Clinical Tests of Fusion and Stereopsis
M. H. Esther Han
Robert H. Duckman
Why Test for Fusion and Stereopsis in Infants and Children?
The purpose of testing fusion and stereopsis is to assess a patient’s level of binocular function. The information a clinician expects and eventually obtains from the patient is often age dependent. The infant, preschooler, and school-aged child have different visual needs. Specific visual findings are necessary, therefore, to make a comprehensive binocular vision assessment with respect to the child’s needs. This chapter discusses the clinical significance of testing and the considerations to be made when administering tests of fusion and stereopsis.
In infants and preschoolers, the main objective in testing fusion and stereopsis is to assess for the presence of strabismus and amblyopia. The earlier such conditions are treated, the greater the prognosis for maximizing visual function (1). Performance on stereo tests is influenced by such factors as equal visual acuity in each eye and on ocular alignment (2). Stereopsis testing also provides a means of documenting changes in visual function during treatment (1). One of the main difficulties in examining this age group is their limited cooperation and maturity level. Children under the age of 5 years, in general, do not provide reliable verbal responses and can be uncooperative in a clinical setting (2). Some children will not respond to specific examination procedures that require eye patching or special lenses or glasses. A study conducted by Shute et al. (3) compared the success rates in measuring monocular visual acuity and stereopsis in subjects aged 1 month to 53 months. They determined that 75% of the infants tested under the age of 6 months (N = 15) tolerated the use of a patch. Only 22% of those 12 to 24 months (N = 18) and 47% of those 24 to 36 months (N = 15), however, were able to wear the patch and successfully complete monocular visual acuities. Interestingly, they found an inverse relationship with respect to stereopsis testing using the Frisby and the Lang tests. They found that 74% of those 12 to 24 months, and 88% of those 24 to 36 months were able to undergo stereopsis testing. Therefore when monocular visual acuity assessment is unsuccessful, stereopsis testing will increase the probability of detecting a vision disorder.
Clinical evaluation of fusion and stereopsis in the school-aged child (ages 6 to 8 years) is completed to determine any binocular dysfunctions that can negatively affect their sensory and motor function. Such deficits can interfere with the child’s visual efficiency in an academic setting. Limitations to testing a child can involve developmental delays in the gross motor or fine motor abilities; learning disabilities that can involve visual perceptual deficits and difficulty understanding instructional sets; attention-related deficits; and sensory integration deficits. The difficulty in examining this age group is that these conditions may have not yet been diagnosed. Instructions and procedures must be
tailored to the abilities of the patient and, at times, objective testing may be required when examining children with special needs.
tailored to the abilities of the patient and, at times, objective testing may be required when examining children with special needs.
Older school-aged children (ages 9 years and up) are in the stage of “reading to learn” as opposed to “learning to read.” The changes in the child’s visual demands involve smaller print text with less spacing, copying from the board, and visual accuracy when playing sports, such as baseball, basketball, tennis, or soccer. There is an overall increase in their need to be more visually efficient, particularly during periods of sustained near work. Testing in this group would emphasize endurance and stability of binocular function over sustained periods.
Clinical Tests of Stereopsis
Stereopsis involves the perception of relative depth under binocular conditions resulting from a horizontal retinal disparity that exists within Panum’s fusional area (4,5,6). Stereoacuity is a quantitative measure of stereopsis, which represents the smallest horizontal retinal image disparity that gives rise to a sensation of depth (7). Clinically normal stereoacuity should be less than 40 to 60 seconds of arc, depending on the test and the study cited (8). Age norms are 150 seconds of arc for ages 3 to 4 years, 70 seconds of arc for ages 4 to 5 years, and 40 seconds of arc for ages 5 to 8 years (9).
Stereoacuity depends on visual acuity or clarity of the retinal image, and ocular alignment (7). Even 1.00 D of uncorrected anisometropia can cause a reduction in stereoacuity (4). A study by Richardson et al. (10) in children ages 3 to 5 years also showed that refractive correction alone could improve stereoacuity to expected levels.
The main types of stereograms discussed in this chapter will be line or contour stereograms or global stereograms. Line stereograms involve the use of horizontal retinal image disparity to elicit the perception of stereopsis and global or random dot stereograms (RDS) which use computer-generated dot patterns that give rise to a central stereoscopic form when fused (11). In these patterns, some of the dots are displaced to one side for one of the eyes. When the two images are fused, the displaced dots appear to have depth (12).
A disadvantage of line stereograms is the presence of monocular cues that can be used to detect disparity (12). RDS tests do not have monocular cues and correct responses cannot be elicited unless there is bifoveation, and reasonably good visual acuity in each eye (12). Patients with a two-line difference in acuity can demonstrate considerably reduced stereoacuity (4). Given such stringent requirements to achieve RDS stereopsis, one study confirmed that local stereopsis is better than stereoacuity measured using RDS (13). Another advantage of RDS over the line stereogram is that those who are microtropic (whose objective angle of turn equals the amount of eccentric fixation) will not appreciate RDS stereopsis because, by definition, they are not bifoveal (11). Patients who are microtropic will appreciate gross stereopsis with line stereograms (>100 seconds) if peripheral targets are used.
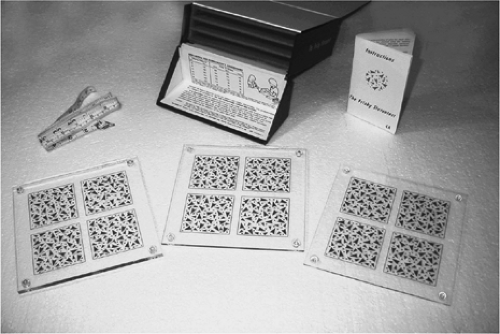
Frisby Stereo Test
The Frisby Test (Fig. 17.1) uses global stereo- grams that do not require the use of special glasses. The test consists of three test plates of different thicknesses (6, 3, and 1 mm). Each plate has four squares, one of which has a circular pattern that must be detected by the patient. The 6-mm plate is tested first because it has the largest disparity. The disparity can be increased by using either a thicker plate or decreasing the test distance (7). When testing at 40 cm, the disparities range from 480 to 15 seconds of arc (5). Normal stereopsis is considered to be 50 seconds of arc or passing the 3-mm plate at 70 cm or the 1-mm plate tested at 40 cm (7).
While administering the test, reflections must be minimized, and the test plate should be placed perpendicular to the patient’s visual axes. The clinician must also ensure that the patient does not make excessive head movements, because it will induce parallax (6,7). Three correct successive answers is the criterion used to determine the level of stereoacuity. Rosner and Rosner (7) also suggest placing a white sheet against the back surface to minimize background confusion. For testing children as young as 13 months of age, a forced-choice preferential looking (FPL) presentation can increase reliability of stereopsis responses.
This can be done by cutting the plates into quarters and placing them on a gray background (7). The clinician then presents two test plates, one with a stimulus and one blank. Broadbent and Westall (5) have shown that this test can be successfully administered to 65% of children under the age of 3 years. Saunders et al. (14) used a nonstereo practice plate with auditory reinforcement to first teach subjects how to perform the test. When administering the test with these modifications, they achieved a 64.7% success rate in infants aged 9 to 11 months, and 100% in children aged 18 to 23 months.
This can be done by cutting the plates into quarters and placing them on a gray background (7). The clinician then presents two test plates, one with a stimulus and one blank. Broadbent and Westall (5) have shown that this test can be successfully administered to 65% of children under the age of 3 years. Saunders et al. (14) used a nonstereo practice plate with auditory reinforcement to first teach subjects how to perform the test. When administering the test with these modifications, they achieved a 64.7% success rate in infants aged 9 to 11 months, and 100% in children aged 18 to 23 months.
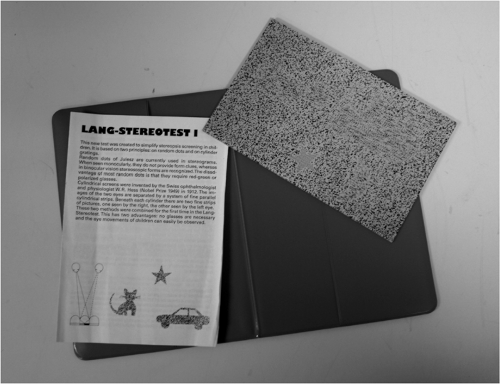
Lang Stereo Test I and II
The Lang Stereo Tests (Fig. 17.2) use RDS stimuli and do not require the use of special glasses. The Lang I card has pictures of a cat (1200 seconds), car (550 seconds), and a star (600 seconds) when used at 40 cm (7). The Lang II card has three pictures with smaller disparities (elephant with 600 seconds, car with 400 seconds, and a crescent moon with 200 seconds) and one nonstereo picture (star) that is seen by all patients (15). To reduce the disparity, Rosner and Rosner (7) stated that the test distance should be increased. Lam et al. (16) used 550 seconds of arc or better to define normal stereopsis in children 4 to 5 years of age. One disadvantage of the Lang test is that it does not measure stereoacuity but only screens for gross level stereopsis (17). As a screening tool, this test can successfully be used in children as young as 6 months and up to 4 years (5,7).
Random Dot E Test
The Random Dot E (RDE) test uses a global stereogram and also requires the use of polarized filters. It comes with a demonstration plate that has a raised “E” and two random dot stereogram plates; one is blank and the other has the stereoscopic “E.” The test distances typically used are 0.5 m (504 seconds of disparity) and 1.0 m (252 seconds of disparity), but it is also recommended to use 1.5 m (168 seconds of disparity) because this distance is more sensitive to both visual acuity reductions and binocular vision deficits. The goal is to present the stereograms to the child and have the child choose the plate with the “E.” Practicing with the demonstration plate ensures that the child understands the task. Rosner and Rosner (7)
stated that if the child is having difficulty understanding the task, try decreasing the working distance to 33 or 40 cm. In addition, they emphasized that the stereograms should be held slightly below eye level and slightly tilted so they are perpendicular to the patient’s visual axes, thereby minimizing reflections. The test is complete when four successive correct responses occur or when six trials have been administered (7). This test can be performed in children as young as 3 years of age (7). Children with poor figure-ground abilities, however, may show inconsistent responses because they have difficulty discerning a target from a visually busy background (9).
stated that if the child is having difficulty understanding the task, try decreasing the working distance to 33 or 40 cm. In addition, they emphasized that the stereograms should be held slightly below eye level and slightly tilted so they are perpendicular to the patient’s visual axes, thereby minimizing reflections. The test is complete when four successive correct responses occur or when six trials have been administered (7). This test can be performed in children as young as 3 years of age (7). Children with poor figure-ground abilities, however, may show inconsistent responses because they have difficulty discerning a target from a visually busy background (9).
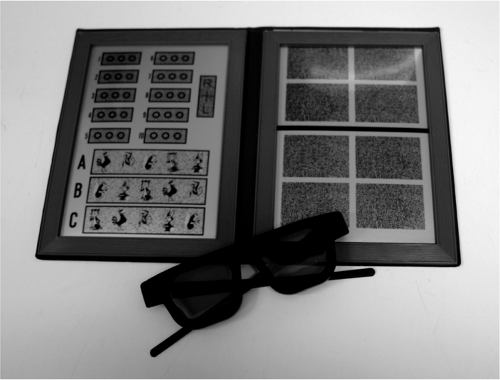
Random Dot Stereo Test
The Random Dot Stereo Test (Fig. 17.3) consists of three subtests, with two tests using line stereo- grams and one using RDS. It also requires the use of polarized filters. The randot forms subtest is a pure RDS test with two disparity levels, 500 and 250 seconds. The animals’ subtest (cat with 400 seconds, rabbit with 200 seconds, and monkey with 100 seconds), and the circles subtest (from 400 to 20 seconds) are line stereograms embedded within a random dot background to reduce the effects of monocular cue interpretation. The test is administered at 40 cm and excessive head movement and reflections must be minimized. Poor responses on this test may reflect language or communication difficulties. To reconfirm the patient’s responses, present the plate upside-down so the patient sees the stereograms in uncrossed disparity with the forms appearing to go into the page. The child can also point to reduce the need to communicate verbally. Rosner and Rosner (7) suggested that, when performing the circles subtest, running a finger across all three circles often helps the child appreciate stereopsis. The
randot forms and the animals subtest can be performed by 4 year olds and the circles subtest by 5 year olds (7). The mean stereoacuity achieved by age 6 years is 30 seconds, which is shown to improve to 20 seconds by age 11 years (10).
randot forms and the animals subtest can be performed by 4 year olds and the circles subtest by 5 year olds (7). The mean stereoacuity achieved by age 6 years is 30 seconds, which is shown to improve to 20 seconds by age 11 years (10).
Random Dot Preschool Stereoacuity Test
The Random Dot Preschool Stereoacuity test uses RDS stimuli and requires polarizing filters. It consists of three books developed by Birch et al. (18). The left-hand side of each book contains two-dimensional black and white illustrations of four test shapes in random order on the page. The right-hand page contains two sets of four random dot patterns with matching shapes, including three stimuli and one blank. Book 1 is made up of shapes with intermediate disparities (200 and 100 seconds); book 2 is made up of figures with fine disparities (60 to 40 seconds); and book 3 uses figures with course disparities (800 and 400 seconds). At each level, the child must identify two of the three stereoscopic stimuli present. If the child passes book 1, then book 2 is administered. If book 1 is not passed, then book 3 is administered. A child should not view all three books when performing this test.
Success rates determined by Birch et al. (18) were 89% to 95% in children ages 3 to 5 years, and 70% in children 2 years of age. These success rates were higher than the rates seen for the Titmus (see below) and the Randot Stereo Tests in children ages 2 to 5 years. Its efficacy was determined to be high with respect to stereoacuity measurement and as a screening tool. Lam et al. (16), however, found that randot stereoacuity was not a measure of biological function as a result of the random distribution of stereoacuity findings seen in normal children 4.5 to 5.5 years of age. They stated that a measure of biological function should show a Gaussian rather than a random distribution.
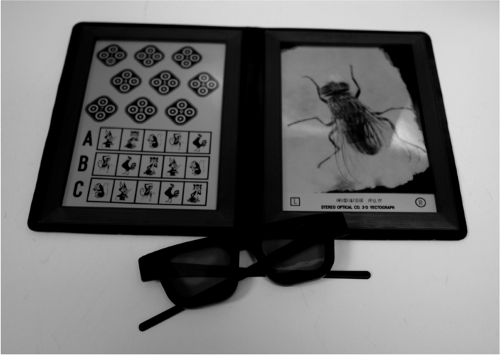
Titmus Stereo Fly Test
All three subtests of the Titmus Stereo Fly Test use line stereograms and require the use of polarizing filters (Fig. 17.4). The house fly subtest is a gross disparity target (3000 seconds), the animals subtest ranges from 400 to 100 seconds, and the circles subtest ranges from 400 to 40 seconds. To ensure a true stereopsis response, the house fly subtest can be repeated to depict uncrossed disparity by turning the test upside-down. The child will then attempt to point into the page when asked to touch the wings. These subtests are initially performed at 40 cm but, if the child is having difficulty discerning stereopsis, try decreasing the working distance (7). The house fly subtest can be used on children as young as 3 years, the animals subtest as young as 4 years, and the circles subtest as young as 5 years of age. The main disadvantage of this subtest is the presence of monocular cues, although Rosner and Rosner (7) indicate that the animals subtest has fewer cues, whereas the first five of the nine circles have strong monocular cues.
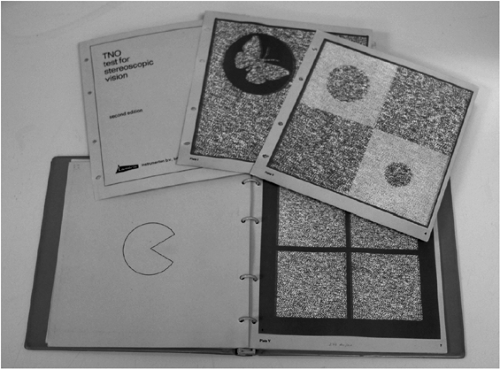
TNO Stereo Test
The TNO (Fig. 17.5) is the only stereo test that uses anaglyphic random dot stereograms and the only test that requires red-green filters. The screening subtest consists of three plates made of disparities ranging from 2000 seconds of arc when administered at 40 cm (7). The second subtest is the suppression subtest and the last is the graded stereoacuity subtest. This last test consists of 12 items divided over three pages. The disparities range from 480 to 15 seconds at 40 cm (13). Each page is divided into four squares with a random dot stereogram of a circle of which a 60° wedge has been removed. Each stereogram has a wedge missing at a different orientation. A main disadvantage of the TNO is that the red-green filters have been shown to cause more binocular dissociation as compared with polarized filters, which often results in
the underestimation of stereoacuity (6). Larson (13) suggested that red-green filters induce rivalry, suppression, and other binocular interactions that also lead to reduced stereoacuity measurements. Cooper (4) stated that chromatic aberrations could lead to different accommodative demands for each eye, which can also reduce stereoacuity. Finally, studies conducted by Simons and Elhatton (19) found that the green filter increases the contrast in the amblyopic eye, thereby artificially improving stereoacuity findings with the TNO.
the underestimation of stereoacuity (6). Larson (13) suggested that red-green filters induce rivalry, suppression, and other binocular interactions that also lead to reduced stereoacuity measurements. Cooper (4) stated that chromatic aberrations could lead to different accommodative demands for each eye, which can also reduce stereoacuity. Finally, studies conducted by Simons and Elhatton (19) found that the green filter increases the contrast in the amblyopic eye, thereby artificially improving stereoacuity findings with the TNO.
The screening subtest can be administered to children ages 2.5 to 3 years, whereas the graded stereoacuity test is successfully used in children ages 6 years and older (7). Broadbent and Westall (5) found that the graded stereoacuity subtest is an excellent screening device for amblyopia. They also suggested that children under the age of 2 years do not appear to understand the task. Williams et al. (20) found the prevalence of stereoscopic defects to be 2.1% to 3.2% in children ages 7 to 11 years when using the TNO.
Clinical Considerations
Filter Considerations
Frantz et al. (21) found that certain plastic prisms, but not glass prisms, cause a reduction in stereoacuity or an apparent failure to perceive stereopsis using tests requiring polarizing filters. Some specific observations noted were that the eye behind the prism may see both eyes’ targets or see only the fellow eye’s target, rather than its own. A thickness-dependent relationship exists that alters the polarization of the light as it passes through the prism. The polymerization process that occurs when manufacturing the plastic prisms creates polymer chains in an orientation that can cause the birefringence of light, which will polarize light as it passes through the plastic. This birefringent
property of the plastic is known to be dependent on the material’s thickness and on the angle the light enters the material. This polarization effect of the plastic prisms can be avoided by placing the prism behind the filter rather than in front of the filter, but this is not clinically practical. The clinician must be aware when using a prism with polarized vectographic materials to view the suppression controls monocularly through the prism at various angles of tilt to ensure that the prism is not affecting the polarization.
property of the plastic is known to be dependent on the material’s thickness and on the angle the light enters the material. This polarization effect of the plastic prisms can be avoided by placing the prism behind the filter rather than in front of the filter, but this is not clinically practical. The clinician must be aware when using a prism with polarized vectographic materials to view the suppression controls monocularly through the prism at various angles of tilt to ensure that the prism is not affecting the polarization.
Some stereo tests have polarized-free versions (Titmus Stereo, Stereo Reindeer, Random Dot Butterfly, Random Dot Figures, and the Random Dot E, Circle, Square). Hatch and Richman (1) compared the validity of the polarized-free tests with their polarized counterparts. They found no statistical difference in the stereoacuity attained with each version. Proper administration, however, is critical with the polarized-free tests. A small amount of tilt can prevent one image from being seen. Proper placement is ensured when suppression controls are seen equally in each eye. This is an important consideration when testing younger and more restless children.
Age Considerations
The sensitive period for binocular development is the time when binocular neurons are plastic, which Broadbent and Westall (5) describe as beginning a few months after birth and peak between 1 to 3 years of age. They also stated that neural development, rather than the development of accurate vergence, limits a child’s performance on stereoacuity tests. Clinically, cognitive factors also affect the measurement of stereoacuity. Studies have concluded that the apparent age-related improvement in stereoacuity is attributable to a child’s cognitive maturation rather than to the completed development of the visual system (22).
Different methods of obtaining responses from children, who are not cognitively mature enough to understand a test’s instructional set, have been investigated. Several authors have stated that operant preferential looking (OPL) presentation provides more reliable stereopsis findings in very young children (11,22,23). Based on OPL, Ciner et al. (22




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree