Meticulous removal of disease is a requirement common to the various types of cholesteatoma surgery. Although this may be pursued via one of a variety of described techniques for surgical access, the choice of which remain controversial, the aims of cholesteatoma dissection remain constant: eradication of disease, restoration of function, and prevention of complications. Within limits, surgery should be simple, versatile, and reliable: simple, so that other otologists can master the technique; versatile, so the skills can be obtained from experience in the greatest number of cases; and reliable with regard to efficacy and durability. Removal of the squamous epithelial matrix is common to all methods. This requires particular aspects of preparation, instrumentation, exposure, and clearance techniques.
21.2 Preparation
Dissection of cholesteatoma matrix often requires full concentration that is demanding and intolerant of interruption. Thus, appropriate preparation and arrangement of the operating table and instrumentation (as described in Chapter 18), plus clear surgical planning, allow the surgeon to “settle into the saddle,” avoid delays, and permit optimal dissection. For the novice cholesteatoma surgeon, it may be important to schedule more surgical time than what may be expected so as to avoid the need to perform the dissection hastily.
21.3 Instrumentation
Prompt access to the necessary instrumentation is essential for efficient cholesteatoma dissection. If working with a novice or in-training surgical assistant, it may be helpful to be involved in organizing a layout of instruments that places the frequently handled instruments (scalpel, suction, micro-picks) nearest the surgeon and the lesser handled at a greater distance (retractors, elevators, speculae, drill, diathermy). Also, numbering a few of the frequently used micro-picks (and maintaining a constant sequence) can help rapid identification and turnover.
Apart from surgeons’ personal preferences and the usual instruments common to most otology sites, some instruments have particular application that readers may find useful during matrix dissection. These are listed in ▶ Table 21.1. All micro-picks should incorporate robust, stiff shafts if possible; flexible, “whippy” types are inadequate or dangerous in many circumstances. Some instruments with specific attributes deserve comment.
Specialized Instruments | Role |
Hughes stapes mobilizer 223502 (KSG) | Matrix elevation over scutum and minor obstructions |
Kley footplate knife 223400 (KSG) | Fine adhesion division; dissection on stapes superstructure, malleus, facial nerve |
Large Plester sickle knife 223303 (KSG) | Extended reach; sharp dissection in anterior EAC angle, anterior attic (via attic defect) |
3-mm 90-degree micro-pick (M) | Incudostapedial disarticulation; elevation of matrix off attic defect edges, stapes arch, malleus handle |
Mini McGee fine alligator forceps 13–1040 (G) | Fine grasp of soft tissues |
Up-biting alligator forceps (M) | Transcanal removal of attic ossicles |
Holmgren self-retaining ear speculae 5 mm 123205 (KSG) 6 mm 123506 (KSG) 7 mm 123507 (KSG) | Transcanal exposure, dilatation of superficial soft tissues |
Other commonly used micro-picks | Sheehy weapon 23–0339 (G) Rosen elevator (M) 260000 (G) Plester knife (M) 251–500 (G) House curette (M) 13–0568 (G) 45° .75mm micro-pick (M) 13–0392 (G) |
Suppliers: Karl Storz Gmb (KSG); Gyrus/Olympus (G); Multiple suppliers (M) | |
Dissection of matrix or mucosa is often difficult when advancing over the rim of the scutum, in confined cells, or around minor obstructions. A curved needle or fine sickle knife may be successful but may lacerate the more friable sacs. Alternatively, a Hughes stapes mobilizer (▶ Fig. 21.1) is advantageous. This resembles the Beales elevator but is narrower. Increasing its longitudinal curve beyond the supplied shape improves its use within the less accessible sites. When very fine needlepoint dissection is required in accessible sites, a Kley knife (▶ Fig. 21.1) is highly effective, especially when dissecting on or around ossicles. The razor-thin tip is especially effective for removing epithelium or drum remnants off the stapes and the handle of the malleus.
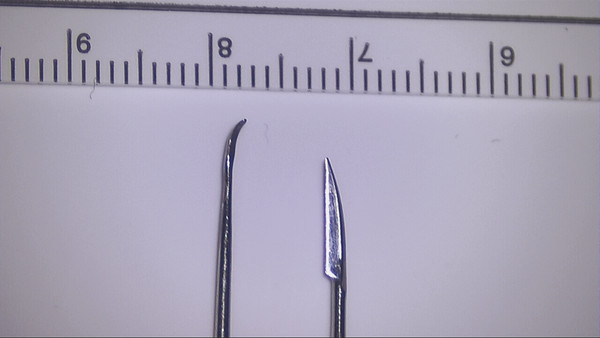
Fig. 21.1 Specialized dissection instrumentation. The Kley Knife (right) has a needle-sharp tip suited to fine dissection and a thin razor-sharp blade, useful in the confines of the oval window or similar sites. The Hughes elevator (left) allows matrix or mucosal elevation when progressing over the scutum or similar low-level obstacles or gentle, blunt dissection over vitals. Both are Karl Storz devices (Karl Storz GmbH and Co., Tuttlingen, Germany).
21.4 Case Evaluation
Cholesteatoma may be classified as congenital, acquired (attic, pars tensa, or combined), or atypical/unclassifiable (▶ Fig. 21.2). The presentation of the disease suggests its pattern, extent, and associated problems1 and also the appropriate dissection steps. For example, a pars tensa pattern without attic extension may be best managed by transcanal removal via fine sharp dissection; limited attic disease may submit to an atticotomy approach and fine blunt elevation; extensive disease may require a mastoidectomy and more robust removal. Audiology and a computed tomography (CT) scan may provide further direction with respect to the ossicular chain status and mastoid aeration, respectively. Deciding the overall management strategy is best left until this evaluation is completed. This evaluation is essential to accurately counsel the patient preoperatively, but to do so effectively, the surgeon will need to forecast the situation that is present at the conclusion of disease clearance, that is, immediately before reconstruction, to be able to assess the effect of disease removal, the prognosis of the appropriate repairs, and, therefore, the final outlook.
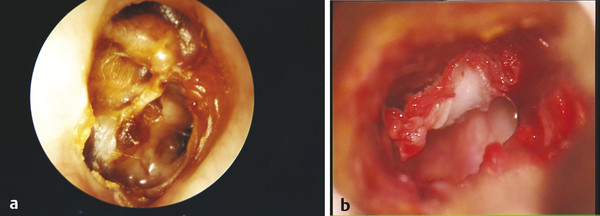
Fig. 21.2 (a) Advanced combined cholesteatoma due to long-standing tubal insufficiency. Gross tubal invagination is present, the ossicles are compromised, but mastoid extension may be limited into a poorly aerated cell system. (b) Atypical cholesteatoma pattern. Squamous epithelium covers the undersurface of the drum, possibly as a result of congenital origins, an adherent sac invagination, or epithelial migration via a drum perforation.
21.5 Cholesteatoma Surgical Scheme
Intraoperatively, a general stepwise flow to cholesteatoma surgery can be followed no matter which approach is favored. This involves the orderly sequence of (1) assessment of disease, (2) exposure of cholesteatoma, (3) removal of cholesteatoma, and (4) reconstruction of the defect.
Ideally, each step is completely finished before moving on to the next. Details of the first three of these are considered in the following discussion, with descriptions of the fourth covered in Part 4, Roundtable on Tympanic Membrane Reconstruction; Part 6, Roundtable on Tympanomastoidectomy; Part 7, Roundtable on Hybrid Tympanomastoid Surgical Techniques; and Chapter 41.
21.5.1 Assessment of Disease
Inspection of the tympanic membrane and exploration of the middle ear provide information about the nature, suspected origin, and extent of cholesteatoma that is helpful in anticipating the optimal surgical technique. Although preoperative imaging may provide useful information, at times it may be difficult to radiologically distinguish cholesteatoma from thickened mucosa, aural polyp, or middle ear secretions. Exploration also allows the surgeon to determine the status of the ossicular chain to avoid acoustic trauma during cholesteatoma exposure and dissection. Lastly, an initial assessment is made of the quality of hemostasis, which if greatly suboptimal, may impact intraoperative surgical decision-making.
21.5.2 Cholesteatoma Exposure
Several steps ensure adequate surgical access to the matrix for dissection that may be severely impeded or impossible should these be overlooked.
The essential first step in cholesteatoma removal surgery is adequate exposure of the stapes and its surrounds. Removal of matrix from this site is mandatory for a dry ear and functional hearing. In many cases this cannot be accomplished adequately via a posterior tympanotomy approach because the descending facial nerve often impedes optimal visualization to the posterior aspect of the oval window niche, the pyramidal process, and the ponticulus; mobilization of the facial nerve2 is very rarely necessitated. The transcanal vantage point gives the best access for instrumentation of the posterior mesotympanum (including the sinus tympani), but this often requires careful modification of the ear canal and/or meatus to be ideal. Also, cholesteatoma surgery requires long-term postoperative observation. Therefore, where possible, an adequately wide and straight external auditory canal (EAC) lumen is advantageous, both during and after surgery.
The superficial narrowing of the EAC is common, especially in children, and may severely impede post-surgical observation of the pars tensa. Also, narrowing at this site may occur after canal wall–up (CWU) surgery, due to minor secondary ossification effects. Superficial meatoplasty may be necessary. Hunsaker’s 1988 technique3 is recommended: the relatively simple technique is transcanal, the final canal introitus size is predictable, and it is readily combined with deeper surgery.
A tortuous EAC is managed by a canalplasty that involves anterior wall drill-back. This facilitates access for initial stapes clearance and also permits postoperative access to the anterior sulcus in the event of myringitis, granulations, graft breakdown, or simple debris accumulation. The combination of superficial meatoplasty and anterior canalplasty exposure thus permits optimal operative and long-term management (▶ Fig. 21.3a).
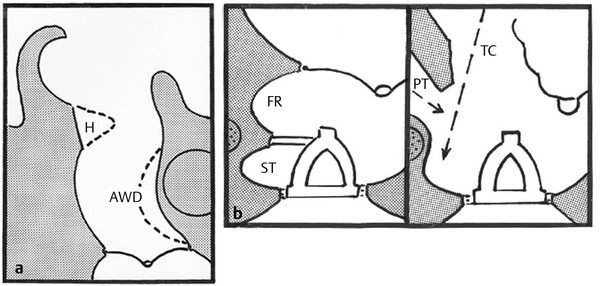
Fig. 21.3 (a) Transcanal access. A Hunsaker correction of superficial narrowing and an anterior EAC wall drill-back permit optimal long-term surveillance of the deep canal and facilitate management of external canal problems (debris, chronic myringitis). (b) Transcanal approach to the sinus tympani. The lateral approach offers the optimal approach to the sinus. Removing scutum back to the plane of the descending facial nerve can be supplemented by skeletonizing the nerve itself, for maximal access to the sinus itself.
If disease is noted in the posterior mesotympanum, a scutum drill-back is necessary. Anticipating this, the tympanomeatal flap is created more superficially (longer) than normal. Sufficiently wide scutum reduction, a step that is often inadequately performed by novice surgeons, affords visualization of the descending facial nerve, which may be skeletonized with a 2-mm diamond bur at its anterior aspect adjacent to the vestibule of the sinus tympani (▶ Fig. 21.3b). The resultant exposure, with proper patient rotation and positioning of the microscope, often permits inspection of the entire sinus tympani, requiring endoscopic assistance for dissection in a small minority. Drum composite grafting should follow scutum reduction to prevent pars tensa re-collapse.
Upon clearance of stapedial disease, management of attic disease may also be sought via the transcanal vantage point. However, the decision to use this method may be complicated by uncertainty as regards the extent of disease extension within the attic, into the mastoid, and/or into the supratubal recess4; endoscopy5 may help in only a proportion of cases. Transcanal enlargement of the attic defect may permit the removal of smaller sacs, but open surgery or a CWU procedure is needed for deeper invaginations. An essential principle to consider is that, no matter which vantage point is chosen for cholesteatoma dissection in the attic, isolation of the cholesteatoma “neck” at its junction of the residual tympanic membrane and complete lateral exposure of the sac should be achieved prior to attempted disease removal. Adhering to this ideal will maximize the odds of definitively removing the sac as a single self-contained specimen. In contrast, blind piecemeal removal of matrix from “around the corner” of the scutum or from a limited and narrow posterior vantage point through the antrum are not recommended.
When postaural surgery is required, ample transmastoid attic exposure is needed (▶ Fig. 21.4). This approach is facilitated by the wide exposure of the root of the zygoma. The following steps as described provide sufficient access without trauma to either the temporalis fascia or the underlying squamous periosteum, both of which may be needed to provide vascular flaps for subsequent reconstructions.6
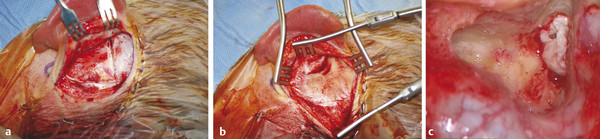
Fig. 21.4 (a) Postaural approach for CWU surgery, left ear. A hairline skin incision is followed by dissection in the avascular plane between skin and the underlying fascia-periosteal layer to expose the latter. A horizontal incision onto bone extends from the glenoid tubercle along the line of the avascular suprameatal crest, extending posteriorly 1–2 cm beyond the line of the skin incision. A second incision passes inferiorly from the crest along the posterior border of the mastoid to the tip. (b) Mastoid exposure. The mastoid periosteum is raised as an inverted-L flap. The temporalis fascia, muscle, and underlying pericranium are elevated intact, retaining vascular supply from the superficial and middle temporal arteries. These tissues can then be used for local vascular flaps if required. (c) Surgical approach to the attic. Vital structures to routinely identify include the lateral semicircular canal, then the posterior geniculate artery (central) that is a landmark identifying the site of the posterior genu. The descending facial nerve is seen immediately inferior.
If CWU surgery is employed, it is important for the surgeon to widely remove all of the bone of the lateral attic wall, including drilling far into the anterior epitympanic wall for access to the perigeniculate region and supratubal recess. To be done properly, this requires the skeletonization of the middle fossa dura. In some cases, a low tegmen and/or an anteriorly displaced lateral sinus will impede CWU attic visualization. These problems may be countered by “egg-shelling” the bone overlying each with a large diamond bur, then displacing the semi-rigid result, or by similarly isolating an island of thin bone, which is then displaced. Bone wax is used to temporarily keep the structures out of the line of inspection. During the approach to the posterior attic, bleeding from a small branch of the middle meningeal artery in the dura above may be troublesome; this can also be managed with bone wax.
21.5.3 Matrix Removal
Sac Characteristics
The nature of the cholesteatoma sac itself will influence the dissection and removal methods employed. The matrix may be saccular, infiltrative, finely atrophic, friable, or a membranous coating of the drum undersurface. Round/oval/globular sacs are common in attic and congenital cases. These have some tensile strength that permits gentle sac retraction with fine suction, plus sharp division of fine mucosal attachments that allows removal without rupture of the sac.
Infiltrative sac patterns are problematic in the anterior attic and in cellular mastoids, particularly around the semicircular canals. Fine, curved needle dissection may extract fine pockets but may carry some risk of local damage or residue. Likewise, infiltration around ossicles presents difficulties. Removal of the affected ossicle may be necessary, and when removed from the stapes or round window, chain repair is often best left until second-stage surgery.
Fine, atrophic squamous epithelium commonly results from drum collapse in pars tensa cases, secondary to chronic tubal insufficiency (▶ Fig. 21.2a). This is also a common problem in open cavity elimination surgery, where the tympanomastoid cavity lining is often particularly atrophic. The fine film may be fragile and adherent to the promontory, the remains of the ossicles, and the surrounding structures. Removal requires fine, sharp dissection to minimize trauma, but in the middle ear the mucosa should be spared if possible to limit subsequent adhesion formation. Absorbable gelatin film or Silastic may reduce postoperative adhesions although obliterative fibrosis often intervenes when mucosal loss is extensive and tubal failure persists. Suction will need to be delicate, using a fine lumen.
Friable sacs disintegrate with minor trauma. This less common fragile matrix variant is found in some congenital cholesteatoma cases and also when body tissues in general are of poor quality (▶ Fig. 21.5). Meticulous clearance is often necessary because the poor tensile strength impedes intact sac removal. Staged surgery to check for residual disease is mandatory in most of these cases.

Fig. 21.5 Cholesteatoma matrix in the attic. (a) Friable-type matrix enveloping the incus and stapes superstructure, right ear. Previous congenital cholesteatoma removal. The lenticular process of the incus has necrosed. The facial nerve and its attendant vasculature are evident in the left field. (b) Removal of superstructure matrix via an incision from the pyramid to the stapes head. The stapedius tendon thus stabilizes the stapes. The two “wings” of matrix can be dissected off the superior and inferior aspects independently. (c) Final disease clearance. A fine Kley knife has been used to clear the matrix from the stapes itself and off the facial nerve above and the promontory below, working from posterior to anterior.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


