(1)
Department of Ophthalmology and Visual Sciences, University of Iowa Hospitals and Clinics, Iowa City, IA, USA
The so-called branch retinal arteries are in fact arterioles [1] (see Chap. 2). Therefore, the universally used term “branch retinal artery occlusion” is incorrect. Branch retinal arteriolar occlusion (BRAO) is a common ocular vascular occlusive disorder. From the point of view of etiology, clinical features, and visual outcome, it can be classified into the following types.
Classification of BRAO
Based on my studies [2, 3], I divided BRAO into permanent and transient types.
1.
Permanent BRAO: This is usually due to an impacted embolus or sometimes due to vasculitis or other causes (see below). In my study of 151 eyes with BRAO, 88 % had the permanent type.
2.
Transient BRAO: This is invariably due to an embolus which temporarily occludes and then migrates, resulting in restoration of normal circulation (see below). In my study of 151 eyes with BRAO, 12 % had transient BRAO.
3.
Bilateral Idiopathic Recurrent BRAO: This is a rare syndrome. There are several reports of this type in the literature [4–10]. Gass et al. [4] in 1986 first described nine cases; they wrote that the findings in their cases suggest, although they did not prove, that the occlusions are caused by focal vascular changes and not emboli. They postulated that the multiple BRAOs are caused by a localized reaction, perhaps immune mediated, in the retinal arterial wall.
The findings of these cases resemble those of Susac’s syndrome.
Susac’s Syndrome
Susac and colleagues have described various aspects of this syndrome since 1979 [11–26]. Susac’s syndrome is a rare disorder. It is thought to be caused by autoimmune-mediated endotheliopathy that affects the microvasculature of the brain, retina, and inner ear, resulting in occlusions leading to a characteristic clinical triad of encephalopathy, BRAO, and hearing loss. Since the first description of this syndrome, many reports have been published, mostly anecdotal cases but a few with more than four patients. Rennebohm et al. [23], based on the activity and course of the syndrome lasting ≤2 years, classified it into three major types – (1) monocyclic (self-limited disease, without recurring), (2) polycyclic (with relapses), and (3) chronic-continuous (with a prolonged, chronic, continuous course).
Dörr et al. [27] in 2013 presented a comprehensive review of Susac’s syndrome, based on 164 publications reporting 304 individual patients with Susac’s syndrome. The following information is based on their review. Among the reported cases, 78 % were female – in 5 % of the women, it was related to pregnancy. Racially 81 % were white, 4 % African Americans, 8 % Asians, 1 % Hispanics, and 5 % Turkish. Range of age of onset was 8–65 (mean ± SD 31.6 ± 10.4) years. The youngest reported patient with Susac’s syndrome has been a two-and-half-year-old female from India [28]. Based on the classification of Susac’s syndrome by Rennebohm et al. [23] (see above), Dörr et al. [27] found that 54 % had monocyclic disease, which fluctuated and was self-limited within 2 years, without recurring; 42 % had polycyclic disease that relapsed and continued beyond 2 years. The chronic-continuous type was seen in only 4 %. The active period of the disease ranged from 1 to 252 (mean ± SD 21 ± 37) months. Numbers of relapses ranged from 1 to 10 (mean ± SD 2.4 ± 1.8) on a follow-up of 8–56 years (mean ± SD 41 ± 46 months). BRAO was seen in 82 %. In BRAO cases, visual acuity was reduced in 71 %, visual field showed scotoma in 98 %, and fluorescein fundus angiography revealed arterial wall hyperfluorescence in 96 %.
Recurrent unilateral and bilateral BRAO can also be caused by recurrent embolization from lesions in the carotid arteries or the heart as well as those from Susac’s syndrome. I have seen bilateral BRAO in 13 % of 141 eyes with BRAO [3]. The following are two examples of patients with Susac’s syndrome whom I have seen.
First Patient [12]
A neurologist referred a 28-year-old woman in her 28th week of pregnancy to my clinic on June 2, 1989. She gave a history that on May 30, 1989, she suddenly developed a black spot in front of the lower, inner quadrant of her right eye at about 1 PM. She had noted periodic imbalance over the previous 2 months. On June 2, ophthalmic evaluation showed 20/20 visual acuity in both eyes. Fundus examination showed a superotemporal retinal infarct secondary to superior temporal BRAO in the right eye (Fig. 15.1a) and visual field defect (Fig. 15.1b). Vasculitis was seen at the site of occlusion of the involved BRAO (see arrow in Fig. 15.1a). The anterior segment and vitreous in the right eye showed no abnormality. Carotid duplex scan was normal, antinuclear antibody titer was elevated at 1:160 (speckled pattern), and the erythrocyte sedimentation rate was 42 mm/h.
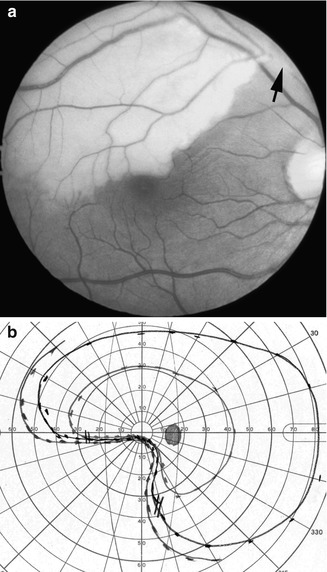
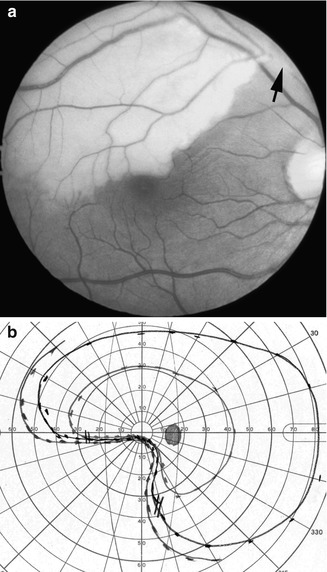
Fig. 15.1
The right eye on June 2, 1989. (a) Fundus photograph shows infarction of the superior temporal retina in distribution of the superior temporal retinal arteriole and site of vasculitis (arrow) (Reproduced from Hayreh SS and Zimmerman MB [144]). (b) Visual field plotted with a Goldmann perimeter shows inferior nasal sector defect, sparing central fixation
On June 11, the patient developed slurred speech and personality changes. Later the same day, she had difficulty sitting and walking, with a tendency to fall to the left. She was admitted by the neurologist to a local hospital and had computed tomogram (CT) scan of the brain, electrocardiogram, screening blood work (including antinuclear and cardiolipin antibody titers), blood cultures, visual evoked potentials, and deep-venous Doppler sonograms of the lower extremities, and all were normal. The erythrocyte sedimentation was 50 mm/h, and contrast echocardiography revealed a right-to-left shunt with Valsalva maneuver, consistent with a patent foramen ovale. She was treated with intravenous heparin and improved slightly, although her dysarthria persisted. She was discharged on June 18 taking subcutaneous heparin (5,000 units every 12 h).
Over the next 48 h, her speech deteriorated and she developed decreased interest in her environment, perioral numbness, and unsteady gait with falling to the right. She was readmitted to the hospital and given intravenous heparin. T2-weighted magnetic resonance imaging of the brain performed on June 22 showed multifocal areas of increased signal intensity in the deep white matter, anterior corpus callosum, and brain stem.
One week later, she was transferred to the neurology department of the University of Iowa Hospitals and Clinics for further care. On arrival, her vital signs were normal. She had a systolic murmur in the heart. She had a flat affect, and she was dysarthric. There was a retinal infarct in the superior temporal sector of her right fundus, as before. Her gait was broad based and ataxic. She had bilateral Babinski’s signs. After admission, intravenous heparin was continued. Her mentation worsened; she became disoriented, responded minimally to questions, and had little interest in her environment. No new lateralizing signs developed. A repeat carotid duplex scan was normal. Repeat contrast echocardiography showed a right-to-left shunt. Thyroid studies and C-reactive protein and double-stranded deoxyribonucleicacid antibody titers were normal. Blood cultures were negative. Somatosensory evoked potentials and brain stem auditory evoked potentials were normal. An electroencephalogram showed diffuse slowing. Formal neurobehavior testing showed moderate to severe impairments in virtually all assessed aspects of cognitive function including attention, memory, behavioral organization, praxis, and language. She also showed perseverative tendencies and poor awareness of her condition. These findings were believed to be consistent with multifocal brain dysfunction. A CT scan of the brain without contrast done on July 1 was normal. Anticoagulants were stopped, and cerebrospinal fluid (CSF) examination revealed a protein concentration of 207 mg/dl with a glucose concentration of 55 mg/dl (serum glucose concentration 89 mg/dl), 2 white blood cells/mm3, a normal myelin-basic protein concentration and IgG index, and absent oligoclonal bands. Another CT scan without contrast done on July 5 showed small areas of hypodensity in the genu of the corpus callosum and the periventricular white matter. Four days later, she delivered a healthy infant boy. A cerebral arteriogram done 4 days after the delivery was normal. A second CSF examination showed a protein concentration of 144 mg/dl, a glucose concentration of 59 mg/dl, 1 white blood cell/mm3, and a normal immunoelectrophoresis pattern.
Ophthalmic evaluation on July 17 showed visual acuity of 20/20 and normal intraocular pressure in both eyes, and the fundus demonstrated multiple branch retinal arteriolar occlusions in the left eye and a cotton-wool spot (Fig. 15.2a). Fluorescein fundus angiography showed occlusion of three retinal arterioles during the transit phase (Fig. 15.2b) and, during the late phase, showed mild staining of the wall of occluded arterioles (Fig. 15.2c). There was marked resolution of the previously noted retinal infarct in the right eye (Fig. 15.3). Visual field plotting revealed corresponding field defects in both eyes. The anterior segment and vitreous in both eyes showed no abnormality. Audiometry demonstrated mild bilateral sensorineural hearing loss. Serum complement levels were mildly elevated (C3 196 mg/dl [normal range 70–176 mg/dl] and C4 45 mg/dl [normal range 16–45 mg/dl]).
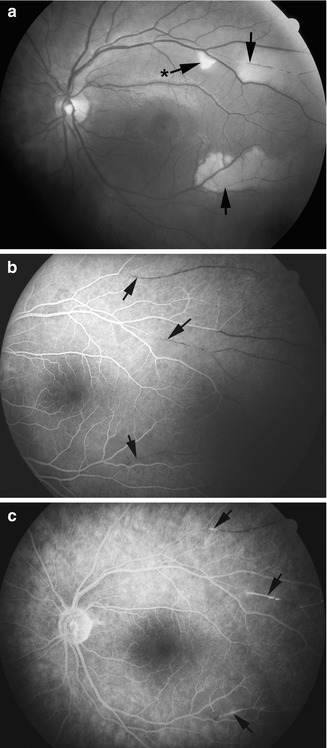
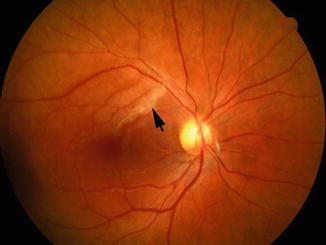
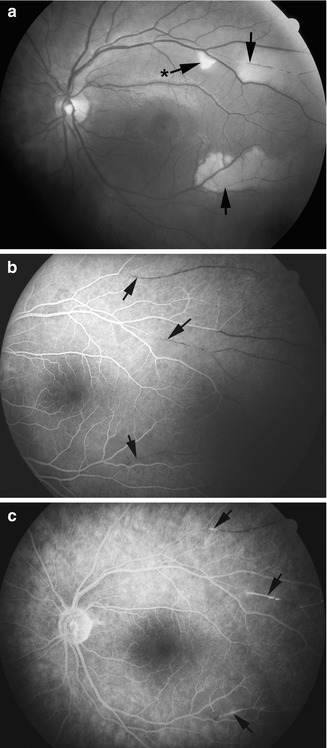
Fig. 15.2
The left eye on July 17, 1989. (a) Fundus photograph shows various sites of retinal arteriolar occlusion (arrows), and one cotton-wool spot (arrow with asterisk). (b) Fluorescein fundus angiogram, during the late retinal venous phase, shows non-filling of the various occluded retinal arterioles (arrows) (Reproduced from Hayreh SS and Zimmerman MB [144]). (c) Fluorescein fundus angiogram, during the late phase, shows staining of the walls of the involved arteriole (arrows)
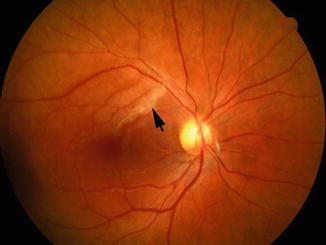
Fig. 15.3
Fundus photograph of the right eye on July 17, 1989, shows resolving infarct
After delivery, the patient’s mental status, dysarthria, and ataxia gradually improved, although she remained amnestic for many of the events of the past month. She was discharged taking warfarin on July 25. Ultrafast (cine) CT scan of the heart done as an outpatient was normal. Six weeks after her discharge, her examination was remarkable only for persistent visual field deficits in both eyes; her mental status, speech, coordination, and gait were normal. She took warfarin for 8 months without further episodes. She then took 325 mg aspirin per day, and 11 months after the onset of initial problem, a hypercoagulability profile including partial thromboplastin time; thrombin time; fibrinogen, antithrombin III, protein C, protein S, and plasminogen concentrations; platelet count; and platelet aggregation studies was normal.
In summary, the clinical features of this syndrome affecting arteriolar vascular distributions may be categorized within the triad of encephalopathy, retinopathy, and hearing loss. This patient had all the typical clinical features of this syndrome. She is a woman within the age range, of 18–40 years. She had an encephalopathy manifested by personality change, dementia, ataxia, long-tract signs, and dysarthria. She had multifocal branch retinal arteriolar occlusions with associated retinal infarcts and scotomas. She had bilateral sensorineural hearing loss detected by audiometry. She had a marked elevation of the CSF protein concentration without a marked pleocytosis. Her MRI showed multifocal areas of increased signal intensity in the cerebral white matter on T2-weighted images. Her cerebral arteriogram was normal. Her EEG showed diffuse slowing. She had a moderately elevated ESR, but there was no other evidence for vasculitis. This patient was shown to have a patent foramen ovale, but all the clinical findings fit Susac’s syndrome.
Second Patient
A 42-year-old female physician was seen in my clinic from July 27, 1992, to September 1998. She developed multiple episodes of BRAO, in one or the other or both eyes from time to time, from August 1991 till September 1994. Figures 15.4, 15.5, 15.6, 15.7, and 15.8 show fundus photographic and fluorescein fundus angiographic findings in July 1992 (Fig. 15.4a, b), September 1992 (Figs. 15.5a, b and 15.6a–c), November 1993 (Fig. 15.7a, b), and September 1994 (Fig. 15.8), involving one or the other eye. During these episodes, on many occasions, the vitreous showed some cells in the involved eye. The eyes progressively developed multiple scotomas and peripheral visual field defects, sparing central fixation so that the visual acuity was 20/15 in both eyes all along (Figs. 15.9 and 15.10). I treated her with corticosteroids from September 1992, starting with a high dose and then tapering it down, but whenever the dose was small, there was a recurrence, and each time she had to start all over again with a high dose. She was on corticosteroids till July 1995, with no recurrence after that. Thus, this lady had recurrent episodes of BRAO in both eyes for about 3 years, and it seems corticosteroids helped each time a new episode developed.
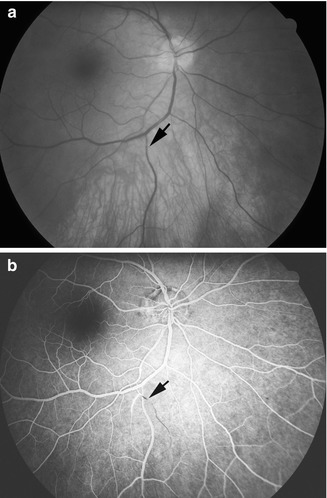
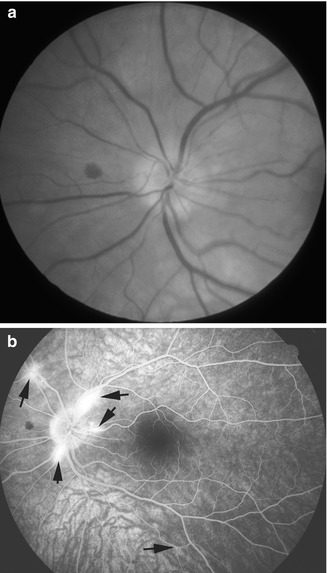
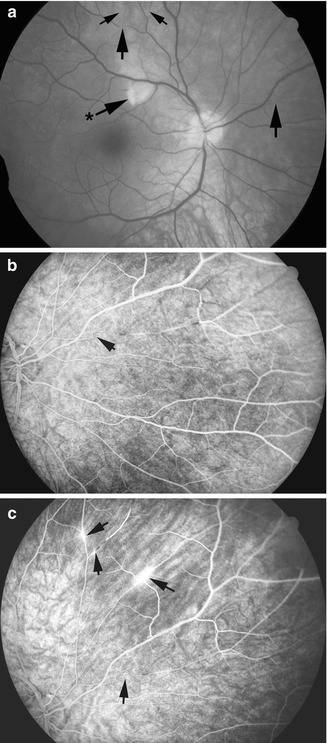
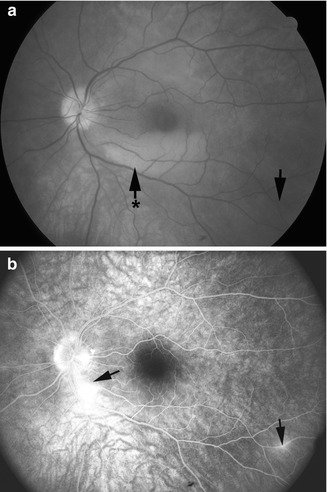
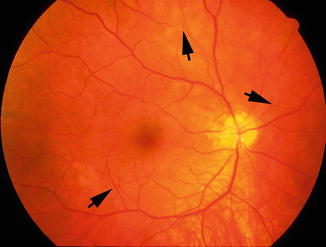
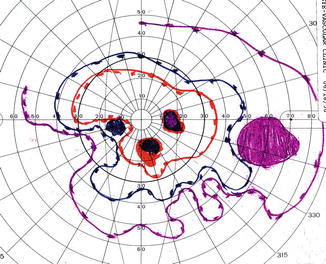
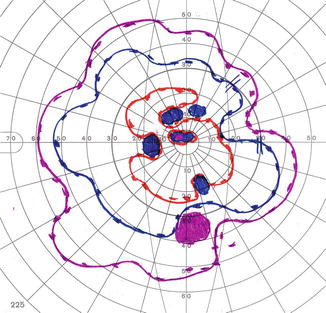
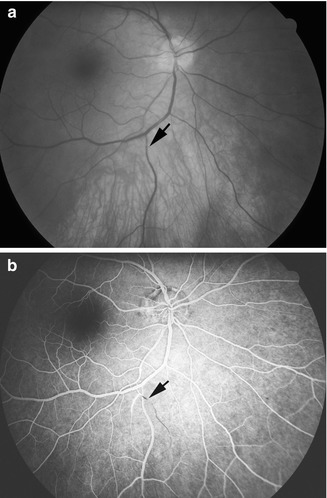
Fig. 15.4
The right eye on July 27, 1992. (a) Fundus photograph shows small BRAO (arrow). (b) Fluorescein fundus angiogram, during the late retinal venous phase, shows non-filling of the occluded branch retinal arteriole (arrow)
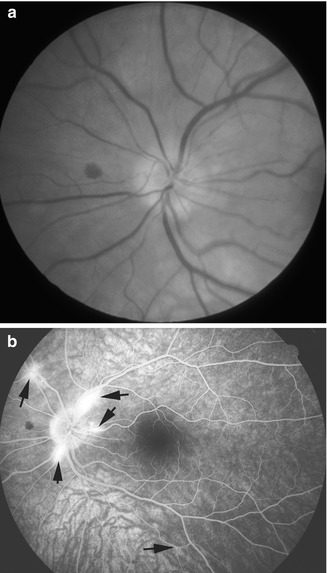
Fig. 15.5
The left eye on September 2, 1992. (a) Fundus photograph shows a small hemorrhage nasal to the optic disc. (b) Fluorescein fundus angiogram, during the late phase, shows fluorescein leakage (arrows) from the involved arterioles, which was not clearly evident in fundus photograph in 5 (a)
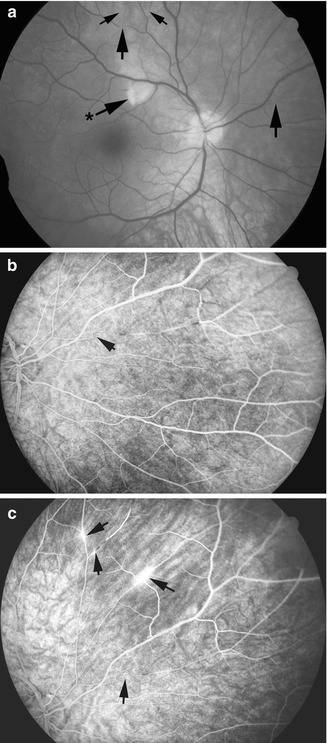
Fig. 15.6
The right eye on September 2, 1992. (a) Fundus photograph shows a small cotton-wool spot (arrow with asterisk) and multiple sites of BRAO (arrows). (b) Fluorescein fundus angiogram, during the late retinal venous phase, shows BRAO (arrow). (c) Fluorescein fundus angiogram, during the late phase, shows fluorescein leakage from the involved arterioles (arrows)
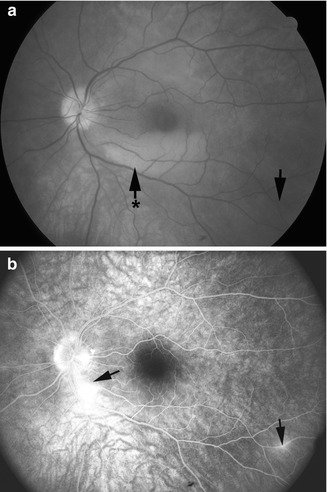
Fig. 15.7
The left eye on November 1, 1993. (a) Fundus photograph shows an area of retinal infarct (arrow with asterisk) and another BRAO (arrow). (b) Fluorescein fundus angiogram, during the late phase, shows fluorescein leakage from the involved arterioles (arrows)
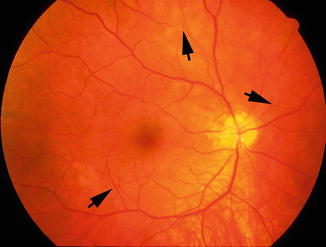
Fig. 15.8
The right eye on September 15, 1994. Fundus photograph shows various sites of BRAO (arrows)
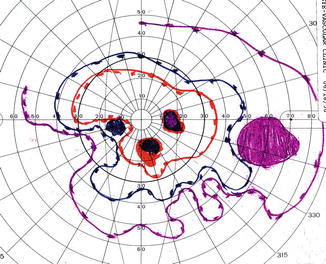
Fig. 15.9
The right eye in September 1998. Visual field plotted with a Goldmann perimeter shows multiple scotomas and peripheral visual field defect
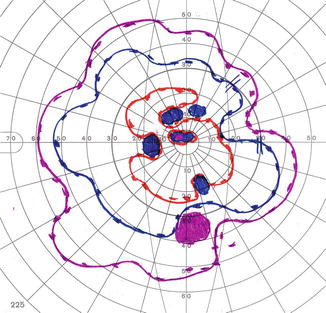
Fig. 15.10
The left eye in September 1998. Visual field plotted with a Goldmann perimeter shows multiple scotomas and peripheral visual field defect
She had a history of hearing loss in the right ear, paresthesia of upper extremities, and migraine since the spring of 1990. On November 17, 1992, at supper time, she developed mental confusion, speech problems, and balance difficulty, with ringing in the ears and hearing problem; her mental and hearing problems, although better when seen on January 13, 1993, were not back to normal. She was fully investigated by the neurology department by various hematological evaluations, including ANA, erythrocyte sedimentation rate, and C-reactive protein evaluations and MRI, cerebral angiography, CSF examination, and other evaluations; none showed any abnormality, except that she had peripheral neuropathy.
Fluorescein fundus angiography in both the above cases with Susac’s syndrome shows that it provides much more useful information about the various BRAO than ophthalmoscopy, and also it shows evidence of vasculitis by the presence of fluorescein staining or leakage.
Conditions Associated with BRAO
There is a voluminous literature describing systemic conditions associated with BRAO; but most of these are based on anecdotal case reports. It is possible that in some situations, there may not be any cause-and-effect relationship. The following is a summary of the conditions described in the literature.
Hyperlipidemia and Atherosclerosis
Hyperlipidemia causes atherosclerosis. Atherosclerosis is the most common cause of cardiovascular disease. This is discussed at length in Chap. 13 dealing with central retinal artery occlusion.
Carotid Artery Disease
The association of carotid artery disease with BRAO is well known. Embolism is the most common cause of BRAO. Atherosclerotic lesions of the common and/or internal carotid artery are well-established causes of BRAO. There are many reports of the association of BRAO with carotid artery disease in the literature.
Cardiac Causes
Diabetes Mellitus and Arterial Hypertension
Following Invasive Cardiovascular Procedures
Vasculitis and Chronic Systemic Autoimmune Diseases
There are anecdotal case reports of the association of BRAO with a variety of vasculitides, including the following: toxoplasmic chorioretinitis [41–47], cytomegalovirus retinitis [48–51], acute multifocal inner retinitis [52], idiopathic retinal vasculitis [47], Behçet’s disease [48, 53, 54], cat-scratch disease [47, 55–57], Takayasu’s arteritis [58–60], aortoarteritis [61], vaccination [62, 63], varicella zoster virus [64], Crohn’s disease [47, 65], Churg-Strauss syndrome [66], lupus [67], rheumatoid arthritis [68], rickettsia infection [47, 69], West Nile virus [47], dengue fever [70], Lyme disease [71], ocular tuberculosis [47], pseudotumor cerebri [72], and candida endophthalmitis [73]. Fineman et al. [74] reported BRAO in giant cell arteritis, but that is in fact cilioretinal artery occlusion due to occlusion of the posterior ciliary artery by giant cell arteritis and not true BRAO because, as mentioned above, the so-called branch retinal arteries are in fact arterioles and giant cell arteritis does not involve arterioles.
Thrombophilia
There are several reports suggesting that thrombophilia plays a role in the development of BRAO. The various thrombophilic factors reported include antiphospholipid syndrome [75–78], factor V Leiden mutation and antiphospholipid antibody syndrome [77], protein C deficiency [5], protein S deficiency [79], hyperhomocysteinemia [80], and methylenetetrahydrofolate reductase [81].
Malignant Diseases
Perioperative BRAO
There are reports of development of BRAO following non-ocular surgery, due to embolism from other regions, such as coronary angiography [84, 85], after carotid artery surgery [86], thyroid artery interventional embolization [87], embolization of arteriovenous malformation [88, 89], embolization of an intracranial meningioma [90], embolization of a maxillary sinus tumor [91], cosmetic facial filler injections [92] and septoplasty [93], and operative complications of optic nerve sheath decompression [94].
Following Facial or Retrobulbar Injections
Development of BRAO has been reported following intranasal anesthetic injection [95].
Following Intravitreal Injection of Anti-vascular Endothelial Growth Factor (VEGF) Therapy
Intravitreal injection of anti-VEGF drugs is commonly used for macular edema due to various causes, for neovascular age-related macular degeneration, and for ocular neovascularization. One report mentions development of BRAO following this injection for ischemic central retinal vein occlusion [96].
Miscellaneous Causes
Several reports based on one or a few cases of BRAO have noted it in association with some other conditions. These include pregnancy [97, 98], migraine [10, 99, 100], prepapillary arterial loop [101, 102], photocoagulation of a peripapillary choroidal neovascular membrane [103] and of an arterial macroaneurysm [104], diathermy of a persistent hyaloid artery [105], removal of an intraocular foreign body from the optic nerve head [106], with interferon [107], with high-dose carmustine and cisplatin therapy [108], epipapillary isolated astrocytoma [109], hereditary hemorrhagic telangiectasia [110], rupture of retinal arteriolar macroaneurysm on the optic disc [111], and Gaucher disease [112].
The above list of causes for BRAO covers all age groups. I further analyzed the causes according to age groups into the following two groups: (1) CRAO in children (the United Nations Convention on the Rights of the Child defines a child as “a human being below the age of 18 years”) and (2) young persons, defined as aged between 18 and 44 years.
BRAO in Children
In this age group, BRAO associated with a variety of conditions has been reported in several anecdotal cases or based on a few cases. These include carotid artery disease [113, 114], toxoplasmosis [46], cytomegalovirus infection [48], acute multifocal inner retinitis [52], cat-scratch disease [55, 57], Takayasu’s arteritis [59], Rickettsia conorii infection [69], pseudotumor cerebri [72], primary antiphospholipid syndrome [76], astrocytoma [109], increased factor VIII activity [115], ocular trauma [115], and unknown etiology [116, 117].
The underlying mechanisms of the development of BRAO associated with the above conditions in children are considered in the discussion dealing with occlusion of CRAO (see Chap. 13).
BRAO in Young Persons
Several reports of one or a few cases have described BRAO associated with a variety of conditions in this age group. These include carotid artery disease [113, 118, 119], cardiac causes [29–32, 35–37], toxoplasmic chorioretinitis [41, 44], cytomegalovirus retinitis [49, 51], acute multifocal inner retinitis [52], Behçet disease [53, 54], cat-scratch disease [55–57], Takayasu’s arteritis [60], vaccination [62], Crohn’s disease [54, 65], lupus [67], rickettsia infection [54, 69], West Nile virus [54], Lyme disease [71], dengue fever [70], antiphospholipid syndrome [78], protein C deficiency [5], protein S deficiency [79], hyperhomocysteinemia [80], methylenetetrahydrofolate reductase [81], after thyroid artery interventional embolization [87], embolization of arteriovenous malformation [89], following embolization of an intracranial meningioma [90], cosmetic facial filler injections [92], after septoplasty [93], following intranasal anesthetic injection [95], following intravitreal anti-VEGF therapy [96], by diathermy of a persistent hyaloid artery [105], pregnancy [97, 98, 115], migraine [11, 99, 100, 115], removal of an intraocular foreign body [106], Gaucher disease [112], hereditary hemorrhagic telangiectasia [110], increased factor VIII activity [115], use of birth control pills [115], drug abuse [115], and unknown cause [115].
Most of the association of BRAO with the systemic conditions described above is based on reports of a single or only a few cases. In most other studies, the findings of BRAO are combined with those of CRAO, so that it is not possible to get accurate information about BRAO alone. The following are some studies based on larger series which provide information specifically on BRAO.
Karjalainen [120] in 1971, in a retrospective review of 39 BRAO patients, found associated arterial hypertension in 4, diabetes mellitus in 4, “arteriosclerosis” in 9, congestive heart failure in 1, myocardial infarction in 6, mitral insufficiency in 1, arterial hypotension in 1, ipsilateral internal carotid artery occlusion or stenosis in 4, hypercholesterolemia in 1, thyrotoxicosis in 1, and hypernephroma in 1.
Schmidt et al. [33] in 2007 reported their findings in 134 patients with BRAO. They found cardiovascular risk factors in 51 %. These were arterial hypertension in 74 % of them, diabetes mellitus in 13 %, hyperlipidemia in 29 %, and chronic smoking in 32 %. Doppler sonography revealed internal carotid artery disease in 65 % (≥70 % stenosis in 21 %, plaques in 29 %). Echocardiography showed disorders of cardiac rhythm (for instance, chronic atrial fibrillation) in 7 %, aortic valve disease in 31 %, mitral valve disease in 14 %, both aortic and mitral valve disease in 3 %, and patent foramen ovale in 9 %. There was history of stroke in 7 %, transient ischemic attack in 4 %, simultaneous stroke or transient ischemic attack with retinal arterial occlusion in 0.7 %, and amaurosis fugax in 13 %.
In 2009, I [3] reported my findings of associated systemic abnormalities in 190 patients with in BRAO. There was diabetes mellitus in 13 %, renal disease in 4 %, arterial hypertension in 54 %, ischemic heart disease in 26 %, stroke/transient ischemic attack in 17 %, hyperlipidemia (males 22 % and females 30 %), and current smokers (males 32 % and females 38 %). Carotid Doppler/angiography and echocardiography findings are summarized in Table 15.1. They show that the most common abnormality and source of embolism in the carotid arteries is the presence of plaque(s) (66 %); significant carotid stenosis (i.e., ≥50 %) was seen in only 31 %. Echocardiography findings in this study showed 42 % with abnormal echocardiogram of an embolic source. Of those with an embolic source, 31 % were from the mitral valve, 28 % from the aortic valve, and 41 % from both. The mitral valve lesions comprised 70 % calcified valve, 4 % mitral valve prolapse, and 26 % other types of lesions. The aortic valve lesions were 68 % calcified valve and 32 % of other types. Patent foramen ovale was detected in 2 %. The finding of an abnormal echocardiogram with an embolic source was not significantly associated with stroke/transient ischemic attack (p = 0.18) or ischemic heart disease (p = 0.69). Relating Doppler/angiography findings to echocardiography findings showed an abnormal echocardiogram with an embolic source in 44 % of those with plaque and 29 % of those without plaque (p = 0.46). This means that when a patient has abnormalities in both Doppler/angiography and echocardiography, the embolus could have come from either the carotid artery or the heart or possibly both. This indicates that one has to evaluate both sources for embolism in all patients with BRAO.
Table 15.1
Carotid Doppler/angiography and echocardiography findings on the side of the involved eye
Test finding | BRAOa |
|---|---|
Patent foramen ovale | (n = 141) |
3 (2 %) | |
Carotid Doppler/angiography: | (n = 128) |
Occlusion | |
0–15 % | 69 (54 %) |
16–49 % | 21 (16 %) |
50–79 % | 21 (16 %) |
80–99 % | 11 (9 %) |
100 % | 6 (5 %) |
Carotid Doppler/angiography: | (n = 123) |
Plaque present | 81 (66 %) |
Echocardiogram | (n = 76) |
Normal | 32 (42 %) |
Abnormal, no embolic source | 12 (16 %) |
Abnormal, with embolic source | 32 (42 %) |
Echocardiogram: | (Of n = 32 with embolic source) |
Abnormal embolic source | |
Mitral valve | 10 (31 %) |
Aortic valve | 9 (28 %) |
Mitral and aortic valves | 13 (41 %) |
Echocardiogram: | (Of n = 23 with mitral valve as embolic source) |
Mitral valve lesion types | |
Calcified valve | 16 (70 %) |
Mitral valve prolapse | 1 (4 %) |
Other types of lesions | 6 (26 %) |
Echocardiogram: | (Of n = 22 with aortic valve as embolic source) |
Aortic valve lesion types | |
Calcified valve | 15 (68 %) |
Other types of lesions | 7 (32 %) |
In my study [3], the prevalence of diabetes mellitus, arterial hypertension, ischemic heart disease, and stroke/transient ischemic attack in BRAO was significantly higher compared to the prevalence of these conditions in the matched US population (all p ≤ 0.009). Smoking prevalence in BRAO compared to the US population was significantly higher for the female patients (p = 0.025).
Therefore, in conclusion, my study [3] showed that the carotid artery and the heart are the most common causes of BRAO by producing emboli, and emboli are the most common cause of BRAO. Retinal emboli are usually of three types: calcific, cholesterol, and platelet-fibrin [121]. Figure 15.11 shows various locations and types of emboli seen in my studies on BRAO. In the carotid artery, plaque is the most common source of that. In the heart, as discussed above, sources of emboli are aortic and mitral valvular lesions, patent foramen ovale, myxoma in the left atrium, and atrial fibrillation.
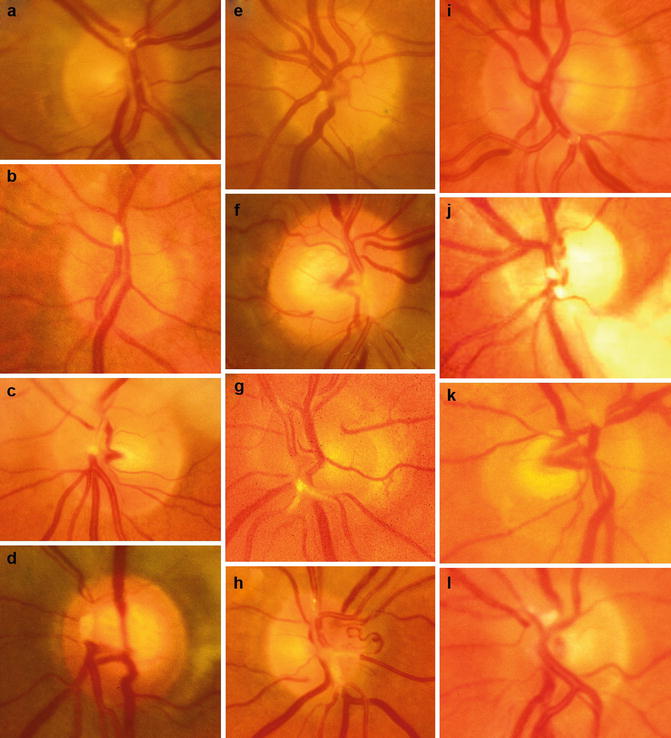
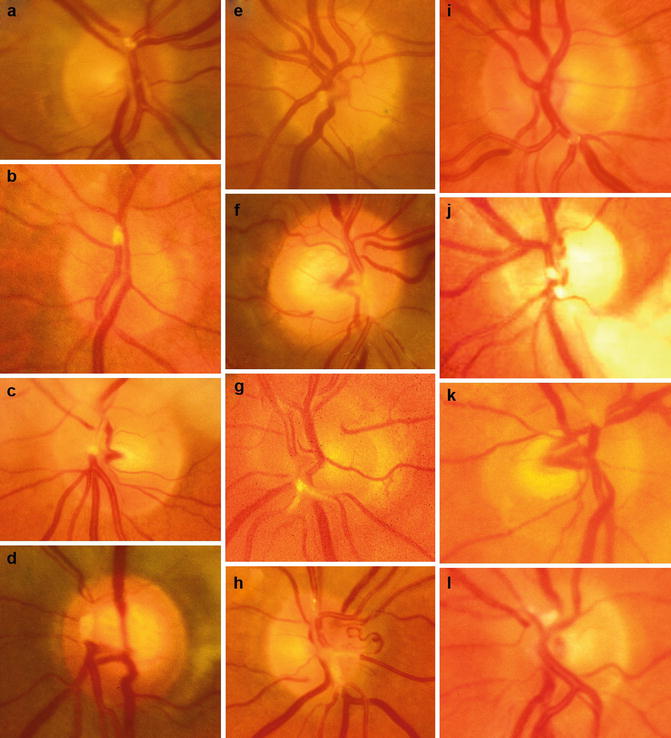
Fig. 15.11
Fundus photographs of BRAO eyes show emboli of different types in different locations. (a–d) Emboli occluding the superior division of the central retinal artery. (e–h) Emboli occluding the inferior division of the central retinal artery. (i, j) Emboli occluding the inferior temporal retinal arterioles. (k, l) Emboli occluding the superior temporal retinal arterioles. (f–h) Platelet emboli. (i) A cholesterol embolus. The rest are most probably calcific emboli
There is interest in finding out about the relationship between the retinal emboli and development of stroke. Klein et al. [122, 123] in their Beaver Dam Eye Studies of 4,926 persons 43–86 years old determined the relationship of retinal emboli to the risk of stroke and ischemic heart disease mortality at 5-year [122] and 10-year incidence [123]. In their 5-year study [122], they found the prevalence of retinal arteriolar emboli was 0.9 %. They found that after adjustments for age and sex, the prevalence of retinal emboli was associated with higher pulse pressure, arterial hypertension, diabetes mellitus, past and current smoking, and cardiovascular disease. After age, sex, and systemic factors were controlled for, people with retinal emboli had a significantly higher hazard of dying of stroke than those without retinal emboli. In their 10-year study [123], the cumulative incidence of retinal emboli was 1.5 %. After adjustment for age and sex, the incidence of retinal emboli was associated with increased pulse pressure (p = 0.03), higher serum total cholesterol level (p = 0.03), higher white blood cell count (p = 0.05), smoking status (p < 0.001), and a history of coronary artery bypass surgery (p < 0.001) at baseline. After controlling for age, sex, and systemic factors, people with retinal emboli had a significantly higher hazard of dying from stroke than those without.
In contrast to that, the finding of my study [3] showed that an abnormal echocardiogram with an embolic source was not significantly associated with stroke/transient ischemic attack (p = 0.18) or ischemic heart disease (p = 0.69).
It is essential to put into proper perspective, how reliable the incidence of retinal emboli in a study is. My study on fundus changes in CRAO [124] showed that migration and disappearance of retinal emboli is a common finding. This topic is discussed in Chap. 13. The phenomenon of migratory emboli places considerable limitations on determining the prevalence of retinal arteriolar emboli and their relationship with stroke or other systemic conditions.
Investigations in Patients with BRAO
From the above discussion, it is evident that patients with BRAO should have the following investigations to find out the cause and to prevent or reduce the risk of any further visual problems or stroke.
1.
Since embolism is the most common cause of BRAO, all patients with BRAO or emboli in the retinal arterioles must have a complete evaluation to find the source of emboli. As discussed above, the most common sources of emboli are the carotid artery and the heart. In the carotid artery, the most common source of embolus is a plaque, so that it is essential to find out if there are any plaques; unfortunately, I have found that most of the time evaluation is primarily focused on whether there is hemodynamically significant carotid artery stenosis, without any attention being paid to the presence of plaques. The actual source of emboli can be missed. A large study showed that asymptomatic Hollenhorst plaques are an important marker of carotid occlusive disease and affected patients should undergo a carotid evaluation similar to those with symptomatic plaques [146].
2.
Cardiac evaluation is equally essential, even if the carotid artery shows lesions, because I have found that at times a patient can have lesions in both places and either of them can be the source of emboli. As discussed above, my study showed that the most common source of emboli in the heart is the valves, although other lesions can also be a cause (Table 15.1). Transesophageal echocardiography is the best way to evaluate heart lesions.
3.
Atherosclerosis is a common cause of lesions in the carotid artery, so that it is essential to do lipid evaluation. I have found that physicians invariably tend to look only at the total cholesterol level. But I have seen many patients with perfectly normal total cholesterol level but with high low-density lipoprotein (LDL), which is the most important parameter to look for. The current guideline is to have LDL not more than 70s mg/dl. Similarly, triglycerides should also be within in normal limits.
4.
Since arterial hypertension and diabetes mellitus are significantly more prevalent in these cases, their evaluation and management is essential.
5.
As discussed above, there are many rare causes of BRAO. In difficult cases, one has to keep those in mind. In my studies, I have not found that doing thrombophilia evaluation is particularly fruitful in BRAO.
Racial Differences in the Causes of Retinal Arterial Occlusion
Ahuja et al. [125], in a retrospective study of consecutive 29 African American and 17 Caucasian patients with a diagnosis of amaurosis fugax, central retinal artery occlusion, BRAO, or intra-arterial retinal plaques, evaluated the causes of retinal artery occlusion. They found that their African American patients had a mean age of 61 years (range, 30–77 years) and the Caucasian patients a mean age of 73 years (range, 56–94 years) (p = 0.003). There was no statistically significant difference between the two groups with respect to visible emboli on ophthalmoscopy, or with regard to risk factors for arterial occlusive disease such as arterial hypertension, coronary artery disease, hypercholesterolemia, tobacco use, and history of stroke or transient ischemic attacks. But Caucasian patients had a 41 % incidence of high-grade ipsilateral internal carotid artery stenosis, compared with a 3.4 % incidence in African American patients (p = 0.002).
Cheung et al. [126] found that the prevalence of retinal emboli was lower in Asian Malaysians than in similarly aged White persons, but associated with similar cardiovascular risk factors.
Demographic Characteristics of BRAO
Karjalainen [120] in 1971, in a retrospective review of 58 BRAO patients, reported the average age at the time of onset 62.0 ± 9.9 years (41–84 years), with 50 % of the patients over 60. There were 35 men and 23 women. Among 40 eyes, involvement of branches was as follows: superior temporal in 17, inferior temporal in 11, macular in 5, superior nasal in 2, inferior half in 2, superior half in 1, temporal half in 1, and nasal half in 1.
Schmidt et al. [33] in 2007 reported their findings in 134 patients with BRAO. There were 68 % males, and median age 65 (range 22–90) years.
In 2009, my study [2] showed the following: In permanent BRAO, there were 122 patients (47 female, 75 male) with BRAO; 11 of them had bilateral involvement. The mean age at first onset was 61 ± 14(SD) years, with a range of 13–83 years. Table 15.2 lists the various types of permanent BRAO. The two most common types were superior temporal BRAO (31 %) and inferior temporal BRAO (28 %), and less common were those involving the entire superior (11 %) or inferior (8 %) halves, those involving only the macular region (10 %), combined superior and inferior temporal (5 %), and other miscellaneous combinations in the rest.
Table 15.2
Types of permanent branch retinal artery occlusion (BRAO)
BRAO type | Count (%) |
|---|---|
n = 133 eyes | |
Superior (involving superior half of the retina) | 14 (11 %) |
Superior temporal | 41 (31 %) |
Superior temporal + inferior nasal | 1 (1 %) |
Superior macular
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|