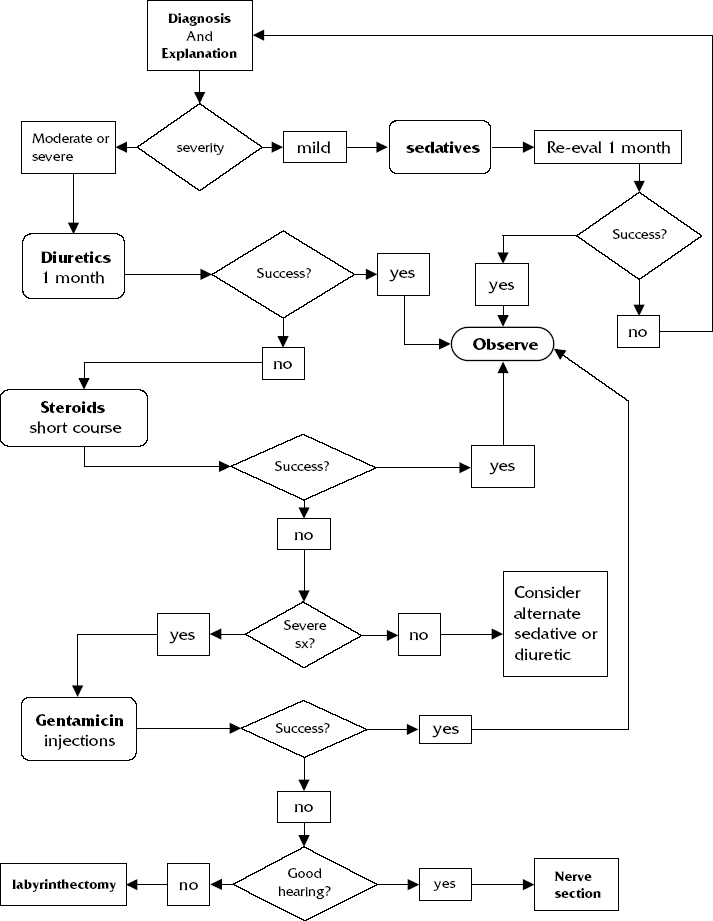
Diagnosis Diagnosis precedes treatment. It’s a simple concept, yet diagnostic uncertainty is a major frustration in treating Meniere’s patients. A complete diagnosis includes estimates of the severity of symptoms, medical and nonmedical influences, and assessment of previous therapy. Each of these can affect treatment decisions. The literature about Meniere’s disease is not very helpful either. Although Meniere’s disease is uncommon—some even say it is rare—there are many single-author reports in the literature with huge numbers of patients. How is this possible? Clearly there is doubt about the diagnosis. Great results occur if the disease is absent. The diagnosis is made on the basis of the history. The official definition of the American Academy of Otolaryngology– Head and Neck Surgery (AAO–HNS) seems reasonable.1 A good, classic history with the criteria as outlined is adequate proof of Meniere’s disease, even if another disorder is found. The following symptoms must be present for a confident diagnosis of Meniere’s disease: Some further diagnostic points to consider are that the physical examination is usually normal, and tests are optional. Many tests are interesting for research purposes, but no test proves or disproves the diagnosis of Meniere’s disease. Vestibular testing for clinical purposes is poor. An audiogram should be done; an electronystagmogram (ENG) is usually perfomed as well, to confirm the presence of function in the other ear. Destroying the only functioning ear would result in disaster. The summating potentials from electrocochleography and other tests are interesting but should not alter clinical treatment decisions. Figure–1 presents a flowchart for a treatment plan for Meniere’s disease. Treatment Once we have a firm diagnosis, what is the next step? This chapter considers only the treatment of vertigo spells. Meniere’s disease patients frequently have varying degrees of imbalance, which is not treated in the same way as vertigo. First we consider the effect on the patient’s activities of daily living. Once again, we have to ask the patient: How frequent is the dizziness? How severe? Does it prevent him or her from going out? Driving? Walking? Working? Specific treatment may not be needed. The first step in treatment is explanation. The patient must understand as much as possible about the unpredictability of the prognosis. Symptoms may resolve. Although effective treatment can usually be found, the fix may not be quick. The risks and alternatives of treatment should be discussed. Even patients with mild disease should be aware of the range of treatment options from the conservative to aggressive surgery. Nonspecific factors that exacerbate most dizziness should be addressed: (1) avoidance of stress if possible, (2) inadequate sleep (consider getting an hour more sleep per night), (3) inadequate irregular meals, (4) side effects of medications, and (5) high caffeine intake (some dizzy patients drink 20 cups of coffee a day. No wonder they are dizzy!). Adequate explanation is all some patients need. For others, a temporary sedative will ease their anxiety over the disabling period. In treating this disorder, it is important to remember that people do not die of Meniere’s disease. We are treating a symptom. The patient will help decide if and when more aggressive therapy is desired. If more than a weekly average of an hour of dizziness occurs, most people will want help. This may be either a single spell or multiple spells. Of course, this guideline should be individualized. Many patients will demand treatment for lesser degrees of vertigo and, if the treatment is safe and inexpensive, it may be reasonable. Any treatment should be continued for at least 1 month, if possible. There are many treatment options. Some are placebos, but we don’t know which ones, and patients may love them. Some treatments that I do not use because of lack of evidence and/or poor clinical results include hypnosis, lipoflavinoids, megavitamins, nicotinamide, nicain, allergy injections, dietary glucose manipulation for hypoglycemia, and glycopyrrolate. The use of vestibular rehabilitation or habituating exercises to treat intermittent symptoms is illogical. Accepted treatments include sedatives, diuretics, steroids, intratympanic gentamicin, and surgery. Figure 46-1 Meniere’s disease decision flowchart. SEDATIVES Although sedatives are not a good long-term solution, they are frequently adequate to cover brief (up to 2 weeks) periods of difficulty with dizziness. The patient should be told about side effects, such as sleepiness. The list of interactions with other medications is considerable. There are many sedatives on the market. With some general principles in mind, the specific choice is probably not critical. Most patients with mild dizziness achieve adequate relief from meclizine taken up to three times per day. Meclizine is not more effective than many other drugs but because it has fewer side effects, it is popular. For severe vertigo, one of the benzodiazepines such as diazepam is reasonable. Most patients do not need these. It is important to moderate the dose in the elderly or frail. Alprazolam or dimenhydrinate are useful as well. The key is to use sedatives briefly. Prolonged use of sedatives impairs compensation, prolongs symptoms, and produces a suboptimal result. Also, patients frequently become psychologically or physically dependent on sedatives if they experience initial relief. Persistent use causes reduced efficacy and shorter effect, necessitating increasing amounts. DIURETICS AND SALT RESTRICTION I rarely recommend one of these without the other. The salt restriction is not severe. I simply instruct patients not to add salt to their food and to avoid salty foods such as potato chips and salted crackers. Hydrochlorothiazide is the most commonly used diuretic, but differences in efficacy among different diuretics have not been shown. Potent diuretics such as furosemide are not more effective. I usually use a combination of hydro-cholorothiazide/triamterene to avoid potassium loss. That is standard procedure, but I have a new wrinkle. Some research papers4–6
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


