent midline fusion of two eyes. These conditions are points along a phenotypic continuum. Clinical findings vary but include a proboscis above the eye(s) and forebrain malformations. Many fetuses with cyclopia or synophthalmia have chromosomal abnormalities and are spontaneously aborted.96
Formation of a cyclopic or synophalmic globe may occur by one of two embryologic mechanism.97 At the trilaminar embryo stage, a field of bilobed, midline ectodermal tissue is “fated” to become the eyes. Failure of this bilobed area to separate completely into two fields could result in synophthalmia or cyclopia. Alternatively, previously separated globes could fuse as a result of faulty midline development.
The latter mechanism is likely responsible for the cyclopia and synophthalmia seen in holoprosencephaly. Holoprosencephaly is a genetically and phenotypically heterogeneous group of disorders that manifest with midline abnormalities.98,99 Classically, this includes complete (alobar) or partial (semilobar) “fusion” of the normal, bilateral cerebral hemispheres into a single hemisphere. Mutations in several genes important in forebrain development have been identified in families with holoprosencephaly, including sonic hedgehog (SHH, 7q36), ZIC2 (13q32), SIX3 (2p21), and transforming growth factor beta-induced factor (TGIF, 18p11.3).100,101,102,103
ANIRIDIA
Classic aniridia is a sporadic or autosomal dominant, bilateral, pan-ocular condition caused by haploinsufficiency of the PAX6 homeobox gene on 11p13.104,105 Contrary to the connotation of “aniridia,” most aniridic patients have at least some rudimentary iris tissue. “Aniridia” is also used to describe absence of iris tissue in some syndromes that are possibly unrelated to PAX6 haploinsufficiency (see later).
Aniridia affects multiple tissues in the eye and has a broad range of clinical presentations. Iris abnormalities range from almost complete absence to radial iris clefts to iris hypoplasia (Fig. 5).106,107,108,109 Foveal hypoplasia is characteristic, but of varying severity, which include optic nerve hypoplasia, corneal pannus, and/or a superficial corneal dystrophy (Fig. 6), microcornea, Peters anomaly, congenital cataracts, ectopia lentis, and glaucoma.110,111,112,113,114 Visual potential varies with the severity of the aniridic phenotype. Vision-limiting factors include optic nerve and foveal hypoplasia, cataracts, and—occasionally—the keratopathy that arises in older patients with aniridia. The keratopathy/corneal pannus is presumably caused by insufficient/absent limbal stem cells. Nystagmus develops in aniridic patients, presumably caused by congenital poor visual acuity. Iris vascular anomalies and leakage have been diagnosed on fluorescein angiography of the anterior segment.109
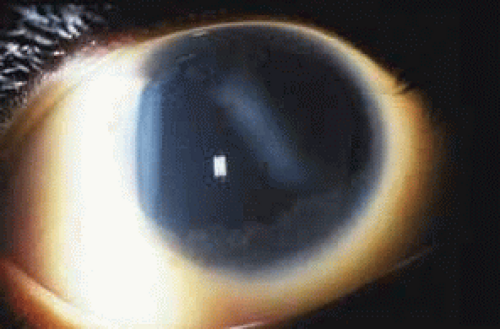 Fig. 6 Keratopathy of aniridia. Note superficial epithelial haze, most prominent in inferior and temporal aspects of the cornea. |
Shaw et al. estimated the prevalence of aniridia in the lower peninsula of Michigan in 1960 to be approximately 1 in 64,000.115 Approximately two-thirds of patients have at least one other affected family member; the remaining one-third are sporadic.
Pathologic studies of aniridic eyes are sometimes complicated by the presence of advanced glaucoma and/or a history of multiple surgical interventions. In 1983, Margo described pathologic features of seven eyes from seven children 6 months to 14 years of age.116 None of these eyes had advanced glaucoma or previous surgery. Congenital anomalies included iris and ciliary body hypoplasia, attenuation of Bowman membrane, and (in two eyes from children with 11p deletions) anomalous anterior chamber angles. Other abnormalities included corneal pannus, cataracts, and peripheral anterior synechiae. Resolution was insufficient to comment on retinal or optic nerve anomalies.
Elsas et al. classified aniridia into four types based on clinical criteria.107 Type I aniridia—what we call classic aniridia—is autosomal-dominant and is characterized by near-absence of iris tissue, foveal hypoplasia, nystagmus, corneal pannus, optic nerve hypoplasia, secondary glaucoma, and (sometimes) dislocation of the lens. Type II aniridia patients have varying iris abnormalities, no nystagmus, and relatively preserved visual acuity. Patients with type III aniridia have classic aniridia and mental retardation. Type IV aniridia patients also have genitourinary anomalies, an increased risk of Wilmss tumor, and mental retardation (WAGR syndrome, discussed later). This system was devised before our detailed knowledge of the cytogenetic and molecular causes of aniridia. Therefore, it does not take into account more recent findings of the phenotypic, cytogenetic, and mutational heterogeneity of this disorder.
Grant and Walton noted progressive angle changes in aniridic patients.117 Although the trabecular meshwork of 25 aniridic patients who did not develop glaucoma appeared normal on gonioscopy, the angles of 31 aniridic patients with glaucoma showed progressive obstruction of the trabecular meshwork by iris tissue. These authors recommended prophylactic goniotomy in aniridic patients who show progressive angle changes before glaucoma develops. This recommendation has not been studied in a controlled fashion.
Cytogenetic studies have played a pivotal role in understanding the molecular basis of aniridia. WAGR syndrome (OMIM 194072)—an acronym for Wilms tumor, aniridia, genitourinary abnormalities, and mental retardation—is associated with deletions of chromosome 11p13 (reviewed by Mannens et al.).118 By comparing the phenotype of patients with the size of the deletion, as determined using both cytogenetic and molecular markers, the critical region for aniridia and for Wilms tumor were identified. Other cytogenetic abnormalities such as paracentric inversions, balanced translocation, and unbalanced translocation involving 11p13 have been reported in subjects with aniridia, both with or without systemic findings.119,120 Not all chromosomal aberrations directly disrupt the PAX6 gene, suggesting that local chromatin structure or cis-acting elements are important for PAX6 expression.121 Crolla and van Heyningen have shown that some patients with deletion of both the Wilms tumor gene (WT1) and PAX6 may not be cytogenetically visible and can only be detected with fluorescent in-situ hybridization (FISH).120
Because the PAX6 gene and the Wilms tumor gene (WT1) are on the same 700-kilobase region of 11p13, chromosomal changes that cause aniridia may also affect the WT1 locus. In general, the increased risk of Wilms tumor occurs in sporadic aniridia cases. The exception to this rule is families in which an affected parent has a deletion of WT1 and passes his/her chromosomal abnormality onto their child. In these cases, autosomal-dominant inheritance is present. Not everyone with a WT1 deletion develops Wilms tumor. Gronskov et al. found two out of five subjects with WT1 deletions that developed Wilms tumor.122 Muto et al. found 13 (45%) of 29 patients with deletions in the Wilms tumor critical region developed Wilms tumor.123 Therefore, cytogenetic studies focused on 11p13 are reasonable in both sporadic aniridia and familial aniridia, when the number of affected individuals in the family is small.
In 1989 Mannens et al. mapped the aniridia locus to markers on 11p13.124 Further analysis of an aniridia pedigree originally mapping to chromosome 2 (AN1 locus)125 showed that the true linkage in this family was also to 11p13 (the AN2 locus.) In 1991, Ton et al. discovered that a homeobox transcription factor gene, now know as PAX6, was either totally or partially deleted in two patients with aniridia.104 Since then, numerous reports of mutations in PAX6 have been reported in patients with aniridia.105 A detailed database of PAX6 mutations can be found online at http://www.pax6.hgu.mrc.ac.uk/.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree