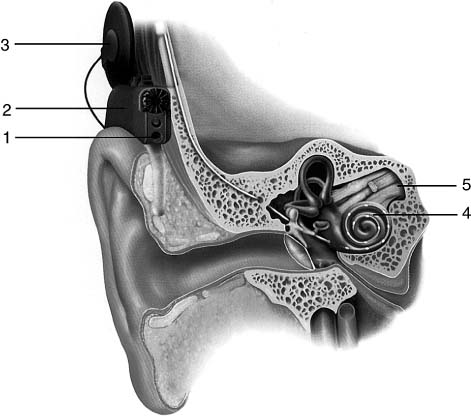
13 Cochlear Implants Cochlear implants can be considered as the first devices that became available for rehabilitation of a sensory function loss. These devices have allowed deaf individuals to reintegrate with the hearing world. Unlike hearing aids, which merely amplify sounds, cochlear implants convert received sounds into a series of electrical impulses, which are delivered to the auditory nerve by placement of an electrode array within the scala tympani of the cochlea. An internal receiver-stimulator contains circuitry designed to convert the coded information received from the externally worn speech processor to electrical impulses and governs the activation of specific electrodes. The newest designs for the externally worn components of these devices combine a microphone and the speech processor technology into one unit that is comfortably worn at the ear level. A small connector cable links the ear level unit to a transmitter coil that interfaces with the internal receiver-stimulator and is held in place by a small magnet (Fig. 13–1). The current technologic sophistication of today’s cochlear implant systems can restore hearing in adults to a functional level and provide young children with auditory stimulation that benefits them in developing, comprehending, and producing spoken communication as well as recognizing and understanding sounds in their environment. These advantages have important implications, especially for young children relative to their communication acquisition, cognitive development, education, social well-being, family relationships, activities of daily living, and future vocational options. Hearing loss is the third most self-reported health problem of individuals 65 years of age or older, listed after arthritis and hypertension.1 It has been reported that there are at least 464,000 and perhaps as many as 738,000 severe to profoundly hard-of-hearing individuals among the 28 million hearing-impaired Americans; 54% of this population is over age 65 years.2 Most of these individuals could benefit from cochlear implantation. Severe to profound hearing loss prior to the development of language (prelingual) occurs in 0.5 to 3 per 1000 live births.3 The prevalence of hearing impairment among children between the ages of 3 and 10 years has been reported to be 1.1 cases per 1000 children.4 Factors that increase the risk for hearing loss in children include a family history of hearing impairment, ototoxic drug exposure, congenital or central nervous system infections, congenital head and neck deformities, birth trauma, minority ethnicity, lower socioeconomic status, and prematurity.5 Hearing-impaired individuals are more likely to be publicly insured, less likely to have private insurance, have lower family incomes, are less educated, and are more likely to be unemployed than the general population.2 Approximately 42% of people with severe to profound hearing loss between the ages 18 and 44 years are not working, compared with 18% of the general population.6 Severe to profound hearing loss has been estimated to cost society $297,000 over the lifetime of an individual. Most of these losses (67%) are due to reduced work productivity, although the use of special education resources among children contributes an additional 21%. Lifetime costs for those with prelingual onset of hearing loss exceed $1 million.6 The educational cost of a severe to profoundly hard-of-hearing child from kindergarten through grade 12 is close to half a million dollars per child, which is five times the cost of educating a normal-hearing child.7,8 Figure 13–1 How a cochlear implant works. Sounds are picked up by the microphone (1). The signal is then “coded” (turned into a special pattern of electrical pulses) (2). These pulses are sent to the coil and are then transmitted across the skin to the implant (3). The implant sends a pattern of electrical pulses to the electrodes in the cochlea (4). The auditory nerve picks up these electrical pulses and sends them to the brain (5). The brain recognizes these signals as sound. (Courtesy of MED-EL Corp., Durham, NC.) Depression and sleep disturbance are more frequent among elderly prelingually deaf people using sign language than among hearing people.9 The Frenchmen Djourno and Eyries10 in 1957 are considered the first to stimulate electrically the auditory nerve on a deaf individual. During the 1960s and 1970s in the United States Michelson, Doyle, Simmons, and House pioneered techniques for cochlear implantation.11–14 The first commercially marketed single-electrode cochlear implant became available in 1972 by the 3M Company (St. Paul, MN). In the 1980s, multichannel implants were introduced and supplanted single-channel implants. Significant research for developing a multi-channel implant was performed mainly by Clark and his team in Australia and was marketed by the Cochlear Company (Englewood, CO) as Nucleus 22. In children, cochlear implantation in the United States began in 1980 with a 9-year-old boy who received the House/3M single-channel system. By 1982, 11 other children joined the ranks of cochlear implant users. Use of multichannel cochlear implants in the pediatric population in the United States started in 1987 and marked the beginning of a new era of rapid evolution. At present there are three companies with Food and Drug Administration (FDA) approval for marketing cochlear implant devices: the Australian Nucleus Cochlear Ltd. Company manufactures the Nucleus 24 device, the U.S. Advanced Bionics Corp. (Sylmar, CA) producing the HiRes 90K Bionic Ear device, and the Austrian Medical Electronics Corporation (Durham, NC) manufactures the MED-EL Combi 40+ system (Fig. 13–2). Cochlear implantation is presently an established modality of rehabilitating patients with severe to profound bilateral hearing loss who cannot benefit from hearing aids. The FDA criteria and guidelines for this procedure have recently expanded and are as follows: • Adults with a pure tone average (PTA) of more than 70 dB and an aided speech discrimination score less than 40% who have failed to benefit from hearing aid amplification and can undergo general anesthesia • Children with profound bilateral hearing loss, an unsuccessful trial period with hearing aids, and associated aural (re) habilitation for 3 to 6 months, age of 12 months or older, absence of medical contraindications to cochlear implantation, and compliance of the child and family Figure 13–2 The MED-EL cochlear implant. (Courtesy of MED-EL Corp., Durham, NC.) A thorough preoperative evaluation is of paramount importance in making a sound decision as to whether or not a patient is a candidate for cochlear implantation. In children, preimplantation findings are also the basis for developing (re) habilitation and educational intervention goals and guiding the expectations of parents following initial programming of the device. An in-depth review of the otologic history with special attention to the timing of the hearing loss onset, previous exposure to noise or ototoxic medications, history of meningitis, and family history of hearing loss can provide significant information and may be helpful in determining outcomes of cochlear implantation. Diagnosis of any other coexisting diseases, such as thyroid, renal, cardiac, and ophthalmologic disease, is crucial. The general health status is a very important factor to be considered in the preoperative evaluation. Chronic illnesses, such as asthma, diabetes mellitus, or cardiac conditions, raise issues related to surgery and anesthesia. The rigorous follow-up required for optimal performance with a cochlear implant must be assessed in the context of treatment demands for any existing medical conditions. In children, genetic evaluation should be obtained at the initial evaluation. Toxoplasmosis, rubella, cytomegalovirus, and herpes simplex (TORCH) titers should be obtained in suspected cases. Thyroid studies, urinalysis, and an electrocardiogram (ECG) should be ordered in cases suspected of associated thyroid, renal, or cardiac disorder. In adults, consultation with a human geneticist should be considered in cases with a family history of hearing loss or findings suggestive of a syndromic condition. Adults and postlingually deafened children should undergo conventional audiologic evaluation (PTA, speech discrimination, hearing in noise test, consonant/nucleus/consonant word testing). Prelingually deafened children require special audiologic testing (Early Speech Reception Test, Craig Lip Inventory, Meaningful Auditory Integration Scale, Infant-Toddler Meaningful Auditory Integration Scale). The role of an experienced audiologist in pediatric hearing loss is crucial in the evaluation of these children. Preoperative imaging studies should include computed tomography (CT) of the temporal bones, which may yield important information regarding the patency of the cochlea and the presence of congenital malformations, and assesses surgical anatomy.15 Magnetic resonance imaging (MRI) of the temporal bones is also very useful in the preoperative evaluation. In postmeningitis cases, high-resolution fast spin-echo T2-weighted MRI is very sensitive in identifying early labyrinthitis ossificans.16 Although cochlear malformations and labyrinthine ossification secondary to meningitis are not contraindications for cochlear implantation, they may present surgeons with technical challenges, require consideration of a particular electrode array, or limit the number of channels that can be inserted into the scala tympani.17 Extensive ossification and severe labyrinthine abnormalities may also affect auditory performance and the development of spoken communication.17 In children with narrow internal auditory canals on CT, MRI of the temporal bones may determine hypoplastic or absent cochlear nerves.18 Children with enlarged vestibular aqueducts, as detected by CT or MRI, should be investigated for Pendred’s syndrome because this is a very common finding in this entity.19 Developmental testing is warranted even without evidence of a concurrent disability. Assessment across developmental areas provides a baseline for performance and can also alert parents and professionals to risk factors for deficits that are subtle or not yet evident, as in the case of learning disabilities or pervasive developmental delays (PDDs). Children may present deficits that will inhibit overall performance as well as linguistic and auditory skill areas that cannot be easily determined without in-depth assessment. Conditions that affect behavior and attention should also be noted because they can create issues for postoperative programming as well as (re) habilitation. Hearing-impaired children are not by virtue of their hearing loss hyperactive or characterized by attention deficit disorder (ADD). Communication factors have always been considered critical in the evaluation of all children to establish candidacy for cochlear implants. The relationship of a child’s age when hearing loss occurs and the level of communication development to that point have received extensive attention in the literature. It is well accepted that early exposure to the spoken language code ensures the best opportunity for acquisition. Children under age 5 with hearing loss acquired after the foundations of spoken language have been established are able to utilize auditory input afforded by a cochlear implant. These children come to the cochlear implant evaluation phase having achieved at least some degree of auditory linguistic familiarity. If they have developed even minimal linguistic competency, documented baseline markers can serve as references against which postimplant progress can be measured. There is an extensive menu of evaluation instruments available to assess linguistic performance of children if there is indeed actual measurable performance evident. However, very young children with early onset of deafness may have no formal communication systems in either a spoken or signed modality. For these children, nonverbal interactions and vocalization patterns serve as the platform for evaluation.20 Communication is more than the speech code, and clinicians working with infants and young children are concerned with creating the child’s interaction profile and addressing components beyond phonemic production, vocabulary, and sentence length. Interactive non-verbal and vocal behaviors, communication strategies, and responsiveness to communication attempts of others are aspects of the superstructure on which verbalization is constructed. In additional, linguistic uniqueness among children, such as communication style and personality, should also be observed and documented.21 Linguistic proficiency should be judged by how well verbal and nonverbal communication conduct serves the child’s purpose. Ideally infants and young children and their parents should be enrolled in an intervention program as soon as the diagnosis of hearing loss is made. Assessment of educational and (re) habilitation options is best undertaken before the child receives a cochlear implant. Young children who receive intervention within the first 6 months of life have a greater opportunity to attain language and communication performance levels that reflect those of normally hearing children.22
Epidemiology of Hearing Loss
Impact of Hearing Loss
History of Cochlear Implantation
Candidacy Criteria
Preoperative Evaluation
Medical Evaluation
Audiologic Evaluation
Imaging Studies
Developmental and Communication Testing for Children
Assessment of Educational and (Re) habilitation Options
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree