For over a century, surgical management of the inferior and middle turbinates has been an ongoing topic of discourse and disagreement. Treatment, either medical or surgical, of the inferior turbinate is required in cases of turbinate hypertrophy where the goals of therapy are to maximize the nasal airway, to preserve nasal mucosal function, and to minimize complications. Middle turbinate management, more controversial than inferior turbinate management, still lacks definitive consensus. This article reviews the anatomy, physiology, and pathology involving these two structures. Advantages, disadvantages, complications, and controversies surrounding the surgical management of the turbinates are discussed.
For over a century, surgical management of the inferior and middle turbinates has been an ongoing topic of discourse and disagreement. Treatment, either medical or surgical, of the inferior turbinate is required in cases of turbinate hypertrophy where the goals of therapy are to maximize the nasal airway, to preserve nasal mucosal function, and to minimize complications. Middle turbinate management, more controversial than inferior turbinate management, still lacks definitive consensus. This article reviews the anatomy, physiology, and pathology involving the inferior and middle turbinates. Advantages, disadvantages, complications, and controversies surrounding the surgical management of the turbinates are discussed.
Inferior turbinate
Inferior turbinate management must be considered in any discussion of sinonasal surgery because turbinate enlargement leads to obstruction of the nasal airway and limited surgical access to the paranasal sinuses in patients presenting with both sinus disease and symptomatic nasal obstruction. The inferior turbinate plays a major role in the regulation of nasal airflow and the development of nasal obstruction. Surgical turbinate reduction, either alone or as an adjunctive procedure during sinus surgery, septoplasty, or rhinoplasty, is often performed in patients after unsuccessful medical management of inferior turbinate hypertrophy. The literature describes multiple techniques of turbinate reduction, each with its associated advantages, disadvantages, and complications. In developing an understanding of which of these techniques is most effective, it is first important to discuss the anatomy and physiology of the inferior turbinate.
Inferior Turbinate Anatomy and Physiology
The nasal turbinates are important landmarks of the lateral nasal wall. The turbinate bones develop from a cartilage ossification center during the fifth intrauterine month. The inferior, middle, and superior turbinates are each composed of a thin bone for structural support and covered by an adherent mucoperiosteum. Stratified squamous epithelium is found on the anterior tip of the inferior turbinate, whereas pseudostratified ciliated columnar respiratory epithelium covers all other mucosal surfaces. The continually beating ciliated mucosa provides constant motion to the mucous blanket within the nose. This blanket acts as a cleaning and filtering system for the upper respiratory tract and also helps to maintain moisture within the nose. The turbinates maximize the effective intranasal surface area for rapid humidification and warming of inspired air.
Similar to the rest of the upper respiratory tract, the membranes of the turbinates are composed of ciliated, pseudostratified, glandular, columnar epithelium. The cilia beat in unison to propel the mucus from the nasal cavity toward the nasopharynx, where the mucus is then swallowed. Mucociliary transport relies on mucus production and ciliary function in healthy mucosa.
Both the blood supply and the autonomic nervous system control the secretions and level of congestion of the turbinates. The autonomic nervous system provides the general innervation to the nose, with the parasympathetic nerves supplying the resting tone and controlling secretions. The nerve supply originates from the facial nerve at the inferior salivatory nucleus and follows along the distribution of the facial nerve through the sphenopalatine ganglion. Overactivity of this parasympathetic innervation or underactivity of sympathetic innervation results in nasal congestion and obstruction.
The histology of the inferior turbinate deserves special consideration. Grossly, it is comprised of its epithelial mucosal layer overlying a basement membrane, an osseous layer, and an intervening lamina propria. The medial aspect of the mucosal layer is thicker and has more surface area than the lateral mucosa of the turbinate, as demonstrated by Berger and colleagues.
A thin acellular basement membrane separates the mucosal epithelium from the underlying lamina propria and the periostium of turbinate bone. The composition of the lamina propria includes loose connective tissue; a superficial inflammatory cell infiltrate with lymphocytes and other immunocompetent cells; serous, mucous, and mixed glands; and a rich network of thin-walled venous sinusoids. Affecting circulation through these sinusoids is a cyclic alternating constriction and dilation of the inferior turbinate vasculature, known as the nasal cycle, which occurs approximately every 2 to 7 hours.
At the core of the inferior turbinate is its central osseous layer of nonhomogeneous, cancellous, spongelike bone made of interwoven bony trabeculae separated by a labyrinth of interconnecting spaces containing fatty tissue and blood vessels.
Inferior Turbinate in Nasal Obstruction
The inferior turbinate plays a major role in the development of nasal obstruction. The nasal valve is the region of the nasal airway extending from the caudal end of the upper lateral cartilage bounded by the septum and the anterior portion of the inferior turbinate. The nasal valve provides approximately 50% of total airway resistance. As air flows through this narrow segment, it accelerates and the pressure drops, which can result in nasal valve collapse, especially if the upper lateral cartilages are anatomically weak. The erectile tissue of the nasal septum and inferior turbinate can also impinge on the nasal valve and increase resistance. Because the cross-sectional area of the nasal valve is small, even minor changes in inferior turbinate congestion can significantly decrease the total diameter and can have marked effects on resistance.
The role of the inferior turbinate in nasal obstruction is not only anatomic but may also be functional. Even in the presence of a normal radius, a sensation of obstruction can occur from turbulent airflow. Nasal airway resistance is an important parameter in nasal function. Airflow turbulence optimizes inspiratory air contact with the mucous membrane. Resistance must remain within certain limits for the perception of normal breathing. If resistance is too high or too low, a sensation of obstruction may occur. The turbinate, through its participation in the nasal valve, can act as a mechanical source of nasal obstruction. Alternatively, the turbinate can also play a role in subjective nasal obstruction if there is compromise in the function of its overlying mucosa.
Some nasal disorders, such as allergic and vasomotor rhinitis, are associated with the development of permanent turbinate hypertrophy producing chronic nasal obstruction. Others are associated with anatomic bony turbinate enlargement due to progressive ossification throughout adulthood. While chronic rhinitis is associated with hypertrophy of the mucosa of the entire nasal cavity, the inferior turbinates are central to the development of nasal obstruction, as they contain sinusoidal erectile tissue. Medical management of these disorders includes antihistamines, sympathomimetics, anticholinergics, and steroids. These medications provide symptomatic relief but no permanent cure. When optimal medical management has been unsatisfactory in the relief of nasal obstruction, surgical intervention is warranted.
Surgical Reduction of the Inferior Turbinates
Inferior turbinate reduction can be performed by various techniques that resect, displace, or decrease the volume of the turbinate.
Turbinate resection, total or partial, was once the surgical treatment of choice for turbinate hypertrophy. However, because of concerns about postoperative crusting, bleeding, and atrophic rhinitis, the treatment fell out of favor. Although very few studies actually demonstrated the validity of these concerns, the procedure became less popular with the development of other techniques.
Outfracturing of the inferior turbinate using a blunt elevator to displace the turbinate laterally is a technique with minimal morbidity. Improvement in nasal airway is transient, however, as the turbinate eventually resumes its original position. The technique also does not address the underlying pathology of hypertrophied turbinate mucosa. Turbinate outfracture, therefore, is often performed concomitantly with another procedure.
Submucosal injection of sclerosing solutions is another intervention that has been used in an attempt to decrease turbinate engorgement by blocking vascular channels. These results are transient, however.
Destructive procedures, including electrocautery, cryosurgery, laser surgery, and submucous resection, have been used to reduce the bulk of the turbinates by inducing scarring or by direct destruction. These procedures can be performed under local anesthesia in the operating room or in an outpatient office in most adult patients. Studies of some of these methods show variable long-term success and such complications as bone necrosis, synechiae, and prolonged crusting and bleeding.
Total Inferior Turbinectomy
In the early 1900s, most surgeons advocated inferior turbinectomy. The procedure fell out of favor after criticisms by such prominent rhinologists as Freer and because of concerns over the risks of postoperative hemorrhage, crusting, and atrophic rhinitis.
Resection of the inferior turbinate, although no longer widely performed, is still considered an option in turbinate reduction surgery. The technique involves fracture of the turbinate bone toward the midline and cutting along its lateral attachment. This can be done with the use of a nasal speculum and headlight or with endoscopic visualization. Controversies regarding this procedure are related to postoperative complications, including bleeding and scar formation, and presumed loss of physiologic function leading to atrophic mucosal changes, nasal crusting, and dryness.
Although resection of the inferior turbinate results in an increase in the volume of the nasal airway and the diameter of the nasal valve, it has been shown that this increase occurs at the expense of nasal physiology with decreased humidifying activity of the nasal mucosa, excess drying of nasal secretions, and resultant crusting. The value of inferior turbinectomy versus the risks of potential complications remains unclear. In some studies of partial or total inferior turbinectomy, complications of bleeding, crusting, and atrophic rhinitis were considered minimal, even in dry, dusty climates.
In one of these studies, 351 patients who underwent standard total inferior turbinectomy were evaluated for subjective improvement in nasal obstruction based on a six-question survey administered at 6 and 18 months postoperatively. All but nine of the patients (97%) reported improved nasal breathing at both time intervals.
In more recent comparisons of total inferior turbinectomy to other techniques, turbinectomy yielded good long-term improvement of nasal obstruction but also resulted in increased complications. In 2003, Passàli and colleagues randomized 382 patients with symptomatic inferior turbinate hypertrophy into six therapeutic groups and found that patients who underwent total or near-total turbinectomy experienced good long-term relief of nasal obstruction but also had a significantly higher percentage of crusting and bleeding compared with patients who underwent laser cautery, electrocautery, cryotherapy, or submucous resection.
Many surgeons understand that, while widening of the nasal airway to reduce resistance might be an important goal, that goal must be balanced against other goals that might lead to increased nasal resistance. Such goals include the maintenance of functional nasal mucosa with normal aerodynamic contours of the lateral wall to prevent turbulence.
Electrocautery
Methods of inferior turbinate electrocautery include linear surface electrocautery, bipolar electrocautery, and submucous diathermy. These may be done under local anesthesia in an operating room or clinic. The main disadvantage is that results are short-lived, but the procedure may be repeated as necessary. Additional disadvantages are postoperative pain, crusting, and scarring.
Meredith reported that 31% of 81 patients treated with both surface electrocautery and outfracture subjectively noted recurrence of nasal obstruction when followed for more than 33 months. Similarly, Warwick-Brown and Marks evaluated 307 patients who underwent submucosal diathermy with and without outfracture and noted that patient satisfaction with the procedure declined from 82% at 1 month postoperatively to 41% at 1 year. Edema and crusting after surface electrocautery has been shown to occur up to 3 to 6 weeks after treatment. Avoidance of bone injury with appropriate needle placement is also important in preventing bone necrosis and sequestration.
Radiofrequency Turbinate Reduction
Another technique presently in use in inferior turbinate reduction is radiofrequency volumetric tissue reduction (RFVTR), which aims at improving the nasal airway while preserving mucosal function. Radiofrequency heat is used to induce submucosal tissue destruction. The device, an electrode probe that induces ionic agitation at the cellular level, heats the turbinate tissue with little heat dissipation. Thermal injury only extends 2 to 4 mm around the active portion of electrode, thus only within the deep mucosa, sparing damage to adjacent structures or mucosal surfaces. The area of injury is replaced with scar-producing fibroblasts, as part of normal wound healing. Scar contraction leads to reduction of turbinate volume and relief of nasal obstruction. Because of the limited heat dispersal, RFVTR is different from submucous diathermy with electrocautery, where much higher tissue temperatures (up to 800°C) are thought to increase morbidities, such as crusting, pain, and bleeding, and have possible deleterious effects on mucosa.
Controlled studies examining RFVTR demonstrate statistically significant long-term improvement in several parameters, including increased nasal volume and decreased nasal airway resistance, based on acoustic rhinometry and decreased subjective nasal obstruction. An increase in turbinate edema may be seen in the first postoperative days. This is thought to be due to the acute tissue insult. The benefits of this procedure include preservation of nasal epithelium and mucociliary function. Also, the procedure can be performed under local anesthesia in an outpatient setting. The use of nasal packing is also generally unnecessary with this technique.
Laser Cautery
Carbon dioxide laser turbinate reduction can also be performed under local anesthesia. Use of laser turbinate reduction has gained greater favor especially because the procedure results in little blood loss and postoperative discomfort. Disadvantages of laser turbinate reduction include eschar formation, which may cause obstruction or, rarely, hemorrhage with sloughing of the eschar. Although the laser is effective at reducing hypertrophied mucosa through the induction of scarring and actual tissue removal, it is ineffective at removing turbinate bone and therefore not ideal in cases where bone reduction is necessary. Another disadvantage is that equipment for laser therapy is expensive and requires additional expertise, training, and safety precautions.
Cryosurgery
Cryoturbinectomy can be performed easily, also in an outpatient setting under local anesthesia. A typical treatment involves the application of a cryoprobe to the medial and lateral surface of the inferior turbinate, and freezing at −85°C for 60 to 75 seconds.
Because of its most pronounced effect on water-laden goblet cells, cryotherapy is thought to be most effective in controlling severe rhinorrhea associated with chronic vasomotor rhinitis. Although cryotherapy is considered to have relatively low associated morbidity, the duration of results is variable and usually temporary, thus requiring repeated applications.
Submucous Resection
First described by Spielberg in 1924 and further elaborated by House in 1951, submucous turbinate reduction involves removal of the inferior turbinate bone while leaving overlying mucosa intact. By maintaining the mucosal flaps, normal mucosal function is preserved, reducing the likelihood of complications, such as crusting and atrophic rhinitis. After a traditional submucous resection, as described by Spielberg, only minimal crusting is typically observed along the incision site. Another reported advantage of this method is very low incidence of postoperative bleeding. The effectiveness of traditional submucous resection is even more pronounced in cases of conchal bone hypertrophy. The primary disadvantages of traditional submucous resection are the potential for mucosal shredding in inexperienced hands and the need for nasal packing postoperatively.
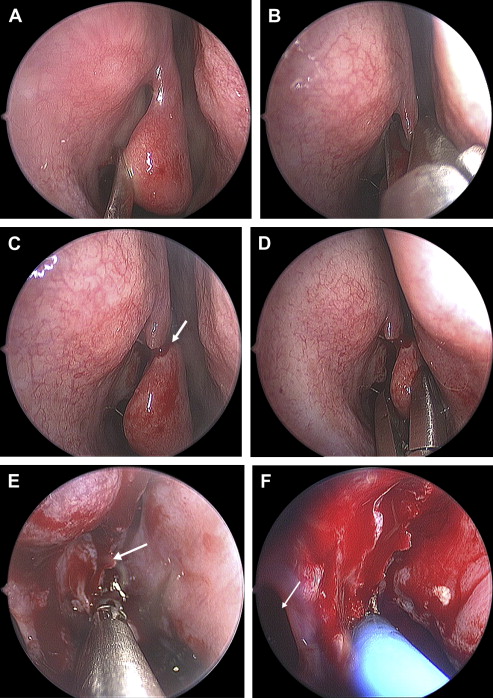
More recently, the use of the microdebrider in submucous resection of the inferior turbinate has proven quite successful with even fewer complications of crusting and similar favorable outcomes. This technique of submucous resection of the inferior turbinate is the method of choice for the senior author and is depicted in Fig. 1 . The first turbinate is infiltrated with 1% Xylocaine and 1:100,000 epinephrine. The turbinate head is then pierced with a turbinate blade (2.9-mm microdebrider tip, Medtronic Xomed, Jacksonville, Florida), which is then inserted into the anterior face of the inferior turbinate and used to dissect a submucosal flap by tunneling along the length of the turbinate, moving anterior to posterior (see Fig. 1 A). The microdebrider, rotating at 3000 rpm, is then run along the length of the turbinate and moved in a steady circular fashion with the intent of removing the stromal tissue from inside the turbinate. The overlying mucosa is completely preserved. In patients with significant hypertrophy of the posterior portion of the inferior turbinate, a second entry with the turbinate blade is made in the midposterior turbinate and the microdebrider is run in a similar manner. The turbinate is then outfractured using a 7-mm chisel placed at the medial aspect of the turbinate along its length, allowing for additional lateralization (see Fig. 1 B).
Chen and colleagues compared microdebrider-assisted inferior turbinoplasty using this technique to standard submucous resection in 160 patients with inferior turbinate hypertrophy. Patients were randomly assigned to either treatment group. Outcome measures were conducted preoperatively and at 1, 2, and 3 years after surgery. These measures included anterior rhinomanometry and subjective symptom improvement. Compared to preoperative values, subjective complaints, including nasal obstruction, sneezing, rhinorrhea, and snoring, improved significantly in both groups as did rhinomanometric measures.
Each of options available in the surgical management of nasal obstruction due to inferior turbinate hypertrophy is associated with complications. Each, also, has its own advantages and disadvantage in comparison with other options, and each has proven to be effective. Most studies suggest that when any of these options is performed well, results can be favorable, albeit transient in some instances. Before undertaking surgical intervention, it is important to ensure that all medical therapy options have been fully explored as surgery may not be effective in some patients with medically treatable conditions. Ultimately, the surgeon’s preference and expertise guide the selection of any particular technique. While the problem of nasal obstruction can have severe adverse effects on quality of life, treatment is almost always elective. One possible exception is severe life-threatening sleep apnea.
The best treatment is the one with minimal morbidity that yields the best response. Jackson and colleagues have proposed an algorithm as a staged protocol of increasingly invasive interventions:
- 1.
Medical management
- 2.
Laser reduction as an initial surgical office procedure when medical management is ineffective
- 3.
Partial anterior turbinectomy or submucosal resection, with or without microdebrider assistance, when office-based procedures fail
- 4.
Rarely, total turbinectomy if all other treatment attempts do not succeed
Finally, other causes of nasal obstruction should be addressed in the full assessment of a patient with nasal obstruction including the need for septoplasty, nasal valve correction, and rhinoplasty.
Middle turbinate
The middle turbinate is an important landmark in endoscopic sinus surgery. Resection of the middle turbinate remains a source of considerable debate and controversy in the surgical management of sinonasal disease. Despite the volume of literature both supporting and disparaging the removal of the middle turbinate, objective evidence either favoring or discouraging the procedure remains sparse. The current rhinology literature remains unclear regarding the best management of the middle turbinate during sinus surgery.
A great deal of controversy surrounding middle turbinate resection appears to be based on each surgeon’s personal philosophy regarding nasal physiology and anatomy. The debate obviously divides those determined to preserve the middle turbinate from those who propose varying degrees of turbinate excision, from partial to near-total removal.
Historically, the practice of middle turbinate resection was condemned. Messerklinger felt that, with few exceptions, the middle turbinate should be preserved. Partial removal was only to be reserved in cases of concha bullosa or paradoxical middle turbinate, and resection in these instances was always conservative. Conversely, Wigand and colleagues recommended partial or total middle turbinate resection as a routine step in virtually all endoscopic sinus surgeries. Both approaches to the middle turbinate have yielded successful outcomes, thus supporting surgeons on both sides of the issue. Yet, even with the good results seen with either approach, surgeons who either routinely resect or those who routinely preserve the middle turbinate vehemently disavow the opposing approach. Surgeons often cling to their respective positions on the issue quite passionately. Even in the face of such fervor, however, surprisingly few studies provide a hard scientific rationale in the approach to middle turbinate preservation or resection. In fact, virtually all of the literature on the subject of middle turbinate resection is based on nonrandomized retrospective data. In 2001, Clement and White reviewed over 500 papers describing turbinate surgery over a period of 35 years and not one randomized controlled study was identified. Their conclusion is essentially the overarching theme regarding middle turbinate resection—there really is no conclusive evidence supporting or discrediting the procedure. For every study that appears to favor one approach, there are others that endorse the opposing view. Thus, management is largely based on personal surgical belief or anecdotal experience.
In the following sections, we review the relevant middle turbinate anatomy. The discussion includes the rationale for its resection in sinus surgery and some of the controversies and theoretical problems associated with removal of the middle turbinate. The sections specifically address the validity or actual occurrence of complications stemming from removal of the turbinate.
Middle Turbinate Development and Anatomy
The middle turbinate is embryologically derived from the ethmoid bone. Structurally, the middle turbinate can be divided into three segments. The anterior third attaches superiorly and vertically to the skull base at the horizontal plate of the ethmoid bone just lateral to the cribriform plate. This attachment may be pneumatized in up to 12% of the population, thus forming an aerated vertical segment of the middle turbinate, which may be referred to as the interlamellar cell. This aerated segment is subject to the same inflammatory and infectious processes as other sinonasal mucosa, thereby resulting in obstruction of drainage from the ethmoid infundibulum. The middle segment of the middle turbinate, the ground or basal lamella, inserts laterally, attaching it to the lamina papyracea. It is this attachment that divides the ethmoid sinus into anterior and a posterior compartments. The posterior segment of the middle turbinate is attached inferiorly and oriented horizontally, inserting onto the perpendicular process of the palatine bone anterior to the sphenopalatine foramen. The anterior/superior portion of the middle turbinate, an important surgical landmark, forms the medial boundary of the frontal recess. Therefore, lateralization of the middle turbinate can lead to structural narrowing of the frontal sinus outflow tract and frontal sinusitis. Also to be considered is the variability in the shape of the middle turbinate wherein there may be paradoxical curvature or pneumatization. Pneumatization of the head of the middle turbinate, or concha bullosa, is also a variation of special consideration in patients where this may cause nasal obstruction or obstruction of the osteomeatal unit.
Management of the Middle Turbinate
The middle turbinate debate is largely centered on one crucial question: How much of the middle turbinate can one safely resect? The effect of middle turbinate resection on normal sinus and nasal physiology remains uncertain. The nasal turbinates are thought to function collectively to direct and assist in lamination of nasal airflow, to humidify and warm inspired air, and to provide a mechanical defense against particulate matter. In comparison with the inferior turbinate, the middle turbinate is significantly smaller, contains less vascular and erectile tissue, accounts for a negligible portion of nasal airway resistance, and is believed to have less functional significance.
Despite this evidence, as well as literature supporting the safety of middle turbinectomy, the procedure continues to provoke a considerable amount of controversy, particularly regarding lateralization of the turbinate remnant as a factor promoting postoperative frontal sinusitis. Other concerns include loss of a significant surgical landmark, development of atrophic rhinitis, postoperative hemorrhage, and anosmia. The controversy surrounding middle turbinate resection appears to be based on personal philosophy regarding nasal physiology and anatomy.
Middle Turbinate Resection
Several indications for the removal of the middle turbinates in endoscopic sinus surgery are now more generally accepted. Some cited indications for middle turbinate resection include treatment of conchae bullosa that participate in nasal obstruction or prevent access to the middle meatus in the “crowded nose,” removal of disease involving the turbinate, creation of surgical access to the paranasal sinuses, and treatment of headache related to the middle turbinate syndrome where contact between an enlarged middle turbinate and either the septum or lateral nasal wall leads to stimulation of the sensory portion of the trigeminal nerve.
The techniques for middle turbinate resection also vary. Kennedy and Sinreich describe a technique where the turbinate is split in the middle and only the lateral portion is removed, leaving the medial portion intact to function physiologically. Wigand describes resecting the posterior third of the middle turbinate when performing any retrograde sphenoethmoidectomy. Morgenstein and Krieger describe a technique that involves cutting the superior attachment of the middle turbinate, then snaring the anterior two thirds. Freedman and Kern describe resection of the middle turbinate to within 0.5 cm of the skull base as an integral part of all headlight intranasal sphenoethmoidectomies. In the majority of patients, this maneuver addresses disease involving the turbinate (eg, polyposis or osteitis); turbinate resection is advocated regardless of the amount of pathology involving the middle turbinate.
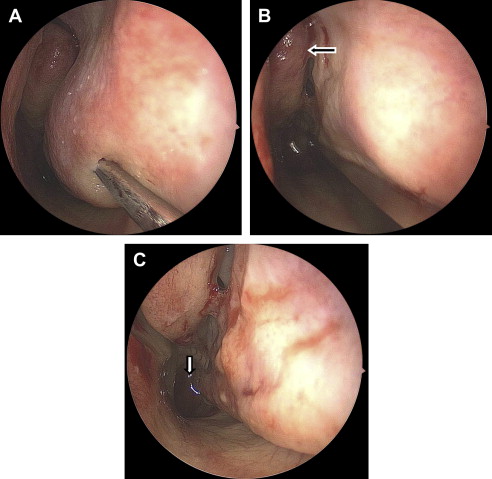
The senior author employs a middle turbinate resection technique ( Fig. 2 ) that is a modification of the techniques described by Wigand. It is performed with the use of a 0° 4-mm telescope. Initially, the middle turbinate is fractured medially toward the septum using a Freer elevator to expose its vertical, superior attachment (see Fig. 2 A). This attachment is incised with a straight turbinate scissor at its most anterior portion (see Fig. 2 B and C). The body of the turbinate is then grasped with straight Wilde forceps (see Fig. 2 D) and pulled inferiorly and posteriorly, leaving at least 0.5 cm of the superior attachment and basal lamella to preserve as landmarks (see Fig. 2 E). The most posterior attachment of the middle turbinate is then incised using through-biting forceps, thereby completing the partial resection. As prophylaxis against intraoperative or postoperative hemorrhage, the remainder of the posterior attachment is then suction-cauterized to coagulate small branches of the sphenopalatine artery (see Fig. 2 F).