Blepharitis and Inflammation of the Eyelids
Naushad Hussein
Ivan R. Schwab
Inflammation of the eyelids, or blepharitis, is the most frequently encountered ocular disease. Based on its anatomic location (i.e., anterior or posterior lamella), the disease process can be divided into two basic categories: anterior lamella lid disease and posterior lamella lid disease.
The anterior lamella is delimited by the skin on the anterior surface and the gray line or Marx line posteriorly. The anterior lamella is usually affected by staphylococcal species and/or seborrhea, which can lead to ocular surface disease. Posterior lamellar lid disease, or posterior marginal blepharitis, is a condition of the eyelid margin characterized by meibomian gland dysfunction (MGD), which may lead to ocular surface disease as well. Both forms of blepharitis may be inflammatory, noninflammatory, or even infectious in nature. The majority of cases are associated with hyperemia and thickening of the lid margin.
EPIDEMIOLOGY
Inflammation of the eyelid is a very common disorder and can be broadly categorized into two forms. Both forms occur more frequently in elderly patients, and both are underdiagnosed. Anterior lamellar lid disease is perhaps more frequently associated with skin diseases such as seborrhea, rosacea, and atopy. Posterior lamellar lid disease usually consists of MGD and is associated with sebaceous gland disorders, especially rosacea. Dry eye syndrome is often associated with both anterior and posterior lamellar lid disease and both can contribute to its severity. Symptoms of coexisting ocular surface disease and allergy can be aggravated by inflammatory lid disease. Exogenous irritants and allergens, although often not causative, may exacerbate both forms of blepharitis. The uncertain cause, chronicity of associated conditions, and inadequate treatments make this disease difficult to manage.
SEBORRHEIC (SQUAMOUS) BLEPHARITIS
Seborrhea is a troublesome condition, and it is the most common cause of anterior lamellar or marginal blepharitis. It usually involves the scalp and face. The skin may be excessively oily. Mild cases often are not recognized because of the lack of symptoms. Severe seborrhea can cause photophobia and a feeling of heaviness of the eyelids.
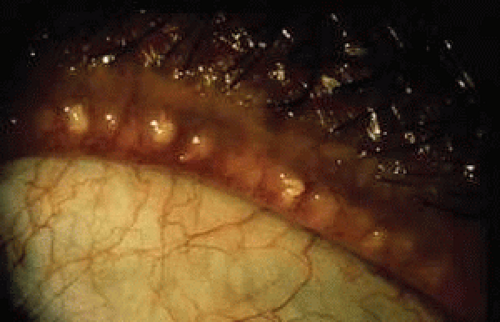
Significant findings include lid-margin inflammation, dry flakes (dandruff or scurf) or oily secretion on the eyelashes and lid margins, and concomitant dandruff of the scalp, eyebrows, and external ears (also called scurf) (Fig. 1). A mild, fine, medium, or blotchy epithelial keratitis can also occur. Seborrhea is frequently accompanied by Staphylococcus aureus infections (see later discussion on mixed blepharitis).
Controversy exists as to the role played by Pityrosporum ovale and Pityrosporum orbiculare in the cause of seborrhea. These budding yeasts are plentiful in scrapings from seborrhea; in AIDS patients with severe seborrheic dermatitis, 2% ketoconazole cream significantly decreases the number of organisms and greatly improves the condition.1 This treatment may be effective in others groups of patients without AIDS but has not been systematically investigated.
Mild forms of seborrhea require only control of the scalp seborrhea with over-the-counter antiseborrheic shampoos, such as Head and Shoulders, Selsun Blue, or Exsel.
In patients with severe seborrheic blepharitis, do the following:
Culture the lid margins to rule out superimposed S. aureus infections, and institute vigorous antiseborrheic lid-margin treatment.
Instruct the patient to remove the seborrheic flakes and oil at least once daily by vigorous scrubbing of the lid margin with a mild soap (e.g., Johnson’s No Tears Shampoo, Dove soap, or Almay Nonoily Eye Makeup Remover) or the commercially available range of lid care towelettes. Gentle lid cleansing cannot be overemphasized in its effectiveness in most patients.
If S. aureus is present, treat the patient with a suitable antibiotic as well (see later discussion).
MEIBOMIAN GLAND DYSFUNCTION
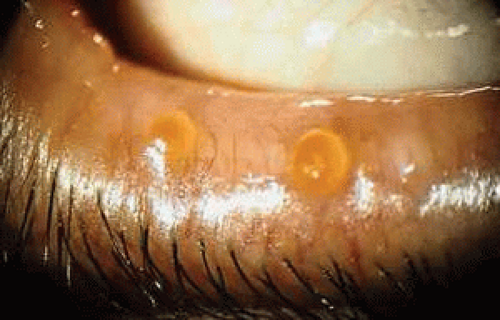
A common and underrecognized cause of lid inflammation is MGD, which usually causes posterior lamella lid disease. Meibomian glands are enlarged sebaceous glands aligned in a row posterior to the eye lashes. They produce a clear, holocrine lipid secretion that makes up the outer layer of the preocular tear film. Inflammation, infection, and obstruction of these glands results in hyperkeratinization of ductal epithelium, atrophy of acinar cells, abnormal gland secretion, altered tear film physiology, and ocular surface irritation (Figs. 2,3,4). Certain persons may be predisposed to this condition, or hormones may play a role in creating an environment that encourages lipase-producing bacteria that alter glandular secretion.2 Research suggests lipase or esterase activity could result in the release of linoleic acid from meibum that could induce differentiation of meibomium gland duct keratinocytes, producing reactive oxygen species. This complex cascade of activity could be important in the development of signs associated with lid inflammation.
With increasing age, meibomian gland disease becomes a more common presentation in patients. Most patients have nonspecific complaints inconsistent with the degree of disease clinically evident on examination. Lid margins have focal or diffuse inflammation, with telangiectasia around the meibomian gland orifices. The orifices are pouting, obstructed, displaced, or reduced in number. Digital pressure on the lid margins reveals hyposecreting or hypersecreting glands with a foamy, turbid, granular, or pasty discharge. Chalazia, papillary conjunctival inflammation, and punctate staining of the ocular surface especially along the lid margin in the lower one fifth of the cornea could also be present, with abnormal tear break-up time indicative of an unstable tear lipid layer that explains the frequently associated evaporative dry eyes. Clinical presentation may be compounded with associated staphylococcal lid infection, seborrhea, and acne rosacea.3,4,5
Management of this chronic condition consists of patient education and lid hygiene with warm compresses and expression of glands every day to alleviate symptoms. In severe cases, patients should take oral tetracycline (250 mg by mouth four times daily), doxycycline (50 mg by mouth twice daily), or minocycline (50 mg by mouth twice daily) for weeks to months. Higher dosages may result in a higher rate of complications. These doses may often be adjusted downward but still control the signs and symptoms, and doses of half, or less, of these initial starting doses can be sufficient. These medications decrease production of bacterial lipases and thus decrease fatty acid levels.6 Their use is contraindicated in children and in pregnant or lactating women, and probably in the elderly with moderate renal failure. Tetracycline and related drugs can cause photosensitization, gastrointestinal upset, vaginitis, and, rarely, azotemia. They have been implicated in cases of pseudotumor cerebri and they also may decrease effectiveness of oral contraceptives and potentiate the effect of warfarin. Keratolytics, such as weak silver nitrate (1% or less) will help remove the keratinized plugs along the lid margin. Associated lid bacterial infections, seborrhea, acne rosacea, and keratoconjunctivitis sicca should be diagnosed and treated appropriately (see later discussion).
BACTERIAL LID INFECTIONS
Bacterial infections of the lid margins, especially staphylococcal infections, are common.
Staphylococcal Lid Infections
Staphylococcal blepharitis is not self-limited and is difficult to eradicate successfully.7 It is a common cause of chronic conjunctivitis, recurrent epithelial keratitis, and recurrent morbidity.8 The patient is frequently beset with symptoms of photophobia, pain, tearing, redness, blurred vision, and discharge.
The infection is characterized by one or more of the following features2:
Ulcerations at the base of the eyelashes: The ulceration is preceded by a folliculitis of the pilosebaceous unit. Fibrin, which exudes from the base of the ulcer, usually masks the presence of the ulcer.
Collarettes: Collarettes are small, thin, fibrinous scales that surround the eyelash like a small piece of paper impaled on a stick. The collarette is formed by the fibrin that covers the base of the ulcer. It usually surrounds the eyelash and may be carried away from the surface of the skin as the lash grows (Fig. 5). This is virtually pathognomonic for microbial lid involvement, especially staphylococcal infections.
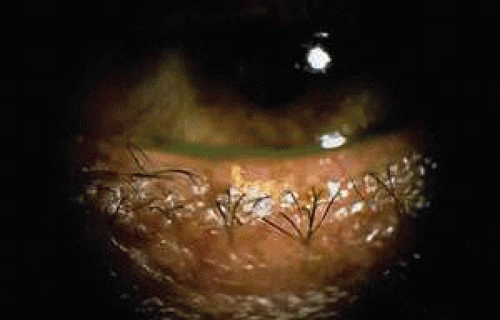
Fig. 5. Anterior lamella lid disease due to staphylococcal infection. Note collarette in the center of the photograph.
Localized poliosis or canities (whitening) of individual eyelashes: Poliosis occurs from staphylococcal damage to the pilosebaceous unit (Fig. 6).
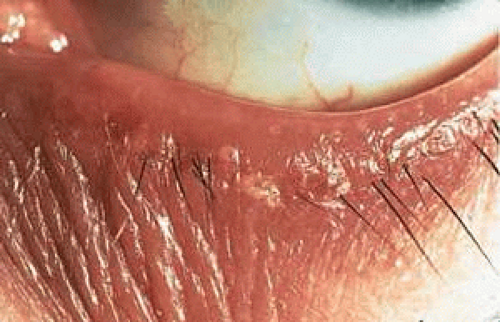
Fig. 6. Anterior lamella lid disease with acute folliculitis, lash misdirection, lash loss, erythema, and tylosis.
Short, misdirected, broken, sparse, or missing eyelashes: The hair follicles are often damaged by the staphylococcal infection. Lashes produced in damaged hair follicles are often short, misdirected, and broken. Large areas where eyelashes are absent are commonly found.
External hordeolum (style): An external hordeolum represents an abscess of a gland of Zeis. Pain, redness, and swelling occur. The pain is proportional to the degree of swelling. The abscess points to the skin at the lid margin.
Internal hordeolum: An internal hordeolum is often caused by a staphylococcal infection. The infection occurs within the meibomian gland and often produces intense pain and swelling. The lesion may eventually drain through the skin or conjunctiva.
Multiple, recurrent chalazia: A chalazion is a sterile, zonal granulomatous reaction of the meibomian gland. Multiple or recurrent chalazia are often caused by staphylococcal infections of the meibomian glands but may also represent sterile inspissation of the orifice leading to a lipogranulomatous inflammatory response to accumulating meibomian secretions. The staphylococcal infections cause inflammation and edema of the neck of the gland, with resulting inspissation of the meibomian gland and, eventually, chalazion formation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree