Nasal obstruction is one of the most common complaints evaluated by the otolaryngologist. The differential diagnosis is broad, ranging from benign reversible causes to life-threatening diseases. In addition, patients may suffer from a combination of etiologies, further confusing the diagnosis. Surgical management is directed at the underlying origin of obstruction. The clinician therefore must use a careful history and physical examination as well as appropriate sinonasal imaging in accurately identifying the causes of nasal obstruction. To further illustrate these principles, we present two interesting cases of patients presenting with nasal obstruction.
This article focuses on the workup and treatment of two distinct cases of nasal obstruction. The first case has to do with a 24-year old male who presented with a brief seizure. Review of systems was positive only for longstanding right nasal obstruction. Imaging studies were consistent with a meningoencephalocele. The patient was taken to surgery for excision of the nasal mass and repair of the skull-base defect. Case two involves the treatment of a male with chronic nasal obstruction due to an S-shaped septal deviation and turbinate hypertrophy. The case illustrates the role of endoscopic septoplasty and shows how the endoscopic septoplasty technique is applied. The article also discusses the management of the enlarged turbinates.
Case one: 23-year-old male with seizure
A 23-year-old previously healthy male presented to the emergency room after experiencing a brief seizure. At the time, he had no headache, photophobia, fevers, chills, or neck stiffness. Review of systems was positive only for longstanding right-sided nasal obstruction. He denied a history of sinusitis, allergies, postnasal drip, epistaxis, or congestion. Facial pain, numbness, and swelling were absent. His remaining medical history was negative. On examination, nasal endoscopy revealed a large right-sided nasal mass. The mass was purplish and appeared smooth. The septum was bowed to the opposite side without any evidence of erosion.
Preoperative Evaluation
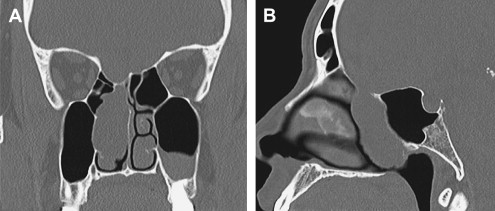
This patient presented with a nasal mass of unclear etiology. The first step in the work-up of any nasal mass is imaging. It is imperative to obtain imaging before performing a biopsy to avoid the potential downfall of biopsying a mass that contains brain tissue or meninges. If there is concern for intracranial extension or communication, both CT and MRI are necessary and complementary imaging modalities because a CT scan of the sinuses will demonstrate any bony defects in the skull base while the MRI will more clearly define the intracranial component and cerebrospinal fluid (CSF) signal. In this patient, the CT of sinuses demonstrated a large nasal mass extending from the skull base into the right nasal cavity. On sagittal views, a skull-base defect was apparent along the right fovea ( Fig. 1 ). The MRI scan demonstrated herniation of meninges through the skull-base defect into the nasal cavity ( Fig. 2 ). The nasal mass was determined to be a meningocele. The patient was subsequently taken to the operating theater for endoscopic repair of the meningocele.

Preoperative Considerations
The surgeon should be prepared to repair either a small or large skull-base defect, depending on intraoperative findings. Preoperative imaging often underestimates the size of the skull-base defect. Surgical repair varies with the size of the defect. A larger skull-base defect needs a stronger repair consisting of fascia and mucosal free grafts. A smaller defect may be repaired with a fat plug and mucosal graft. Although pedicled septal mucosal flaps are not routinely used to repair these lesions, the surgeon should be prepared to use them if the defect is large enough. In addition, preoperative scans may not be able to accurately differentiate between a meningocele and meningoencephalocele. It is ultimately up to the surgeon to correctly identify during the case whether the mass contains meninges only (meningocele) or meninges with brain tissue (meningoencephalocele). This identification is critical as it may alter the choice of surgical repair of the skull-base defect as discussed below. A lumbar drain is not recommended in the case of large skull-base defects because the drain, rather than helping to seal the defect, creates a greater potential for air to be sucked intracranially. Lastly, image guidance should be available and used if necessary.
Surgical Technique
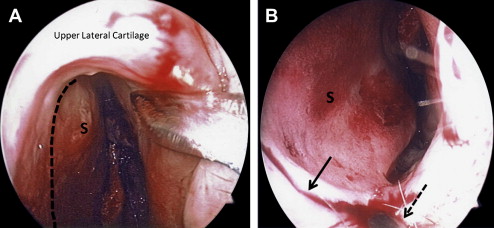
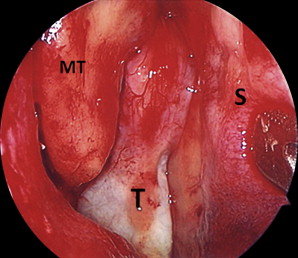
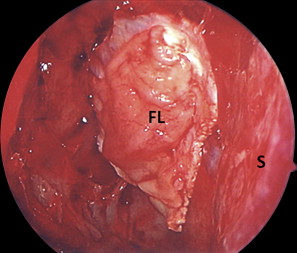
The patient was positioned in the supine position with the head of bed elevated at 30°. The nasal cavity was infiltrated with local anesthetic. Neuropatties saturated with topical cocaine (10%) mixed with normal saline and adrenaline were placed in the nasal cavity bilaterally. The uncinate process was removed using the swinging-door technique. Next, the natural ostium of the maxillary sinus was identified and widened. This was followed by an anterior and posterior ethmoidectomy. When the sphenoethmoidal recess was entered, care was taken not to enter into the sac of the meningocele. The sac was seen extending from the skull base into the nasal cavity adjacent to the septum and middle/superior turbinate in the sphenoethmoidal recess ( Fig. 3 ). The natural ostium of the sphenoid sinus was identified medial to the superior turbinate and widened in a medial and inferior direction. The anterior wall of the sphenoid sinus was removed to the level of the skull base. The remaining posterior ethmoids were opened to improve access and exposure of the skull base. The middle turbinate was removed flush with the neck of the meningocele sac at its exit from the skull base. The mucosa of the middle turbinate was saved to be used as a free mucosal graft later in the repair. The entire sac was visualized and incised to reveal its contents. When the sac was incised, both brain and meninges herniated through the opening. Half of the sac appeared to contain nonfunctional brain tissue. The sac and protruding contents were carefully debrided with a shaver until the extent of the skull-base defect could be visualized. When using the shaver, the tissue should be handled gently and every attempt should be made to identify and cauterize any vessels before debriding the tissue. This may be accomplished by using the suction in the shaver to capture the tissue before oscillating the blade. The surgeon should look at the tissue in the mouth of the blade and stop to cauterize vessels if visualized. Without this careful dissection, traumatized vessels could potentially retract intracranially and bleed. During this procedure, the surgeon should stop using the shaver as the sac gets smaller and as the shaver gets close to the skull base. At this time, the dissection should be performed meticulously with bipolar cautery. The bipolar cautery was used to effectively shrink the prolapsing brain tissue and meninges until it was flush with the skull-base defect. The mucosa around the defect was removed and the edges of the skull-base defect were freshened using a blunt probe and a sickle knife. Care was taken not to enlarge the skull-base defect while creating the ledge for the graft to be placed under. Proper closure and, ultimately, the success of the repair rely on the creation of a plane between the edges of the skull-base defect and surrounding dura. In the case of a meningoencephalocele, the prolapsed brain tissue is often found to contact the skull-base defect and to adhere to the dura around the defect. When this occurs, repair with a fat plug is not suitable because there is insufficient space intracranially to place the plug. The fat plug can be used in defects up to 1.5 cm if there is sufficient space intracranially in which to place the fat. Where there is prolapse of brain through the skull-base defect, the repair should be performed with two pieces of fascia lata covered either by a pedicled vascularized mucosal flap or free mucosal graft. Prior to placing the fascia, a malleable suction Freer elevator may be used to gently mobilize the brain tissue from the dural edges around the defect to create sufficient space to place the graft intracranially. In this case, the defect was filled with prolapsed brain tissue, so two pieces of fascia lata were harvested from the lateral thigh. The skull-base defect was measured using the tip of a 3-mm curette. A piece of fascia lata just slightly larger (by 5 mm on all sides) than the defect was fashioned. The first layer of fascia was then placed in an underlay manner between the skull-base defect and dura. The edges of the graft were smoothed out to eliminate any folds. Folds in the graft indicate that the graft is too large and may not seal the leak. A second piece of fascia was placed in an overlay fashion and finished with the free middle turbinate mucosal graft ( Fig. 4 ). The layers were sealed with synthetic tissue glue and two pieces of Gelfoam. The nasal cavity was packed with gauze soaked in bismuth iodoform paraffin paste. The placement of two large layers of Gelfoam before the nasal packing helps prevent the gauze from sticking to the grafts during removal. The packing was removed on postoperative day 1 and the patient was discharged from the hospital on postoperative day 2. Discharge medications included a 7-day course of broad-spectrum antibiotics and pain medication. The patient was instructed to refrain for 2 weeks from blowing his nose, lifting over 20 lb, or participating in strenuous exercise. The patient has made a full recovery without evidence of any further CSF leak.
Discussion
Intranasal meningoencephaloceles are rare with an estimated incidence of 1 per 40,000 live births. They are characterized by a protrusion of meninges and glial tissue through a skull-base defect into the nasal cavity. They may be categorized as spontaneous (congenital or acquired) or traumatic in origin. The majority are congenital anomalies thought to arise from the failure of closure of the neural tube. Thus, most are diagnosed early in the pediatric population as either an isolated malformation or as part of a congenital anomaly. There have been few reports of intranasal meningoencephaloceles presenting in the adult population. Most adult cases are diagnosed after recurrent episodes of meningitis or in association with a CSF leak. The diagnosis is made by imaging and not biopsy. A CT scan can delineate the skull-base defect, while the MRI may demonstrate CSF within the sac, the presence of brain tissue extending into the nasal cavity, and flow voids associated with vasculature. As discussed, the preoperative images may be misleading and fail to distinguish between a meningocele and a meningoencephalocele with a 100% certainty. Neurosurgery should be consulted to advise on the safety of brain resection in the case of a meningoencephalocele. Once the diagnosis has been made, surgical planning should begin. Endoscopic repair has been successful in most cases. The key to successful surgery is clear identification of the skull-base defect and secure placement of the graft. To provide improved access and allow for two surgeons to work simultaneously, a septal window may be created ( Fig. 5 ). This facilitates the dissection and removal of larger tumors in which retraction is performed by one surgeon while the other one dissects.