Clinical Visual Electrophysiology
J. Vernon Odom
Monique Leys
George W. Weinstein
In this chapter, we introduce the reader to some of the principles of and major observations in clinical electrophysiology. Although this is a brief summary that must be limited in its depth of coverage, several other chapters in this volume point out the utility of electrophysiologic measures in the diagnosis of particular diseases or categories of disease1,2,3,4 or discuss their physiologic origins.5 Additionally, several brief books6,7 and major reviews8,9,10 are available for the reader who is interested in a more extensive introduction. An excellent reference volume, which is currently being revised, is available for the serious student of clinical electrophysiology.11
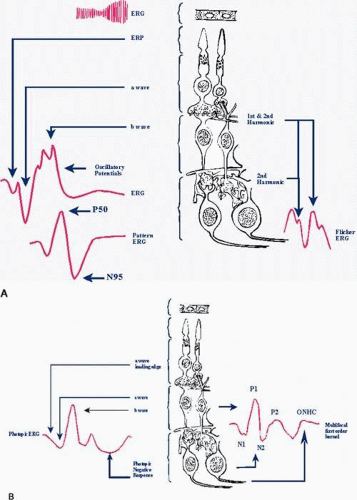
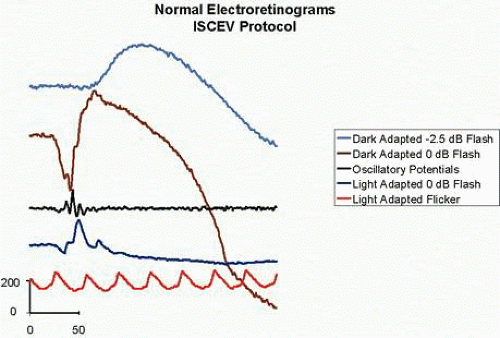
The primary means of electrophysiologic testing are electroretinography (electroretinogram [ERG]), electro-oculography (electro-oculogram [EOG]), and visually evoked potential (VEP) testing. Electroretinography, as it is classically performed using flashes of light, provides information primarily about the outer retinal layers (Fig. 1A and B). EOGs (and the c wave of the ERG) reflect variations in the standing potential across Bruch’s membrane and are altered by metabolic changes in the retinal pigment epithelium and outer retina (Fig. 1A). VEPs are cortical responses elicited by visual stimuli. Normal cortical responses are obtained only if the entire visual system is intact. Disturbances anywhere within the visual system can produce abnormal VEPs.
GENERAL CONSIDERATIONS
GENERAL TERMINOLOGY
As with any specialized area, clinical electrophysiology abounds with specialized terminology. Terms that deal with general characteristics of the stimulus or response are introduced here. Terms specific to a particular response are introduced in that particular section.
The stimulus for clinical visual electrophysiology is usually either diffuse light or patterned light. The stimulus may vary in intensity, duration, wavelength, rise time, fall time, spatial extent, and spatial location. A diffuse light stimulus varies in time but is uniform across a relatively large area of visual space. A diffuse light stimulus that appears and disappears suddenly and is of brief duration is termed a light flash or simply a flash. Diffuse, uniform stimuli are often presented in a sphere called a cupola, which provides Ganzfeld (full-field) stimulation. If the light appears and disappears periodically, it is said to flicker. The number of cycles of appearance and disappearance of light in one second equals the temporal frequency of the flicker in cycles per sec (cps) or Hertz (Hz).
A patterned stimulus varies not only in time but also in space. A patterned stimulus may appear and disappear as some areas become lighter and others become darker, or it may reverse so that light areas become dark and dark areas become light. The stimulator should perform these functions without any change in mean light level or luminance, which generally requires that light and dark areas appear equally in the pattern presented. The temporal frequency of an appearing-disappearing pattern is equal to the number of appearances (or disappearances) in 1 second. However, there are two reversals in a reversal cycle. Therefore, the number of reversal cycles in 1 second of the reversing pattern expressed in Hz—in other words, the temporal frequency—is one-half the number of reversals in 1 second. Because of the possible confusion between temporal frequency and the number of reversals, it is advisable to indicate both frequency and reversal rate when describing the reversing stimulus. The spatial characteristics of a patterned stimulus may be described either in terms of the visual angle (arc tan [size/distance]) of the elements in the pattern or in terms of their spatial frequency, which is the number of cycles of light and dark transitions in one degree of visual angle.
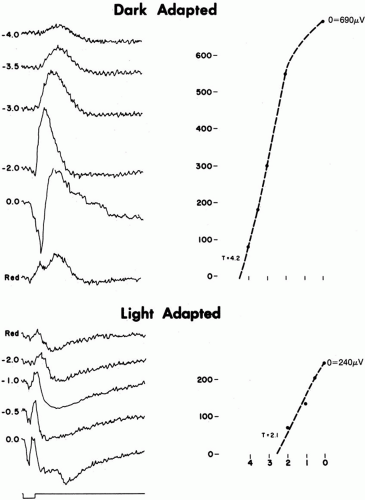
To isolate rod system from cone system function, stimuli are presented after the patient has been in the dark for some period of time. Responses recorded after a period of dark adaptation are termed dark-adapted, scotopic, or rod mediated. To isolate cone system function, patients are tested after a period in the light, usually at a light level that suppresses rod activity. Responses recorded after a period of light adaptation are termed light adapted, photopic, or cone mediated.
Electrophysiologic responses elicited by visual stimuli have a shape, or waveform, which depends on the characteristics of the stimulus and the patient. The response can usually be decomposed into components. If the stimulus is presented at a slow frequency, the response is said to be transient, and peaks of a specific polarity usually define the components. The peaks can be characterized by their size or amplitude, their polarity positive or negative the time to their maximum amplitude, which is termed implicit time for the ERG and latency for the VEP. If the stimulus frequency is fast, the peaks of the transient response become blurred so that the response often consists of only one or two peaks. The amplitude and implicit time or latency of these steady state responses may be measured; for example, 30-Hz flicker ERGs, or the response, may be Fourier analyzed and characterized by the amplitudes and phases of the Fourier components.
Irrespective of the response component measured, one may establish functions relating the component to a stimulus parameter, such as intensity, contrast, or frequency. If one varies the stimulus parameter and measures the response, one establishes a response function, such as an intensity response function. However, if one uses some response criterion, such as a criterion voltage, one determines sensitivity.12,13 If one determines sensitivity across a range of values, one determines a sensitivity function, such as a contrast sensitivity function. Although functions are usually determined using a set of separate responses, it is possible to determine response functions from a single stimulus presentation if the parameter of interest, such as intensity or luminance, is varied continuously (or approximately continuously). Such continuous stimulus presentations are called stimulus sweeps, and the responses elicited by them are termed sweep or swept VEPs or ERGs (Fig. 2). Generally, sweep responses are elicited by steady state stimulation as well as the signals analyzed in the frequency domain using a lock-in amplifier or Fourier analysis.14
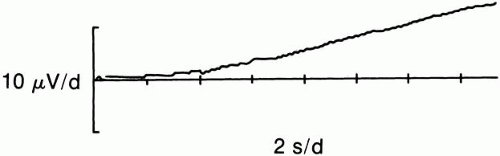 Fig. 2. Sweep 30-Hz flicker electroretinograms recorded under light-adapted conditions. Background luminance was 10 cd·m-2. During 16 seconds, flicker luminance increased from 0.0314 cd·m-2 on the far left to 314 cd·m-2 at the far right. (Redrawn from data presented in Bocquet et al.14). |
A number of terms have been used to describe severely abnormal responses, including flat, absent, extinguished, and nonrecordable. We use the term nonrecordable as a more neutral term. Nonrecordable indicates that under a specific set of stimuli and recording conditions, a response was not recorded. Often, with a change in stimulus or recording conditions, a response is recordable.
INTERNATIONAL STANDARDS
Members of the International Society for Clinical Electrophysiology of Vision (ISCEV) establish ophthalmic standards for various electrophysiologic tests (http://www.iscev.org).15,16,17,18,19,20,21,22,23,24 The accepted standards are reconsidered and revised, if necessary, on a regular basis. These standards are intended to assist in normalizing electrophysiologic testing by establishing minimal standards for diagnostic test conditions and analysis methods. Additional tests or analyses are always permitted. Because of inevitable variations due to choice of electrode, subjects, and other variables, the standards also require each laboratory to establish normal values and the limits of normal values for all tests performed in that laboratory. These normal values and their limits should be included in clinical reports and publications from the laboratory.
ELECTRORETINOGRAM
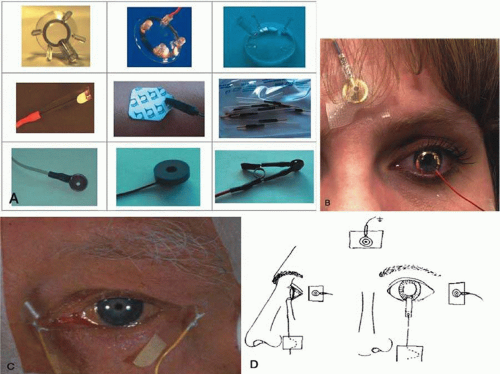
The ERG is the retinal electrical potential elicited by visual stimulation. Electroretinography dates back more than a century.25 The amplitude of dark-adapted, flash-elicited ERGs is usually several hundred microvolts and, therefore, does not require complex averaging instrumentation. A schematic ERG is presented in Figure 3. The era of clinical electroretinography began with the introduction of the contact lens electrode in the 1950s (Fig 4).
The different waves of the ERG can be useful in detecting retinal diseases, which may or may not affect the VEP. For example, early stages of retinitis pigmentosa may have little or no effect on the VEP, although the ERG may be severely altered. In sphingolipidoses, such as Niemann-Pick disease, retinal degeneration tends to parallel cerebral dysfunction and the ERG may serve as a useful noninvasive diagnostic test.
FLASH ELECTRORETINOGRAMS
Retinal Physiology and the Flash Electroretinogram
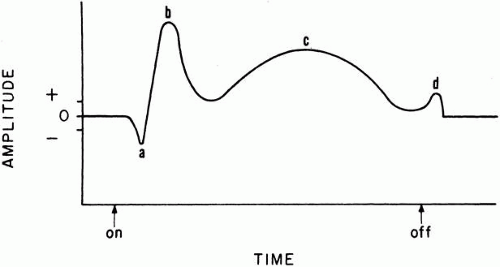
Under the proper conditions, the human eye has a subjective range of sensitivity of approximately 1010 (10 log units). The dark-adapted flash ERG b-wave range is approximately 1 log unit less than this. At the very lowest stimulus intensities, very near subjective threshold, under fully dark-adapted conditions, the ERG response consists of a slow negative deflection, termed the scotopic threshold response (STR), which appears to reflect the activity of amacrine cells, probably the AII type.26 As intensity increases, the STR decreases in latency and is replaced by the b wave about 1 log unit above subjective threshold; the a wave is not seen until the stimulus is 2 or 3 log units brighter (Fig 5). The c and d waves are not recorded under the ISCEV standard conditions. Both the a and b waves increase in amplitude and decrease in implicit time with increasing stimulus intensity.
When the eye is stimulated, a chain of vegetative and neural biochemical and electrical events are activated in the retinal neural cells, glial cells, and retinal pigment epithelium. The electrical voltages reflecting these events are volume conducted through the ocular media and tissues and recorded at the cornea as the ERG. Consequently, the various waves of the ERG reflect the algebraic summation of the activity of several processes. Granit27 advanced an analysis of the dark-adapted flash ERG, the main points of which are still accepted. He identified three retinal processes, abbreviated PI, PII, and PIII. Subsequent analyses have shown that each of the three processes can be subdivided and localized with even greater precision. Generally, PI-related processes derive from the choroid and retinal pigment epithelium and are primarily reflected in the c wave. PII-related processes reflect the activity of Müller’s cells at about the level of the bipolar cells and are primarily reflected in the b wave. PIII-related processes primarily derive from the outer retina at about the level of the photoreceptors and are primarily reflected in the a wave, especially in its slope. The relationship of the a-wave slope to rod photoreceptor currents has opened the door to the possibility of noninvasively monitoring human rod receptor dynamics in vivo.
Perception of light in the dark-adapted and light-adapted states is subserved by different retinal circuitry. As flash intensity increases under light-adapted background conditions, both the a and b wave appear at about 1 log unit above the psychophysical increment threshold. As flash intensity increases, the a and b waves increase roughly in parallel until the b wave reaches a peak, after which the a wave continues to grow and the b wave declines in amplitude and then grows again. The light-adapted ERG is dependent on retinal cells different from those required by the dark-adapted ERG. The dark-adapted PII is dependent only on the on-bipolar cells, whereas the light-adapted PII is dependent on both the on-bipolar and off-bipolar cells. The difference in timing between activation of the on-bipolars and off-bipolars results in a small potential difference at low flash intensities, which appears as an a wave, accounting for the simultaneous appearance of a and b waves in the light-adapted ERG.28
After the photopic b wave, a negative component can frequently be seen. This photopic negative component disappears if the spiking activity of ganglion and amacrine cells is eliminated pharmacologically.29,30 Consequently, in both animal models of glaucoma31,32 and glaucoma patients,33,34 the photopic negative component is greatly reduced or abolished.35
The cone-mediated (photopic) and rod-mediated (scotopic) systems each contribute distinct components to both the a and b wave. In each wave, the photopic components are seen first because of the directness of the neuronal connections of this system as compared with the diffuseness of the scotopic system. These components are termed a-photopic (ap), a-scotopic (as), b-photopic (bp), and b-scotopic (bs).
Both a and b waves originate in the outer retinal layers. The a wave is produced primarily by the photoreceptors; the b wave is produced by the Müller cells, largely at the level of the bipolar cells. The ganglion cells do not contribute to the ERG because their electrical signals are in the form of spikes that cannot be recorded externally. The ERG has been referred to as an amplitude-modulated (AM) signal as contrasted to the frequency-modulated (FM) signal of the ganglion cells. A normal ERG may be recorded in the absence of the ganglion cells or their axons (including the optic nerve), which occurs in many eye diseases (such as glaucoma and optic nerve injury or section).
Nutrition comes to the receptors through the choroidal vasculature and to the inner nuclear layer (bipolar, amacrine, and horizontal cells) from the central retinal system. A variety of disorders may affect one, but not another of these circulations. For example, disorders of the retinal circulation, such as central retinal artery occlusion, tend to unmask a large negative component as the positive (b wave) is reduced. The result has been described as a “negative ERG,” a sign of inner retinal ischemia. Conversely, insufficiency of the choroidal circulation, which occurs in ophthalmic artery occlusion or degenerative disorders such as choroideremia, halts the initial chain of events, thereby producing reduction of both ERG a- and b-wave amplitudes.
Because the stimulus light has a light-adapting effect on the retina, flickering stimuli tend to isolate the photopic components of the response, especially faster rates such as 30-Hz flicker. Flicker ERGs are usually of small magnitude relative to single-flash ERGs. Therefore, a flicker ERG is most informative when it is recorded using a summing and averaging device, which can extract relatively small signals from background interference. Typically, under clinical test conditions, 30-Hz flicker produces a sinusoidal response. Because the a and b waves are no longer clearly visible, the origins of the flicker ERG are uncertain. One line of argument suggests that the a wave, which diminishes with light adaptation, is suppressed. Therefore, the resultant responses consist mainly of b waves. Alternatively, Müller’s cells, which generate the b waves, are relatively less active at higher temporal frequencies,36 so the response to 30-Hz flicker might reflect neural activity, primarily the cone receptor potential.37 It is also possible to separate 30-Hz flicker ERGs into linear, first harmonic, and nonlinear, second harmonic components, which have an apparent latency suggestive of an outer retinal (receptor or bipolar cell) origin of the first harmonic components and an inner retinal (amacrine or ganglion cell) origin of the second harmonic.38 If one varies stimulation frequency, the first harmonic has multiple maxima and minima, suggesting that at least two sources combine to generate it and that these two sources cancel out at around 10 Hz.38 The two mechanisms are the on- and off-bipolar cells, which are about 180 degrees out of phase in the region of 10 Hz.39,40,41 If one blocks all postreceptor activity, there is minimal first harmonic response remaining, which indicates that the photoreceptors do not make the major contribution to the first harmonic in the 30-Hz region.41
Oscillatory potentials (OPs) appear as oscillations on the ascending portion of the b wave. The sensitivity of OPs to inner retinal diseases is consistent with suggestions that OPs derive from inner nuclear and/or the inner plexiform layers of the retina. However, individual oscillations may have different sources, as the number and characteristics of the OPs change with light adaptation and stimulus parameters.
International Standards for Clinical Electroretinography
Internationally accepted ERG standards were finally achieved in l98915 and have been revised subsequently.16 To comply with the international standards, a clinical laboratory must employ full-field stimulation. ERGs may be recorded using a variety of corneal electrodes, including contact lens, fiber, and foil electrodes. Contact lens electrodes have been preferred in the United States. Standard flashes must be 5 milliseconds (msec) or less in duration at their peak and have an intensity of between 1.5 and 3 candelas per square meter per second (cd·m-2·s-1). If a laboratory or manufacturer cannot generate a stimulus with these characteristics, they may calibrate the stimulus relative to the standard to generate a response of equivalent response characteristics. The light-adapted background must be between 17 and 34 cd·m-2 depending on the luminance of the standard flash.
Clinical ERG testing should assess the function of both cones and rods. Rod function should be tested using at least two ERGs recorded following a minimum of 20 minutes of dark adaptation with a minimum of 5 seconds between flashes. A dark-adapted ERG elicited by a low-luminance flash (2.5 log units below the standard flash) and an ERG elicited by a standard flash are suggested as standards for testing dark-adapted function. Dark-adapted OPs should also be recorded. The OPs should be measured in the dark using standard flashes and recording the second and subsequent flashes with a 15 msec separation.
To assess cone function, one should record a light-adapted ERG elicited by the standard flash following a minimum of 10 minutes of light adaptation. Flicker should be presented at the standard intensity, with the background at the same level as for the light-adapted ERG, and the frequency should be 30 Hz. Figure 5 presents examples of normal ERGs recorded under a range of stimulus intensities. Figure 6 presents normal ERGs recorded using the ISCEV protocol.
Some clinical electrophysiologists employ different stimulus conditions or record ERGs using skin electrodes placed underneath the eyes as their active electrodes. Although such recordings do not conform to the standard, they can be clinically useful. Recordings using skin electrodes may be especially useful in children who are too old to be swaddled or sedated but remain uncooperative with corneal electrode testing. Nonstandard conditions are most useful if appropriate norms and normal limits are available. Some countries, notably France, concerned about disease transmission through contact with the cornea and tear film require the use of disposable electrodes.
BEYOND THE STANDARD ELECTRORETINOGRAM
The ISCEV standards represent what its members regard as the minimum needed to perform a satisfactory, clinically useful ERG examination. Several modifications of the ERG protocol have proven particularly useful adjuncts to the ISCEV standard ERG: use of chromatic filters, calculation of intensity response functions, modeling of photoreceptor current, use of long-duration flashes, and measurement of the photopic negative response. It is not clear which, if any, of these techniques will gain widespread use, and in part, it depends on their careful implementation on commercial equipment as a “standard” protocol on that system.
Chromatic Electroretinograms
Most ERG protocols before the ISCEV standard employed chromatic stimuli as one means of isolating rods and cones. Consequently, most commercial clinical electrophysiology systems provide some means by which chromatic stimuli and backgrounds may be presented. Although the ISCEV standards eliminated this requirement, some diseases are best studied using chromatic stimuli. A notable example is the enhanced S cone syndrome, which is characterized by an enhanced response to stimuli that activate short-wavelength–sensitive cones.42,43,44,45,46,47,48,49 Additionally, experiments investigating the photopic negative response have frequently employed chromatic stimuli.32,33,34,50 Present evidence seems to support the idea that the S cone photopic negative response is more sensitive to glaucomatous damage than the L or M cone photopic negative response.51
Intensity Response Functions
Sometimes referred to as Naka-Rushton or Michaelis-Menton functions, intensity response functions have been useful in understanding the mechanisms of a number of retinal diseases.12 The basic strategy in employing intensity response functions is to record ERGs under a wide range of intensity levels from very dim flashes to very bright flashes. The major question that emerges and that has not been standardized, however, is how one fits the intensity response functions.52,53,54,55,56,57,58 Few of the manufacturers of electrophysiology equipment supply a built-in strategy for calculating an intensity response function of the b wave.
Modeling of Photoreceptor Current
When intensity response functions for the b wave are calculated, the a wave at higher intensities is accentuated. Using the leading edge of the a wave, it becomes possible to calculate a response that is largely dependent on the photoreceptors.59,60,61,62,63,64,65,66,67,68,69,70 Using models based on the properties of the photocurrent, it has been possible to make interesting observations in a number of diseases.44,66,67 Implementation of the technique requires specialized curve-fitting algorithms and a much brighter flash than that recommended as the ISCEV standard. The widespread clinical application of the technique depends on implementation of the brighter flash and curve-fitting algorithms by commercial manufacturers.
Use of Long-Duration Flashes
In his original work, Granit27 used long-duration flashes and demonstrated an off response in the dark-adapted ERG. Several Japanese scientists continued to use long-duration flashes.71,72 The work of Professor Miyake and colleagues73 demonstrated that differences in photopic on and off responses could usefully distinguish subtypes of congenital stationary night blindness, which was further explained through subsequent work by Sieving’s group and others.74,75,76 Subsequently, long-duration flashes have proven useful in understanding the mechanisms of a number of diseases, including cancer- and melanoma-associated retinopathies77 and juvenile X-linked retinoschisis.78,79
Measurement of the Photopic Negative Response
As noted earlier, the photopic negative response is dependent on ganglion cell activity and is reduced in glaucoma.32,33,34,50 Therefore, as standard procedures are developed and established for eliciting the response, the photopic negative response may become a useful adjunct to standard electroretinography, and because this response is larger and easier to record, it may supplement, or even replace, the pattern ERG (PERG).
PATTERN ELECTRORETINOGRAMS
Although the PERG was initially thought to have the same origins as the flash ERG, the PERG is now considered to be the sum of local luminance and pattern responses.80,81,82 In the steady state PERG, the local luminance responses have both an inner retinal and outer retinal origin, whereas the pattern response elicited by rapid sinusoidal modulation of sine wave gratings has only an inner retinal origin.83 The local luminance responses appear to represent the parallel activity of several systems whose relative importance varies with temporal frequency.38 Consequently, the relative importance of local luminance and pattern components of the PERG vary as a function of a number of stimulus parameters, including temporal frequency, contrast, and spatial frequency. One possible source of the inner retinal local luminance component is the so-called m wave. The m wave, originating in the inner retina, shows a negative deflection to both the onset and offset of light and shows spatial tuning, such that it is largest for intermediate spot sizes.84 However, eliminating the spiking activity of retinal ganglion cells does not substantially reduce the m wave.85
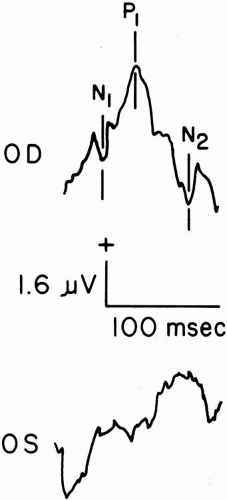
The transient PERG waveform appears superficially like the ERG elicited by luminance stimulation: There is an early negativity at about 30 msec, a positivity at about 50 msec, and a later negativity at about 95 msec. Because of this superficial similarity, the responses were originally labeled a, b, and after potentials, as those of the flash-elicited ERG. More recently, because the PERG waves have different origins than those of the flash ERG, additional nomenclatures have been proposed. We use the terms N30, P50, and N95 to describe the waves of the PERG. Other alternatives that have been used are p, q, and r and N1, P1, and N2. In enucleated eyes, the PERG N95 appears to follow the activity of the optic nerve response.86 Similarly, while leaving the P50 relatively unaffected,87 elimination of spiking retinal neurons eliminates not only the photopic negative response but also the PERG N95.
N95 appears to reflect activity from the ganglion cell layer more clearly than P50. N95 shows greater variation in amplitude with spatial frequency (Fig. 7) and is more affected in diseases of the optic nerve.88 P50, however, is altered in a number of diseases that affect primarily the outer retina.88 A ratio of P50 and N95 has been suggested as useful in discriminating a number of diseases that affect the optic nerve.88,89,90,91 Similarly, correcting VEP latency by PERG P50 latency may improve diagnosis and prediction of optic nerve disease.8 Examples of PERGs from a patient with pseudotumor cerebri of the left eye, which affects the optic nerve, are presented in (Figure 8. Holder91 recently reviewed his approach to clinical electrophysiology, which places the transient PERG at the center of electrophysiologic diagnosis because of its ability to differentiate inner retinal (ganglion and amacrine cell) from outer retinal (bipolar and photoreceptor). Holder’s review provides an excellent introduction to the range of uses of the PERG.
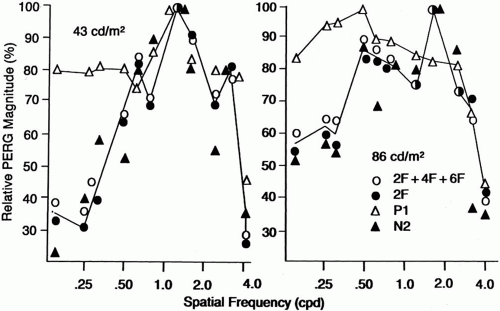 Fig. 7. Relative spatial tuning of 4-Hz pattern electroretinogram components at two light levels. Note that N95 shows greater relative spatial tuning than P50. The second harmonic and the sum of the even harmonics show tuning similar to N95. (Derived from data presented in Odom et al.80) |
International Standards for Pattern Electroretinography
ISCEV approved PERG standards in 2000.21 The standards emphasize the transient PERG; they discourage laboratories without special equipment from performing Fourier transforms on PERGs, which are an exact multiple of the stimulus cycles from recording or using steady state PERGs. A major emphasis of the guidelines is the care with which the signals must be recorded. Care is important because the small size of the signals that can be contaminated by electrical or physiologic artifacts, such as blinks with relative ease and the use of pattern stimulation, requires additional attention to refraction and accommodative status of the patient.
The PERG is seldom more than 5 μV; therefore, averaging is always necessary. Active electrodes, which do not interfere with the optics of the eye, are recommended. Because binocular recording is recommended, the preferred electrode locations are the active electrode on the cornea and the reference near the ipsilateral lateral canthus. The recommended stimulus is a reversing black-and-white checkerboard with a stimulus field between 10 and 16 degrees and a check size of approximately 0.8 degrees, reversing at two to six reversals per second (1 to 3 Hz) in a room with dim, indirect lighting. The stimulus contrast should be greater than 80%, with the white areas greater than 80 cd·m-2. The amplitudes and latencies of the P50 and N95 should be measured. If one records steady state PERGs as well, the amplitude and phase should be measured at the second harmonic of the recommended 8-Hz stimulation rate (16 reversals per second).
ELECTRO-OCULOGRAM
The EOG reflects metabolic changes in the retinal pigment epithelium that depend, in part, on the neural retina. Thus, this test supplies additional information concerning the retina and its supporting tissues. As a test of retinal function, the EOG serves primarily to complement the ERG. Together, these tests provide objective information about a portion of the visual apparatus. Often an abnormal EOG makes the diagnostician more certain of a marginally abnormal ERG.
An example of a patient undergoing EOG testing in a cupola is presented in Figure 9. Electro-oculography is based on the standing potential of the eye (Fig. 10). Since the cornea is positive with respect to the posterior aspect of the eye, the eyeball acts as a dipole.92 Therefore, eye movements can be recorded by electrodes arranged in pairs on the skin (usually horizontally) (Fig. 11), so that changes in polarity can be recorded and amplified with shifts in gaze (Fig. 12). The amplitudes of the voltages generated by constant-amplitude eye movements in the light and in the dark are the basic measures obtained in the EOG.
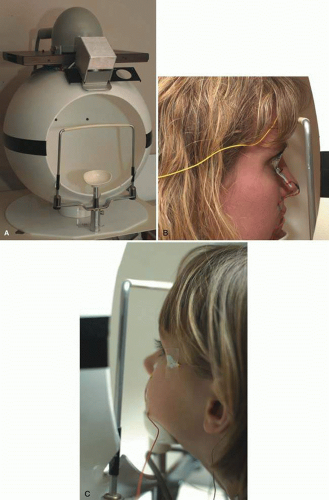 Fig. 9. A cupola used for Ganzfeld stimulation. Full-field or Ganzfeld stimulation is important to provide uniform illumination of the entire retina. Although a translucent corneal contact lens may be used, it is more common to use a cupola. A. Cupola manufactured by LKC Technologies (Gaithersburg, MD; http://www.lkc.com). A typical cupola has a method to control background luminance and flash intensity (possibly wavelength). The LKC cupola also has three light-emitting diodes (LEDs) (only two can be seen). The central one is for fixation in electroretinograms and flash visually evoked potentials. The two lateral LEDs are separated by 30 degrees and are used to control eye movements during electro-oculography. B. Adult seated with her chin on the chin rest. Note the active electrodes are Burian-Allen electrodes. The reference skin electrode is on the ipsilateral earlobe and the ground electrode on the forehead. C. Child with her chin on the chin rest. Note the active electrodes are skin electrodes placed on the lower lid. The reference skin electrode is near the ipsilateral outer canthus and the ground electrode on the forehead. |
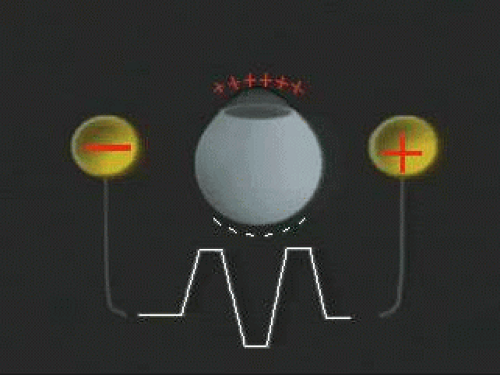 Fig. 10. The standing potential of the eye. For purposes of the electro-oculogram, the eye may be thought of as a battery. The anterior part has a positive polarity relative to the posterior part of the eye. As the eye shifts in position from side to side over a 30-degree excursion, skin electrodes record electrical changes; these can be amplified and recorded on a computer and displayed on an ink writer or cathode ray oscilloscope. (Adapted from a video frame obtained from Metrovision, Pérenchies, France: http://www.metrovision.fr.) |
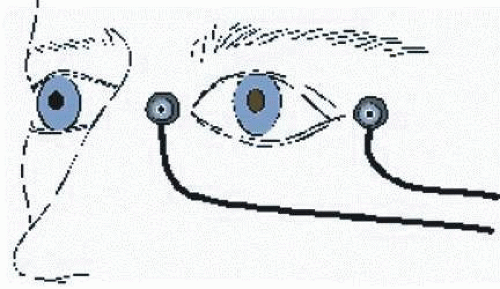 Fig. 11. The basis of the electro-oculogram (EOG). Subjects are seated before a cupola as portrayed in Figure 9. Skin electrodes are placed near the inner and outer canthi for recording the EOG. At regular intervals, the patient is required to move his or her eyes back and forth through an excursion of 30 degrees. In the cupola portrayed in Figure 9, this would be the distance between the two outer light-emitting diodes. Typically, EOG recording is bilateral. (Adapted from a figure provided by Metrovision, Pérenchies, France: http://www.metrovision.fr.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|