PREOPERATIVE ASSESSMENT AND EVALUATION
Frequently overlooked by surgeons, the preoperative assessment is one of the most important components to planning a successful operation. The preoperative evaluation begins in the office with a detailed history and physical. All medications, including herbal supplements and dosages, must be recorded. It is also prudent to discuss illicit drug use, alcohol consumption, and tobacco use with the patient as these social habits can affect anesthesia and post-operative outcomes. Functional capacity can be assessed with questions about activities of daily living. Patients who can climb one flight of stairs or walk several blocks expend four or more metabolic equivalents (METs) and typically require no further cardiac workup (
Table 2.1) (
1). However, patients who can do little more than dress themselves will need further cardiac assessment prior to surgery (
2). Based on the information gathered at this initial visit, the patient’s overall health status can be judged and further assessment completed as necessary.
The goal of preoperative assessment is to identify patients who are at risk of perioperative complications and work to limit their risk prior to surgery. The most important component is the cardiac assessment. The American College of Cardiology (ACC) and American Heart Association (AHA) created a task force in 1997 to develop perioperative guidelines to better direct the preoperative workup. These guidelines were updated in 2007 and provide tools to evaluate cardiac status prior to noncardiac surgery (
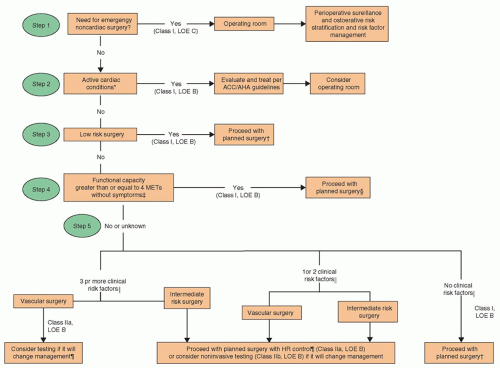
1). The guidelines are summarized in algorithm format (
Fig. 2.1) (
1). The primary decisions are limited to two essential questions—should the patient undergo additional cardiac evaluation prior to surgery, and is a perioperative beta-blocker indicated to reduce the risk of cardiac complications?
While the algorithm appears complex at first glance, it is actually a very simple tool to quickly answer these questions. The first step is to identify the urgency of the procedure, as emergent or more urgent procedures cannot wait for thorough cardiac evaluation and possible revascularization. The next step is determining the risk of the procedure being performed. For most otolaryngology cases, the risk will be low to intermediate as the high-risk category is generally reserved for vascular operations. Once these steps are completed, the patient’s current functional status and symptoms as well as past medical history are utilized to determine the need for further preoperative cardiac assessment, such as stress testing and potential referral for formal cardiology evaluation.
The algorithm utilizes five clinical risk factors—history of ischemic heart disease, prior or compensated heart failure, diabetes mellitus, chronic kidney disease, and cerebral vascular disease—to identify and stratify a patient’s risk for cardiac complications. In addition, any symptoms of active myocardial ischemia, heart arrhythmia, valvular heart disease, or decompensated heart failure should prompt a formal cardiology referral. Per the ACC/AHA guidelines, an ECG should be obtained in all patients with a history of coronary artery disease, peripheral vascular disease, or congestive heart failure who are undergoing head and neck surgery. Currently, there is no consensus on minimum age at which an ECG should be routinely obtained. If an abnormality is identified on ECG, then this would also prompt referral to a cardiology subspecialist for further evaluation.
Perioperative beta-blockade has been shown to reduce the incidence of perioperative cardiac risk in patients with any of the five clinical risk factors listed in the prior paragraph. Beta-blockade should be considered in these higher risk patients even in emergent operations. Usually patients with chronic medical conditions that predispose them to heart disease will have a primary internal medicine
physician who can assist in the decision-making process when the operation is done on an elective basis.
After the cardiac assessment, the next most important factor in preoperative management is pulmonary evaluation. Patients with a history of restrictive or obstructive pulmonary disease, long-term smokers, oxygen-dependent patients, and/or a recent history of upper respiratory infection need further pulmonary workup. Pulmonary studies including a chest x-ray, arterial blood gas, or pulmonary function testing are examples of routine tests required for preoperative risk assessment and management. Often patients with chronic lung disease will need detailed evaluation and recommendations for perioperative management from a pulmonary subspecialist (
3).
Renal and hepatic function also affect perioperative patient management and risk. The clearance of medications from the body is nearly always affected by either renal or hepatic function. Therefore, both should be assessed with careful history and laboratory assessment as indicated to appropriately choose and dose perioperative medications including antibiotics, beta-blockers, sedatives, and analgesics. Patients with asymptomatic elevations in liver-associated enzymes often can proceed to surgery without delay. However, patients with active hepatitis or cirrhosis do have an increased risk of postoperative complications and mortality, which may require postponement of surgery and/or aggressive preoperative planning for risk reduction (
4). Hepatic dysfunction alone can be an independent risk factor for perioperative morbidity and mortality, especially in patients undergoing high-risk operations. Bleeding complications are increased due to the propensity for coagulopathy from decreased liver synthetic function and thrombocytopenia from splenic sequestration associated with severe liver disease. Head and neck operations are considered low to intermediate risk, and the studies that have defined perioperative risk include few head and neck operations (
5). One study limited to the evaluation of perioperative risk in otolaryngology cases found a history of hepatitis was associated with complications, but only five patients with hepatitis or a history of hepatitis were included in the analysis (
6). Another recent study found no statistically significant increase in overall flap complications in patients with hepatic dysfunction although there was an increase in incidence of postoperative flap hematoma (
7).
Perioperative medication management is essential even in the absence of renal or hepatic impairment. A complete medication review including over-the-counter and herbal supplements is important not only to assess a patient’s known comorbidities but also to prevent intra- and post-operative complications. In general, most chronic medications can be taken with a glass of water the morning of the operation. Common exceptions to this rule include oral hypoglycemic medications, chronic anticoagulation, diuretics, and nonstatin hypolipidemics. However, the risk and benefit for continuing each individual medication should be addressed preoperatively. Type I and II diabetic patients on chronic insulin therapy will need to develop a perioperative plan with their primary physicians or endocrinologists especially for longer, more complex operations.
Anticoagulation and antiplatelet therapy alone can involve significant preoperative planning and execution. The indication for anticoagulation is important for devising a plan for perioperative management. For instance, if a patient is taking anticoagulation for the treatment of acute venous thromboembolic (VTE) disease or has a mechanical heart valve, it is much more important to maintain therapeutic anticoagulation throughout the perioperative period than if a patient is taking anticoagulation for prevention of VTE, in patients with a remote history of cere-brovascular accident, or in patients with atrial fibrillation. Antiplatelet therapy planning is likewise dependent on the reason for use. In most cases, antiplatelet therapy will be discontinued due to operative bleeding risk. Exceptions are when bleeding risk is minimal or discontinuation will cause a life-threatening complication, that is, coronary artery stent thrombosis.
INFORMED CONSENT
Consent is the process of obtaining permission to perform a surgical procedure after thoroughly informing the patient about all aspects of the procedure. Consent is typically obtained from the patient on whom the procedure will be performed; however, should the patient in need of surgery be unable to provide consent, the next of kin or legal guardian can provide consent. Examples of the types of patients who are unable to personally give consent are not limited to the following: patients under the age of 18, patients who are intubated and/or sedated, and patients with mental health problems or mental handicaps. Patients giving consent must have decision-making capabilities.
The consent must state in layman’s terms the procedure that is to be performed as well as the risks, benefits, and alternatives. Risks of the surgical procedure, including possible complications, should be discussed with the patient. Benefits of the procedure should also be made clear to the patient. Alternatives to the procedure should be reviewed and it should be clarified that the alternative to refuse surgery is the patient’s ultimate choice. In acquiring consent, the patient must understand his or her disease process, the goals of the procedure, and possible outcomes.
UNIVERSAL PRECAUTIONS
In 1987, the Centers for Disease Control (CDC) published a report on the prevention of blood-borne pathogen transmission in the world of health care. This document, in comparison to a similar report by the CDC in 1983, made recommendations for health care workers, which would eventually become known as “Universal Precautions.” This
new report highlighted the importance of consistent use of body fluid precautions regardless of the patient’s bloodborne infection status. It was wisely felt that the patients’ accurate infection status was often unknown and therefore safest to implement universal precautions.
The CDC recommends the use of gloves, barrier gowns, and mucous membrane barriers, including eye protection and masks, when there is contact with body fluids or blood. Gloves are to be worn by the health care worker any time there is contact with blood or body fluids and must be changed after contact with each patient. Gowns should be donned any time a splash of blood or body fluids is expected, especially during procedures. Mucous membrane barriers, masks and eye protection, should also be worn if a splash is expected in order to prevent exposure to the eyes, nose, or mouth.