11

Combined Microscopic and
Endoscopic Technique
(COMET Surgery)
Over the past three decades there has been great evolution in nose and paranasal sinus surgery compared with classical approach techniques that have been used. Interest in nasal anatomy dates to practitioners in ancient Egyptian (c. 1500 B.C.) who used the nose as a route for removing the contents of the cranial vault as part of the mummification process to avoid any facial disfiguration.1 From those times until the last century, the progress of medical science, technological developments, and the contribution of excellent physicians throughout the years havemade the techniques performed today possible. By reviewing the medical literature related with the history of paranasal sinus, diagnosis, and treatment, it is possible to conclude that there are five important reasons for the present state of the field of nose and paranasal sinus surgery.
The first reason is the introduction of the binocular Zeiss operating microscope with coaxial illumination for endonasal surgery invented by Hans Heermann (1958).2 At about the same time, Harold Hopkins (1956) applied a new concept of lens systems and proximal illumination to the rigid telescope and used glass fibers for transmission of cold light.3 Nowadays, endoscopes use a light source connected by fiberglass cable that is fitted with a halogen lamp and is available with assorted angles of vision. With its improved illumination and wider field of vision, this newly designed endoscope was immediately used for diagnostic endoscopy. However, the use of telescopes for intranasal surgical procedures is a more recent development because it was necessary to improve the endoscopes and manufacture finer microinstruments that would be suitable for endoscopic sinus surgery.
The second reason is the concept pioneered by Messerklinger (1972),4 who showed that most of the sinus pathology occurs in the anterior ethmoid sinus at the level of the ostiomeatal unit. He used endoscopy in fresh cadaver specimens to demonstrate a disruption of mucociliary clearance in areas obstructed by the contact of two mucosal-covered surfaces in the middle meatus. Stasis of secretions follows this obstruction, which, in turn, leads to infection. According to Messerklinger, such areas of obstruction are most likely to develop in the middle meatus and to involve the anterior and middle ethmoids, with possible involvement of the maxillary, frontal, and posterior ethmoid sinuses and eventually the sphenoid sinus. If these obstructive areas can be removed with an endoscopic approach with restoration of drainage and ventilation through the natural ostia can be established, then resolution of limited or extensive disease in the dependent sinus can be achieved and its mucosa preserved. This represents a revolutionary concept compared with the classical surgical techniques of paranasal sinus surgery, which preferred creation of radical cavities, sometimes with removal of the mucosal coverage, or even intranasal total ethmoidectomy when there was only limited disease. The development of functional endoscopic sinus surgery contributed tremendously by providing a means to remove localized disease obstructing the narrow ethmoid clefts and thereby restoring normal mucociliary drainage and ventilation. Spontaneous resolution of mucosal disease in the maxillary and frontal sinuses could occur without the need for radical mucosal removal. Unfortunately, Messerklinger’s surgical approach for treatment of paranasal sinus disease was not published in the English literature until 1978.5
The fourth reason is the general improvement of medical care, particularly anesthesia, and the administration of antibiotics to prevent local and intracranial complications.
The fifth reason is related to the contribution of many excellent specialists throughout the world practicing rhinology in different locations and teaching these new surgical techniques to the younger generation of doctors. In this regard, the contributions of (in historical order) Prades,6 Dixon,7–9 and Park10 in microsurgery of the paranasal sinus are very valuable. The concept of functional endoscopic sinus surgery was popularized and disseminated throughout the world by Stammberger (1985)11–15 and Kennedy (1985).16–21 Wigand,22–27 Rice,28–33 and Levine34–39 also shared their experience to achieve widespread circulation of this procedure with numerous publications.
Today the concept of functional surgery can be applied to three basic surgical procedures: microscopic sinus surgery, endoscopic sinus surgery, or a combination of both techniques, which has been the author’s preference since 1986.40–42 Other surgeons, including Draf,43–44 Rudert,45 and Stamm,46 are using the same combined technique.
 Surgical Principles
Surgical Principles
General Overview
Contemporary sinus surgery has made tremendous progress over the last three decades. This is the natural consequence of a clear understanding of the pathogenesis of sinus diseases, the improvement of imaging studies, and the development of new optical technologies for better diagnosis and surgical treatment. Also the concept of the ostiomeatal complex, pioneered by Messerklinger,4 has gained wide acceptance. A set of general surgical principles that are applicable to virtually any surgical procedure has been established (Table 11–1).
1. Sinus surgery should be performed after an accurate sinus diagnosis based on clinical history, endoscopic nasal findings, and imaging studies (the basic principle for surgical management of sinus patients). The pathology of the sinus should be clearly established by CT scan prior to any scheduled sinus procedure.
2. Surgical treatment of sinus disease should be performed after failure of appropriate medical management. This should be the general rule of contemporary sinus surgery, and conservative medical treatment should be the first choice for treating sinus problems. Even with massive nasal polyposis a significant decrease of the polyp mass is achieved after systemic administration of steroids. In this situation, preceding medical management will render the surgical procedure easier and less hazardous by decreasing the polyp mass.
3. Proper surgical planning should be the guideline for a comprehensive and accurate surgical plan supported by the clinical history, the nasal findings by endoscopy, and the preoperative CT scan, although it is possible to find unexpected pathology that should be taken care of during surgery.
4. The concept of one-stage integrated treatment of the nose and paranasal sinus is an adequate approach to treat combined nasal problems and sinus diseases during the same surgical procedure (Table 11–2). The importance of correcting local morphological alterations of the nasal cavity, such as septal deviations, septal perforations, concha bullosa, and hypertrophy of the inferior turbinates, during the same operative procedure should be emphasized. These alterations may decrease the nasal airflow and may affect their mucosal drainage and the ventilation of the sinus and, consequently, may cause sinus problems. On the contrary, an infected sinus may drain purulent material to the nasal cavity, adversely affecting the nasal mucosa, which aggravates sinusitis, particularly when there are nasal abnormalities. In this situation, a vicious circle is generated between the affected sinus and the pathologic mucosa of the nasal cavity.
1. Accurate sinus diagnosis 2. Sinus surgery should be performed after failure of appropriate medical management 3. Proper surgical planning 4. One-stage integrated treatment of the nose and paranasal sinus 5. Combined management of sinus disease 6. A thorough knowledge of the nose and paranasal sinus anatomy 7. Excellent visualization and minimal bleeding in the surgical field 8. Removal of diseased tissue from the sinuses 9. Restoration of normal drainage and ventilation in the affected sinuses 10. Adequate postoperative follow-up |
1. Septoplasty and/or rhinoplasty 2. Reduction of hyperthrophic inferior turbinates 3. General surgical principles for endoscopic sinus surgery |
5. Combined management of sinus diseases including pre- and/or postoperative medical treatment should be programmed before any surgical intervention and explained to the patient. The pathogenesis and natural course of chronic hypertrophic inflammatory sinusitis are incompletely understood, and many patients with diffuse nasal polyposis, aspirin sensitivity, and asthma require continued medical therapy such as topical nasal steroids and immunotherapy following surgery to maintain control of their symptoms and to decrease the risk of recurrent disease.
It must be recognized that sinus surgery techniques do not provide a cure for all of the inflammatory sinus diseases because the underlying factors are multiple. Allergies, systemic diseases, genetic influences, and environmental pollution are associated with reactive airway disease. Surgical treatment may correct anatomical abnormalities of the nose and sinus, remove the diseased tissues, restore drainage and ventilation, and possibly control the nature of the disease. However, there are other factors including those mentioned before that should also be taken into consideration and may influence the final outcome of the treatment. Tobacco smoking and exposure to environmental tobacco smoke are also important factors implicated in chronic nasal irritation and other respiratory symptoms in children and adults.47–49 Children exposed to the parental smoking are also at higher risk to develop chronic middle ear effusions and allergic disorders, including allergic rhinitis. It might be expected that after chronic nasal irritation caused by active and passive smoking, such exposure may result in an increased incidence of respiratory disorders of the nose and paranasal sinus, and/or may potentiate the effects of allergies on nasal and sinus functions, and/or may induce the recurrence of sinus disorders after medical/surgical treatment.
6. A thorough knowledge of the nose and paranasal sinus anatomy is of paramount importance. Recognition of the anatomical landmarks that provide surgical guidance is crucial for an effective and safe surgery. The great variability of anatomical structures is a constant feature, and even in the same individual variability occurs from one side to another. Because of these anatomical variations, previous surgical dissections in cadaveric specimens of paranasal sinus should be mandatory before starting surgical treatment of patients with paranasal sinus pathology.
7. Excellent visualization and minimal bleeding are basic surgical requirements for a safe surgery. The use of optical instruments such as the microscope and endoscope allows the surgeon to have an excellent view of the surgical field, including clefts, recesses, niches, and even the inside of the sinus cavities. The contribution of local vasoconstriction to keep bleeding to a minimum is very important.
8. Removal of diseased tissue from the sinus with minimal surgical trauma is another principle of contemporary sinus surgery. One of the priorities of this surgical procedure is the complete and accurate resection of the diseased tissue with maximum preservation of normal-looking mucosa. This concept of functional surgery directed only to a limited removal of irreversibly damaged mucosa and the obstructing anatomy has gained wide acceptance. Even massive inflammatory changes in the sinus mucosa have the capacity to undergo spontaneous healing after restoration of drainage and ventilation. This concept of “reversibility” of mucosal disease has been debated in our specialty for many years, and the merits of aeration versus radical procedures have been discussed. At what point does mucosal disease become irreversible? It is probably better to remove questionable mucosa than to leave it behind and hope that it undergoes transition back to normal tissue, providing that such removal can be safely accomplished.
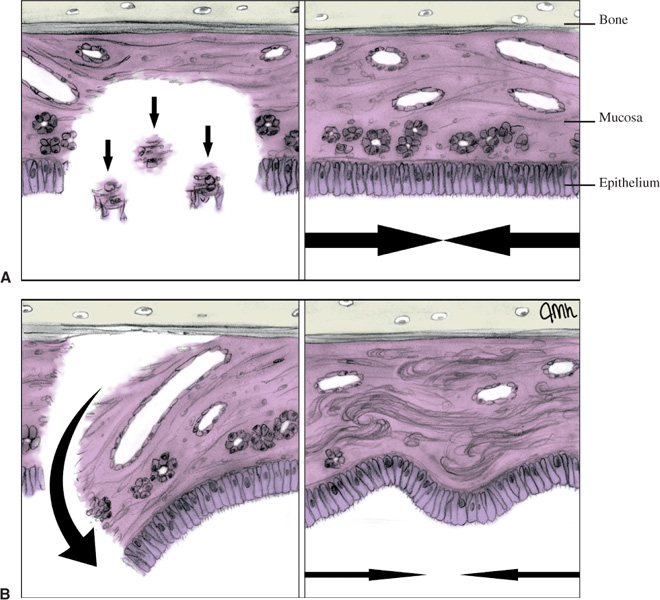
In severe cases of chronic sinusitis, it is important to remove osteitic bony partitions as thoroughly as possible from the areas of severe mucosal disease. It is possible that these sites have a low-grade chronic osteomyelitis that may be responsible for the recurrent focus of chronic sinusitis.50 Although the concept of minimally invasive surgical therapy to remove obstructive areas to improve mucociliary clearance and restore normal sinus drainage and ventilation should be applied particularly in early and mild diseases, a more aggressive surgery should be performed with removal of bony partitions where there is more extensive pathology, while at the same time preserving the normal-looking mucosa. However, complete removal of mucosa from the bony surfaces should be avoided because this will increase the possibility of postoperative osteitis and scar formation (Fig. 11–1A and B).
9. Restoration of normal drainage and ventilation from the affected sinus is the concept introduced by Messerklinger.5 In the past it was believed that chronic inflammatory disorder of the paranasal sinuses was an infectious process arising primarily from the affected sinus itself. However, based on studies of mucociliary clearance, Messerklinger was able to demonstrate that the etiology in most patients with chronic or recurrent sinusitis in the ethmoid, maxillary, and frontal sinuses is related to anatomical abnormalities and/or mucosal pathology obstructing the drainage system of these sinuses. Classical surgical procedures for treatment of chronic infections of the sinuses and other disorders, such as nasal polyposis, direct the surgeon to remove diseased tissues in the nose and/or paranasal sinuses. The new surgical openings in the sinus caused by those conventional surgical techniques are in locations distant from the natural ostium, and so treatment of the disease interferes with the mechanism of drainage of secretions of the sinus already disturbed by the infection.
FIGURE 11–1 Surgical dissection of the sinus mucosa should be very gentle, leaving normal-looking mucosa behind and avoiding exposure of the bony surface as much as possible. (A) The reepithelization with ciliated epithelium is more rapid, with less scarring effect and with a more uniform aspect. (B) Same dissection with denuded bone, more scarring and a less uniform appearance result.
The mucus produced in the anterior ethmoid sinus, maxillary sinus, and frontal sinus drains into an anatomically complex region of the lateral nasal wall called the ostiomeatal complex. The ostiomeatal complex is a narrow anatomical region consisting of multiple bony structures (middle turbinate, uncinate process, ethmoid bulla), air spaces (frontal recess, ethmoid infundibulum, middle meatus), and the ostia of the anterior ethmoid, maxillary, and frontal sinuses. In this area the mucosal surfaces are very close or even in contact with each other, and mucous secretions can be removed easily from the sinus because of the ciliary sweeping motion, which keeps the drainage system functioning. If, however, the opposing mucosal surfaces in this cleft become inflamed and swollen, drainage and ventilation of the sinus may be seriously impaired because the ciliary sweeping motion decreases and eventually ceases. When edema develops, the ostium quickly becomes blocked because of its small diameter, and consequently mucus can no longer be excreted. Also, ventilation that ensures gaseous exchange can be affected, and any alteration of this mechanism can have deleterious consequences. Hypoxia, increasing edema, decreased ciliary motion, and transudate form a vicious circle that facilitates possible infection. Supuration then develops either as a result of aerobic bacterial infection that consumes large amounts of oxygen or by a gradual decrease in pO2 pressure that makes phagocytosis less effective and permits colonization by anaerobic organisms.
The concept that restoration of the drainage and ventilation systems through the natural ostia using endoscopic sinus surgery can reestablish normal function of the sinus and treat pathological changes in the dependent sinus has radically revolutionized the surgical treatment of sinus diseases.
10. Adequate postoperative follow-up after sinus surgery is mandatory at regular intervals until healing is complete. Endoscopic examination of the nose is advised to clean the crusts, clotted blood, and thick mucus from the nose, ostiomeatal complex area, and accessible regions of the sinus cavities. Synechiae must be removed at an early stage, and lateralization of the middle turbinate should be avoided.
All patients who have undergone endonasal sinus surgery will benefit postoperatively from a prolonged course of nasal irrigations using a saline nasal spray and an aerosol nasal corticosteroid for a shorter period of time following initial healing and diminution of crusting. Patients with allergic rhinitis should be maintained on topical corticosteroids and appropriate pharmacotherapy and immunotherapy.
Surgical Indications
The current indications for surgical treatment of paranasal sinus disease are defined by our knowledge of its pathogenesis, its natural evolution, and how that course can be changed by different treatment modalities. Certainly surgery is one option, and the ultimate goal is to eradicate the disease. However, we should keep in mind that we cannot cure all patients even with the most up-to-date equipment and the best surgical techniques available and properly executed.
The main and most frequent indications for paranasal sinus surgery are summarized in Table 11–3, but their range will continue to increase and expand with new sophisticated equipment and more refined surgical procedures. The surgeon must tailor the operation to the disease and its characteristics, location, and extent. However, the patient’s clinical condition, ability to withstand general anesthesia, prolonged postoperative care, and expectations must be considered.
– Inflammatory diseases • Chronic sinusitis • Complicated acute sinusitis • Recurrent acute sinusitis • Hyperplastic sinusitis (sinonasal polyposis) • Sinus mucoceles • Allergic fungal sinusitis – Neurorhinologic disorders • Rhinopathic headaches resistant to medical therapy – Orbital indications • Severe exophthalmos • Nasolacrimal duct obstruction – Restorative indications • Cerebrospinal fluid rhinorrhea • Severe posterior epistaxis • Choanal atresia/stenosis – Neoplastic diseases • Benign tumors (osteoma, hemangiopercytioma, juvenile angiofibroma, and pituitary tumors) • Malignant tumors (biopsy for diagnosis and assistance in craniofacial resection) |
The most common indication for performing paranasal sinus surgery is chronic sinusitis. However, if adequate medical therapy can control the patient’s symptoms and the evolution of the disease, then the benefit of surgery is difficult to justify, and it should be avoided. Most patients with acute sinusitis can be treated with appropriate medical management without the need for surgical intervention. In certain cases with threatening or established complications (e.g., abscess formation), surgery should be performed to achieve drainage of the involved sinuses. In cases of acute sinusitis with periorbital or intraorbital complications, sinus surgery can provide access to the medial orbital wall (lamina papyracea), and resecting the lamina will expose the periorbital fascia to drain the periorbital abscess or to incise the fascia to decompress orbital cellulitis.
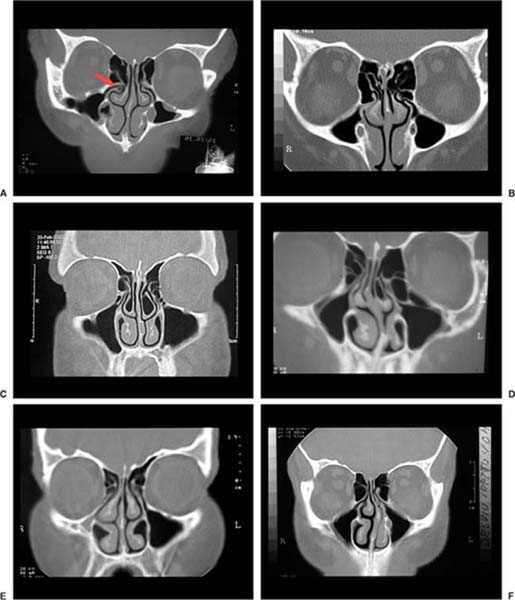
Recurrent acute sinusitis is an uncommon indication, and the patient should be evaluated very carefully before the decision to undergo surgery is made. This condition is defined by the absence of significant mucosal disease during the intervals of acute sinusitis episodes. A variety of anatomical abnormalities may be visualized on CT scan in this type of sinusitis, including the concha bullosa and the paradoxical middle turbinate (Fig. 11–2).
Variations of the uncinate process (with either pneumatization or lateralization), excessive aeration of anterior ethmoid cells, enlarged Haller’s cells, and agger nasi cells may also be found. These alterations may decrease sinus drainage and ventilation and predispose the patient to recurrent acute sinusitis. An excessively deviated nasal septum may have the same effect by impinging upon the middle turbinate and narrowing the infundibulum. In these cases, medical management may help control the frequency and severity of the infections, but only surgery can solve the problem. Usually the maxillary sinus is the affected sinus, and a very limited approach to enlarge the natural ostium is the treatment of choice. The other abnormalities should be surgically treated also using techniques like septoplasty, resection of the lateral lamella of the concha bullosa and partial resection of the middle turbinate to remove the lateralized segment.
FIGURE 11–2 Coronal CT scans of patients with anatomical abnormalities of the nose and paranasal sinus. (A) Pneumatized right uncinate process. (B) Hypertrophy of the ethmoid bulla obstructing, the right ostiomeatal complex. (C). Bilateral concha bullosa. (D) Deviated nasal septum toward the right side. On the left side a concha bullosa and Haller’s cells are obstructing the ostiomeatal complex. (E). Hypoplasia of the right maxillary sinus. (F) Deviated nasal septum pushing the middle turbinate laterally, causing obstruction of the left ostiomeatal complex. (Images courtesy of J. Almeida Pinto.)
Another indication for sinus surgery is the endoscopic drainage of the sinus mucoceles. The frontal sinus is most commonly involved, followed, in order of frequency, by the ethmoid, sphenoid, and maxillary sinuses.
Allergic fungal sinusitis is an absolute indication for endonasal sinus surgery, and surgery should be considered in patients who do not respond to conventional medical therapy. The goal of this surgical treatment is the complete removal of diseased mucosa, bony partitions, and inspissated material containing fungus that should be sent for staining and culture tests for positive identification. Postoperatively, all patients require adjunctive medical treatment with antibiotics, topical and oral steroids, and oral antifungal agents.
Endoscopic surgery for management of rhinopathic headaches refractory to medical therapy is one of the most controversial indications of sinus surgery. It is possible that, in the absence of sinus inflammation, structural abnormalities may create an intermittent obstruction of the sinus that may induce chronic facial pain syndrome. This phenomenon can be compared with others related to the ear and eustachian tube dysfunction. The sinus CT scan may only reveal bony anatomical variations or abnormalities. In the author’s experience, this condition may be misdiagnosed despite a very careful evaluation and screening. During surgical treatment of a limited number of cases, a lateralized uncinate process, a small concha bullosa, or a paradoxical middle turbinate was found. In all cases the mucosa of the infundibulum was edematous, and the maxillary sinus ostium was closed. The procedure itself consisted only of removal of the anatomical abnormalities and the enlargement of the maxillary sinus ostium. In all patients the symptoms disappeared. Definitive proof of this association, though, depends on resolution of the syndrome after surgical correction. However, in patients complaining of headaches with limited sinus symptomatology, negative neurological work-up, and prolonged medical therapy with nasal steroid spray and decongestant, surgery should be considered the treatment of last resort when other methods have not controlled the complaints.
Endoscopic orbital decompression may be used for surgical treatment of severe exophthalmos (thyroid orbitopathy or Graves’ disease), and the results are similar to the conventional techniques with the added advantages of an endoscopic approach.
Nasolacrimal duct obstruction and chronic dacryocystitis requiring surgical intervention can also be managed endoscopically with significant advantages over external intervention.
Cerebrospinal fluid rhinorrhea can be treated with an endoscopic nasal approach with higher success rates using mucosal grafts and, for lesions greater than 5 mm, free bone or cartilage grafts along with a local pedicled mucosal flap. Certainly craniotomy may be required for larger defects, but the endoscopic management of skull base defects avoids the significant morbidity associated with a craniotomy.
Even posterior epistaxis can be treated endoscopically through cauterization or clipping of the sphenopalatine artery. Choanal atresia/stenosis may be managed by removing the stenotic area using this technique.
The role of endoscopic sinus surgery in neoplastic diseases is primarily to treat selected cases of benign tumors, such as osteomas, hemangiopericytomas, juvenile angiofibromas, and pituitary tumors. Vascular lesions should have preoperative embolization to decrease intraoperative bleeding to a minimum. In the author’s experience this is an excellent approach, with decreased morbidity and a better postoperative period.
The contribution of endoscopic techniques in relation to malignant tumors is to assist in craniofacial resection. During the tumor resection an endonasal approach provides excellent illumination of the roof of the nasal cavity and guides anterior fossa osteotomies from the cranial side under microscopic visualization of the vertical cuts on both the medial orbital walls after the brain has been retracted posteriorly. The extensive skull base defect following the resection of both ethmoid bones (en bloc resection of anterior cranial floor) is then closed with a bone graft from the internal table of the cranium. Additional resection of adjacent structures can be performed depending on the extent of disease. This is the perfect example of the benefit of combined microscopic and endoscopic sinus surgery (COMET surgery).
Other indications for paranasal sinus surgery and special procedures will be covered in other chapters of this book.
Absolute | Relative |
• Clinical history • Complete ORL examination • Nasal endoscopy • Computed tomography (coronal and axial scans) | • Rhinomanometry and acoustic rhinometry • Allergy testing • Olfactometry • Mucociliary testing • Nasal citology • Sweat test (children) • Immunoglobulin studies • Nasal mucosal biopsy |
Preoperative Evaluation
The outcome of paranasal sinus surgery depends on a very careful preoperative evaluation, including a complete otorhinolaryngologic examination with special emphasis on the nose and paranasal sinuses, and a collection of general medical information about the clinical condition of the patient. The routine examination comprehends a clinical history, physical examination, and complementary testing considered necessary for an accurate diagnosis (Table 11–4).
The clinical history related with the nose and paranasal sinuses is directed to the most common symptoms: nasal obstruction, nasal stuffiness, anterior nasal discharge, postnasal drip, mucopurulent rhinorrhea, itchy nose, sneezing, disorders of smell, facial pain, pressure, and headaches. Questioning should be systematic and should also cover the symptoms of ear diseases (e.g., hearing loss, popping and itching in the ears, and sensations of pressure). Chronic throat symptoms, such as slight discomfort, pain, dry sensation, scratchy throat, and frequent throat clearing, are often due to discharge from an infected nasal region and/or chronic sinusitis flowing down the pharynx. Also, pulmonary symptoms (coughing, spitting, wheezing, etc.), diseases of the teeth and jaws, allergic symptoms, eye complaints (eye pressure, pain, watery eyes, etc.), dizziness, chronic fatigue, weight loss, inflammatory diseases of the joints, autonomic disorders, and skin and systemic diseases, such as diabetes and hypertension, should be inquired about. The clinical history should establish the timing of the symptoms, duration of the disease (acute, chronic, or recurrent), tobacco smoking, current medications, previous surgeries, and complications.
The nasal examination should be performed in a routine fashion looking for morphologic abnormalities and characteristics of the nasal mucosa and its secretions. Particular attention should be paid to the lateral nasal wall and the middle turbinate area, although often this cannot be accomplished until a nasal spray decongestant is applied. This nasal inspection can also be accomplished using the microscope as the light source instead of a headlight (Fig. 11–3). The author has used the microscope for routine otorhinolaryngologic examination for the past 20 years because it provides better illumination and amplification.
If the nasal abnormalities are detected by anterior or posterior microrhinoscopy, no further examination is necessary. However, if the nasal examination under the microscope needs further evaluation or is otherwise incomplete, it should be combined with nasal endoscopy. This diagnostic technique is best performed by spraying the nose with a vasoconstrictor (0.5% phenilephrine hydrochloride) and an anesthetic agent (10% lidocaine) and allowing them to work for a few minutes. Then the entire nasal cavity should be systematically examined (including the nasopharynx) with a rigid 0-degree, 4 mm endoscope, or, if it is difficult to pass between the middle turbinate and the lateral nasal wall, a 30-degree, 2.7 mm endoscope. The flexible 3.2 mm endoscope is preferable with children. Again, particular attention should be paid to the middle meatus, where it is likely that the main changes will be found. Using videoendoscopy, these findings can be stored on a digital videotape, and with a laser printer the resulting images can be printed for the patient’s chart.
FIGURE 11–3 Routine otorhinolaryngologic examination using the microscope.
The rhinologist must develop a special expertise in this imaging technique that will allow him or her to read the images, follow them carefully in the operating room, and compare them with the intraoperative findings. The clinical examination is mandatory, but the correlation with the imaging studies is absolutely necessary to make an accurate diagnosis and to manage the patient correctly according to his or her problem.
Other tests, such as the rhinomanometry and acoustic rhinometry,51–60 are performed on patients complaining of nasal obstruction in the routine preoperative evaluation. The rhinomanometry is an objective nasal test that measures nasal airway resistance by making a quantitative measurement of nasal flow and pressure. Acoustic rhinometry is another nasal test based on sound reflection that provides an estimate of the cross-sectional area as a function of distance from the nostril. Both are indicated mainly for quantification of pre- and posttherapy (medical and/or surgical) for nasal obstruction, for exclusion of functional disorders, and for medicolegal purposes. Nasal respiration and paranasal sinus aeration are not always correlated. However, improvement of the nasal air passages will contribute to the recovery of the sinus from sinusitis. In this situation, surgical treatment of the deviated nasal septum and/or the hyperthrophic inferior turbinates together with paranasal sinus surgery is essential to correct the nose and paranasal sinus unit. All of these procedures can be performed during the same operation, which the author calls one-stage integrated surgical treatment.
If there are systemic allergic disorders such as asthma, dermatitis, conjunctivitis, or gastrointestinal disturbances, or an underlying allergy coupled with nasal symptoms, then allergy testing is requested. The skin prick test, IgE antibodies (RAST) test, and serum IgE (PRIST) test are very useful for identification of the allergens responsible for the symptoms.61–66
Preoperative olfactometry is very valuable for assessing disturbances of the olfaction and the results of ethmoid procedures in diffuse polyposis. Dysosmia is often caused by inflammation of the olfactory mucosa, and it improves after careful endoscopic management of the polypoid mucosa of the olfactory cleft. Other tests, such as mucociliary testing and nasal cytology, may be useful for additional information, but they should not be considered routine tests for preoperative evaluation.67–74
In children with chronic recurrent sinusitis, the sweat test should be used to rule out cystic fibrosis, and determination of immunoglobulins and immunoglobulin classes, along with nasal mucosa biopsy to establish the diagnosis of ciliary diskinesia.75–78
After reviewing these tests for preoperative evaluation, it should be concluded that clinical examination of the patient together with the imaging studies is essential for an accurate diagnosis. Other tests should be performed according to the clinical judgment. Correct diagnosis and the establishment of a surgical plan can be achieved in most situations by combining clinical examination, endoscopic results, and imaging studies.
The author strongly advises having a protocol for sinus surgery to evaluate sinus symptoms and to describe the nasal endoscopic and CT scan findings, surgical planning, and the results of surgery. It is a great effort toward data standardization that can be stored in a computer for a better update and follow-up, analysis of long-term results, and interchange of medical information.
Surgical Planning
After a careful preoperative evaluation, an accurate diagnosis can be established, and a treatment plan must be developed and introduced to the patient. The surgical procedure should be defined by the clinical examination, and the objective findings encountered during the preoperative evaluation must follow the surgical principles already described and must be performed according to the surgeon’s experience. The age of the patient and his or her medical conditions, expectations should also be considered before a final decision is made and the patient is scheduled for surgery.
Preoperative medication should be recommended before surgery in patients who have suppurative sinusitis. They should receive an appropriate oral antibiotic for 10 to 12 days before the surgical procedure. Patients with massive polyposis should take a short treatment of oral corticosteroids immediately before surgical treatment with a “booster” dose intraoperatively. Hypertension and diabetes must be controlled before surgical intervention with the cooperation of an internist. Medications, such as aspirin and nonsteroidal anti-inflammatory drugs that prolong bleeding should be discontinued before the operation.
The different phases of the treatment plan, including preoperative remarks, type and extent of surgery, and the postoperative follow-up, should be discussed with the patient. The final outcome of the treatment, including possible risks and complications of surgery, should also be stressed. Certainly the surgeon’s experience and his or her trust in the results are very important factors in convincing the patient to accept the proposed treatment plan and sign the informed consent.
 Instrumentation
Instrumentation
Surgical Equipment
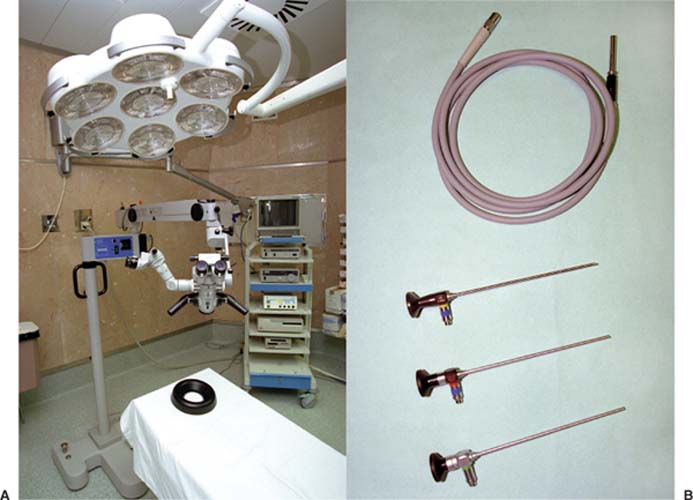
Two optical systems are used to surgically treat the nose and paranasal sinuses: the microscope and the endoscope. The combination of both systems during the same surgical procedure is called combined microscopic and endoscopic technique (COMET surgery).
The majority of the surgical operation is performed with the Zeiss operating microscope OPMI ORL (Fig. 11–4) equipped with coaxial fiberoptic, cold-light illumination with a 12 V, 100 W halogen reflector lamp (cold light), spot illumination, 0-degree central illumination, 1:6 zoom magnification, 180-degree wide field tiltable tubes with eyepieces, and motorized internal fine focusing. A stereo co-observation tube with excellent ergonomic conditions is used for the assistant, and another arm with a video camera system is adapted to the microscope and fitted with a lens with a focal length of 300 mm.
FIGURE 11–4 The two optical systems used in COMET surgery. (A) Zeiss operating microscope OPM1 with 300 mm lens. Next to the microscope is the Karl Storz Mobile Video-cart (Karl Storz, Tuttlingen, Germany) containing the video endoscopic system (color monitor, cold-light fountain, endocamera, video recorder, and video printer). (B) Standard 4 mm Hopkins rod telescopes with 0-, 30-, and 70-degree angled lenses.
The viewing angles of telescopes range from 0 to 120 degrees. They are all available in standard or wide angles. The standard diameter is 4 mm for surgical procedures in adults. The smaller diameter 30-degree, 2.7 mm telescopes are used to view through the trocar sleeve and are also used for pediatric patients. The 0- and 30-degree, 4 mm diameter telescopes are the most useful. The 70-degree telescope is often required to visualize hidden pathology or deep lateral wall structures inside the sinuses. The telescopes have a length of 18 cm, and they have a connection for a fiberoptic light cable. The relationship between the diameter and the length of an endoscope requires a complex optical rod system. The intermediate image produced by the lens is transposed through a series of rod-lens inversion systems over the length of the endoscope sheath. The term inversion system means that each one of these systems inverts the image. The image is always returned to its correct position if there is an even number of rod lenses in the system. The intermediate image from the last (proximal) inversion system is displayed and enlarged through the eyepiece of the telescope. Cold-light illumination, provided by a powerful xenon light source and conducted by film optic light cables, is always used.
Video recording of the images obtained with a small change-coupled device (CCD-type) video camera attached to both the microscope and the telescope is extremely important for surgical demonstration of endonasal surgery and, therefore, for teaching purposes and for medical documentation. The high light sensitivity of modern video systems permits their use with moderate-intensity light sources. For video recording, the most widely used and best for compatibility are VHS and SVHS 8 mm formats. The 8 mm formats have the convenience of small tape size, which facilitates storage. For most purposes, the SVHS is a good compromise between convenient size and image quality. The recording techniques of still photography and video imaging permit retention of images for later retrieval and also offer the ability to compare images before and after treatment. Recently, with the introduction of a digital still recorder with superior image quality, images can be obtained as still pictures of video recording. Because of their superior quality, these images are recommended for publication and teaching.
In a teaching hospital, an endoscopic camera is a necessity and can be linked to an endoscope or to the sidearm on the operating microscope, permitting all the staff or those outside the operating room to follow the surgery. Although cameras are available using couplings with or without beam splitters (which provide the surgeon with visualization through the endoscope), the former is recommended.
A wide range of microsurgical instruments is available for endoscopic nasal surgery, including sickle knives, rasps, probes, elevators, suction tubes, curettes, and microscissors. The basic set also contains punches and forceps. The backbitting forceps have a through-cutting mechanism that prevents tearing and stripping of the mucosa and leaves a smoother cut than the standard grasping/biting jaws. The cutting punches allow removal of tissue with preservation of neighboring viable mucosa. These instruments have been modified since the beginning of endoscopic sinus surgery to have a more narrow profile and a longer jaw. Other modifications include downbiting forceps, sidebiting forceps, and a forceps with a rotating head that allows any orientation of the jaws. The set also contains giraffe forceps with a long, thin shaft capable of changing angles (hence the name giraffe forceps). The standard set should also have a drill with an angulated hand piece and extra-long diamond burs (used in sphenoid sinus and transnasal surgery of the hypohysis). Other instruments, such as forceps with offset handles for intranasal bipolar coagulation and semi-rigid coagulation probes, complete the set of surgical equipment to perform sinus surgery.
 Optical Principles
Optical Principles
Microscopes have been well-established magnifying equipment in practical use in otorhinolaryngology, and their sophistication has reached powerful limits with the current technologies. In 1923, Holmgren introduced the binocular operative microscope without coaxial light for ear surgery.79
Endonasal surgery and laryngeal microsurgery accompany the historical developments of ear surgery. In 1958, Heermann pioneered the use of the binocular Zeiss operating microscope with coaxial illumination in endonasal surgery.2 Kleinsasser was the founder of modern laryngeal microsurgery in 1962, using a Zeiss operating microscope.80
Since the beginning, the application of the operating microscope has been the standard method of optical aid in otorhinolaryngology. In 1972, Messerklinger developed the concept of endoscopic sinus surgery using nasal endoscopes. This has revolutionized, improved, and radically changed the techniques used for the diagnosis and treatment of patients with sinus disease.
– Focal distance (working distance) – Depth of field (focus) – Numerical aperture – Field of view – Resolution limit – Luminance (brightness) – Distortion – Cleanliness and protection |
Other surgeons, including this author, are continuing to use both instruments, combining microscopic and endoscopic techniques (COMET surgery).
Optical Performances
The two basic optical instruments used for sinus surgery are the microscope and the endoscope. It is absolutely necessary for technical knowledge and teaching purposes to describe the main parameters of any optical system81 and to compare the characteristics of these optical aids based on optical performance and ergonomic capabilities. Although there are several relationships between the main characteristic parameters of any optical system, for practical reasons, the most important and currently used ones are described here (Tables 11–5 and 11–6).
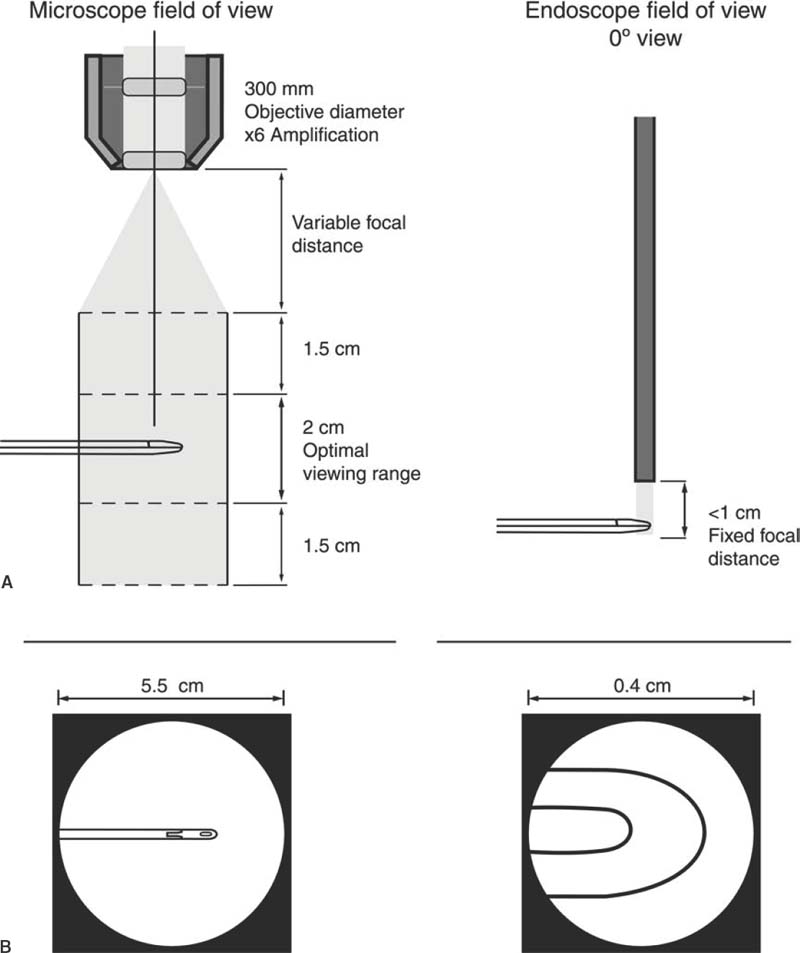
The focal distance (working distance) defines the clearance or distance between the object and the first surface of a lens system. It affects the user’s ability to image and manipulate the sample at the same time. The working distance increases with the objective focal length. For the microscope, the focal distance is variable and finely adjustable. The range is in the order of 300 mm, giving very ample volume for all surgical work. The head of the surgeon, once working on a region, remains steady behind the ocular, and the adjustment of the focus is simple by rotating the focusing knob.
For the endoscope, the focal distance is fixed, not adjustable. The range is in the order of a few millimeters. The working volume is very small. The head and one of the hands of the surgeon have to move to focus. The surgeon has to bow his or her head over the patient and remain at a close distance to see through the endoscope.
The depth of field (focus) is the distance by which the image (or object) may be shifted longitudinally with respect to a reference plane (retina of optical system) without introducing unacceptable blur. In practice, this represents the visible depth of the object.
The microscope presents a much larger depth of field, providing a deeper volume of visibility. Also, the depth of focus is much greater, and the surgeon can comfortably move his or her eyes behind the ocular lens. With the endoscope, the depth of field is shorter; therefore, the endoscope must be finely moved by hand to examine in depth. The depth of focus is short, and consequently the eyes of the surgeon have to move together with the endoscope to keep the image in focus.
The numerical aperture is related to the depth of field (focus), the luminance, and the resolution of the system. The illumination of an image is proportional to the square of the numerical aperture. The numerical aperture in the microscope is smaller, more light is required (illuminating a larger area), and resolution limit is smaller than in the endoscope. However, it can be varied and adjusted. In the endoscope, the numerical aperture is higher and the image looks brighter and has better fine details, although the image field extension is much smaller. The numerical aperture is fixed, and the endoscope must be moved.
Optical characteristics | Microscope | Endoscope |
Focal distance | • Variable and finely adjustable • Larger working volume | Fixed, not adjustable Small working volume |
Depth of field (Focus) | Larger, with a deeper volume of visibility | Shorter; the surgeon’s eyes move in sync with the endoscope |
Numerical aperture | More light is required; when illuminating a larger area, resolution is smaller | Image looks brighter, better fine details, although field extension is much smaller |
Field of view | More extended (as is the volume); surgeon observes the full movement of the total body of surgical | Smaller; surgeon sees only the tip of the surgical instruments and cannot follow the movement |
except | Instruments | within a short range |
Resolution limit | Smaller but very adequate; can be varied and adjusted | Higher, giving finer details; resolution is fixed, and the endoscope must be changed whenever resolution has to be adjusted |
Luminance (brightness of image) | Smaller, can be adjusted by using a stronger light source; uniform without bright spots | Higher, with strong reflections; bright spots occur with frequency, which may cause temporary discomfort to the surgeon |
Distortion | Smaller | Higher |
Cleanliness and protection | The entire optical system is away from the surgical field, so the system is clean and protected | Part of the optical system is placed within the working surgical volume and constantly affected by fogging, staining, and accidental scratching |
The field of view is the volume within which there is image formation. In the microscope, the field of view is much more extended, as is the volume. The surgeon is able to follow the movement of almost the entire body of the surgical instruments. With the endoscope, the field of view is much smaller. The surgeon can see only the tip of the surgical tools and therefore follow the movement only within a short range (Fig. 11–5).
FIGURE 11–5 Comparison of the optical performances of the microscope versus the endoscope. (A) Field of view of the microscope. (B) Field of view of the endoscope.
With the endoscope, the resolution, in principle, is higher, giving finer details in a clear form. However, the resolution is fixed, and the endoscope must be changed whenever the numerical aperture and the resolution have to be adjusted.
The luminance (brightness of the image) is the quantity of light flux passing through a point on a specific surface, in a specified direction per unit of projected area, and per unit solid angle in the given direction. For the microscope, the luminance is smaller, but it can be adjusted, either by using a stronger light source or by increasing the numerical aperture. In practice, it does not represent a disadvantage. The luminance is uniform without bright spots. The endoscope intrinsically presents a higher luminance. However, due to the mechanism, if illumination is by fiber optics and the image forming process is fiber optics, the used light source has to be more intense. In practice, the problem is solved, and the luminance of the image is good. Nevertheless, as the tip of the endoscope acts as a light source very close to the surgical instruments with highly reflective surfaces, strong reflections occur during the procedure that saturate the image, and bright spots occur with frequency. This may cause temporary discomfort to the surgeon, but slight adjustments of light intensity during surgery can be performed.
The distortion is related to technical performance of the optical system, which has imperfections and does not handle perfect spherical waves. Distortion is one of the so-called primary aberrations Efforts are being made to design an optical system that minimizes aberrations and optimizes its performance for this application.
The design of the optical microscope leads to smaller distortion. In the endoscope, the number of optical elements for aberration correction generally causes a higher distortion.
Cleanliness and protection are relevant for preservation and operation purposes. Because the microscope has all optical systems far away from the surgical field, it presents as an ideal solution. The endoscope is placed within the area to be treated, and so is constantly affected by fogging, staining, and accidental scratching.
Optical characteristics | Microscope | Endoscope |
Objective focal length | 0.5–100 mm | 0.2–5 mm |
Magnification | 5X–5000X | 2X–26X |
Numerical aperture | 0.10–0.96 | 0.25–0.7 |
Resolution power | <430 I p/mm | 250–400 I p/mm |
Depth of field | Few μm | Mm to ∞ |